Rajashree Srinivasan
![]()
30: Pediatric Traumatic Brain Injury
![]()
PATIENT CARE
GOALS
Evaluate and develop a comprehensive rehabilitative plan of care for the pediatric patient with traumatic brain injury (TBI) that is compassionate, appropriate, and effective for the treatment and management of TBI problems and the promotion of health.
OBJECTIVES
1. Describe the key elements of the history and pertinent physical examination of the child with TBI.
2. Describe the key impairments, functional and activity limitations, and participation restrictions in the child with TBI.
3. Describe the psychosocial and vocational implications in the child with TBI and strategies to address them.
4. Describe the impact of TBI on the school-age child in school and community activity.
5. Describe the long-term consequences of pediatric TBI.
6. Describe potential injuries associated with pediatric TBI.
7. Describe the key components of a rehabilitation or treatment plan for the child with TBI.
First, an evaluation is done by the medical team involved in the care of the child. The child’s complete medical history—current and past—is obtained from the caregivers. Sometimes, the history may have to be obtained from the medical records as caregivers may not be available, as in the cases of nonaccidental TBI or associated fatalities. The detailed history is followed by a physical examination. The details of the history that the physician should focus on are included in Table 30.1.
Children in distress are naturally apprehensive of strangers. Therefore, it is important to initially observe the child before performing a hands-on examination. Newborns show spontaneous mass movement patterns. A child who is in pain or afraid may not demonstrate a normal movement pattern. Instead, he or she may just lie on the bed or show abnormal patterns of movement when compensating for pain (e.g., antalgic gait pattern when ambulating, guarding a limb when performing bimanual activities). A child in a coma will not interact with the environment. Reflex movements may sometimes be mistaken for purposeful responses to stimulus. It is important to distinguish this with a thorough and consistent examination. These children may need to be examined either on the bed or on the parent’s lap. Initial observation is followed by a hands-on examination, performed at the end of the evaluation to minimize the distress associated with the procedure.
The physical examination should be thorough, complete, and cephalocaudal; the physician should have a set blueprint in performing it, so every aspect is addressed. The vitals are documented to ensure stability prior to starting therapies. Documentation of weight-bearing status and use of prophylaxis for deep vein thrombosis when applicable is important. It is also important to document if the child is in a coma, using the Ranchos Los Amigos Scale or the Rappaport Scale. The head and neck examination is followed by detailed examinations of the cardiorespiratory system, abdomen, and central nervous system. Skin examination should document any rashes, breakdown, or wounds/sutures/staples. It is important to document when the sutures/staples have to be removed. If a tracheostomy is present, the physician should note its size and take care to ensure that a spare is present at the patient’s bedside. Gastrostomy sites should be examined to determine if there is any leakage, skin irritation, or signs of infection.
In the ICU setting, as the focus is on ensuring medical stability, range of motion can be performed; the physician should also monitor heart rate and note any signs of distress. The child can be placed in splints/positioning braces at the ankles and the wrists for proper positioning. Once in the rehabilitation setting, strength and sensory testing are performed, as well as evaluations for any early contracture formation. Also, it is important to evaluate for any occult fractures that may be missed or the presence of associated spinal cord injury. Associated amputations can complicate the rehabilitation process, particularly if the weight-bearing limb is the one that has non-weight-bearing restrictions.
Cognitive ability also plays an enormous role in the rehabilitative process. The child may not remember not to place any weight on the limb if there are any documented restrictions, and may require frequent cueing to maintain the non-weight-bearing status. The restrictions compound the impairments, both physically and cognitively, particularly if there are weight-bearing restrictions in an existing limb after amputation (depending on the level). Depending on the ability of the patient, he or she might sit up on the edge of the bed, or in a chair—if able to do so with adequate head and trunk control—providing assistance when necessary. Use of standing frames, tilt tables, wheelchairs for positioning and mobility, and development of skills is of paramount importance. Spasticity may interfere with these, requiring aggressive range of motion and providing splinting and orthoses, serial casting, and medications.
TABLE 30.1 History Taking-Points to Focus On
History of present illness | Modality of injury, motor vehicle accident, nonaccidental traumatic brain injury, all-terrain vehicle rollover, gunshot injuries, injury with sports; was the child adequately restrained—seat belt, car seat with restraints, time needed to extract; presence of drugs or alcohol; Glasgow Coma Scale, loss of consciousness, seizures at the scene, presence of posturing, presence of dirty wounds, additional wounds |
Medical and surgical history | Surgical procedures like intramedullary nailing, open reduction and internal fixation of fractures, wound debridements, sutures of lacerations, presence of any grafts, placement of any central lines, duration of placement of external ventricular drain, ventricular peritoneal drain, electrolyte abnormalities, presence of additional injuries, spinal cord injury, extremity fractures, liver and spleen lacerations, lung contusion |
Past medical history | History of brain injury; history of ADHD; developmental history; history of any allergies to medications; list of medications |
Social history/family history | Number of people in the family available to provide support to the family; any problems with behavioral issues in the family; any history of drug use in the family; the kind of house they live in; whether caregivers are physically capable of taking care of the child |
Review of systems | Focus on spasticity, decerebrate and decorticate posturing, dysphagia, dysautonomia, seizures, and weakness. Was there a history of infection? How long was the child on the ventilator? Did the child need to have a tracheostomy and was a gastrostomy tube placed? |
Autonomic dysfunction is an important complication of severe TBI. The incidence is 8% to 9.3%. The condition is caused by disruption of inhibitory activity from the brainstem. causing sympathetic outflow (1). It is usually triggered and exacerbated by any noxious stimuli like a full bladder, incomplete bowel evacuation, and spasticity, underlying infection, deep vein thrombosis, heterotopic ossification, or progressive hydrocephalus. Patients present with increased heart rate or blood pressure, tachypnea, hyperpyrexia, sweating episodes, and posturing. Addressing the underlying cause usually diminishes the symptoms. The presence of dysautonomia should be a cautious indicator when performing therapies.
Patients in a coma are usually evaluated based on their responsiveness to their surroundings. There are various scales used: Rappaport Scale, Ranchos Los Amigos Scale (Revised), Western Neuro Sensory Stimulation Profile, and the JFK Coma Recovery Scale (Revised), to name a few. The Glasgow Coma Scale (GCS) is unsuitable for use in the rehabilitation setting as it does not predict outcomes in brain injury or guide treatment.
Depending on the part of the brain injured, severity of the injury, and resulting complications, post-TBI effects are varied. The patients may continue in a persistent vegetative state, needing tracheostomy and gastrostomy support. They may continue to have tetraparesis, spasticity setting in, and contractures developing later. Improvements in physical conditions are varied, with complete physical recovery—including ability to ambulate to hemiparesis with a circumducted gait pattern—being seen. Spasticity may be persistent, affecting activities of daily living, positioning, and ambulation. These may be seen as long-term complications.
Associated dysfunctions in TBI include olfactory dysfunction (anosmia, a common consequence, seen with severe TBI). There is questionable association of anosmia with executive function. Hearing impairment may be due to central processing deficit, peripheral nerve damage, cochlear injury, or disruption of middle ear structures. Vertigo secondary to vestibular impairment resolves within 6 months of injury; however, electronystagmogram abnormalities can persist for years. Central auditory processing deficits are seen due to damage to tracts or cortical tissue. Normal pure tone audiometry is seen, but speech discrimination or late waveforms of brainstem auditory evoked potentials are abnormal. Conductive hearing loss is seen due to disruption of ossicles, or the presence of cerebrospinal fluid (CSF) or blood in the middle ear, which is associated with fractures of temporal bone. Conductive hearing loss resolves spontaneously in 3 weeks. If recovery is greater than 3 weeks (especially for 30 db), repeat audiogram and exploration of the middle ear are recommended. Fluid in the middle ear usually resolves spontaneously. Sensorineural hearing loss is noted at higher frequencies and associated with inner-ear pathology. Eighth cranial nerve pathology or injury to the labyrinthine capsule, or labyrinthine concussion, causes hearing loss because of transmission of high-energy vibrations and a pattern similar to hearing loss after prolonged exposure. Injuries to the labyrinthine capsule and eighth cranial nerve are associated with basilar skull fracture.
Visual impairments include visual acuity deficit as the most common deficit seen with frontal lobe injuries. Visual impairments may be associated with more severe neuropsychological impairments. Temporal lobe involvement causes visual memory impairment; parietal lobe involvement causes impairment of spatial awareness. Diplopia is due to extraocular muscle imbalance due to trochlear palsy, sixth nerve palsy, or difficulties with convergence seen due to supranuclear impairment (1). It is important to be vigilant about electrolyte imbalances and neuroendocrine dysfunctions like syndrome of inappropriate antidiuretic hormone secretion (SIADH), Diabetes Insipidus (DI), and cerebral salt wasting and address them as they arise.
Speech impediments may be seen in the form of dysarthria, word-finding problems, grammatical errors, or understanding social cues. This can complicate communication further, deepening the patient’s gorge of social isolation.
Neuropharmacologic agents are frequently used in the acute rehabilitation setting. Medications typically used are dopamine agonists like amantadine, methylphenidate, gamma-amino butyric acid (GABA), agonists like baclofen, and anticonvulsants like phenytoin and lamotrigine, to name a few (2). It is important to be able to identify side effects and adverse reactions.
Spasticity is defined as velocity-dependent resistance to stretch. Treatment of spasticity is based on whether function is affected, caregiving including hygiene becomes difficult, and positioning in bed and wheelchair is very difficult. It is measured by the Ashworth and Modified Ashworth Scales, and the Tardieu Scale. Range-of-motion exercises, stretching, and placement of orthoses are noninvasive methods of managing spasticity. Use of oral medications like baclofen and diazepam (GABA receptors), tizanidine (α1 antagonist), or dantrolene (acts on sarcoplasmic reticulum) should be monitored for side effects like sedation, abnormalities of liver enzyme, hypotension, and liver and renal dysfunctions. Use of dantrolene in the pediatric patient should be circumspect, prompting the physician to monitor liver function tests regularly. Chemodenervation with botulinum toxin injections or phenol injections has been shown to be helpful in reducing spasticity. Intrathecal baclofen (ITB) pump placement has been found to be extremely helpful in the day-to-day activities by managing spasticity efficiently. It should, however, be noted that ITB in children should be managed with care as children are dependent on the adult caregivers for regular maintenance. It is also important to emphasize the criticality of not refilling the ITB use in a timely fashion, as the result is far more life threatening and can result in death, stressing the also importance of proper education and proper selection of candidates for the placement. Selective dorsal root rhizotomy is a permanent surgical procedure used more often in children with cerebral palsy that has been found to be helpful in managing spasticity.
Table 30.2 provides a list of areas to monitor after brain injury.
Physical therapists focus on range of motion, stretching, strengthening of lower extremities, transfer and mobility training, ambulation and assistive devices needed for ambulation, evaluation of splints and adaptive equipment, and family training. Occupational therapists focus on evaluating activities of daily living like eating, brushing one’s teeth, toileting, bathing, dressing, and upper extremity range of motion, stretching, strengthening, evaluating for splints and assistive devices, cognitive screen, and family training. Occupational therapists also evaluate for visual, spatial, and perceptual deficits. Speech and language therapists evaluate swallow function, communication skills, thinking, and processing. If unsure of the swallow status of a patient, a bed swallow usually provides the answer until a modified barium swallow can be performed by the speech therapists. Neuropsychologists evaluate the patient’s ability to think and process information, determine impulse control, and determine the best strategy to facilitate learning.
TABLE 30.2 To Monitor After Brain Injury
AREAS TO MONITOR | INTERVENTIONS THAT CAN BE HELPFUL |
Spasticity/contractures | Timely management of spasticity either with range of motion, bracing, serial casting, medications, chemodenervation, or surgical options; once contractures set in, recognition of surgical options is needed to maximize function |
Aspiration pneumonia | Recognition of dysphagia to minimize risk of aspiration and educate families about the same; well-meaning families may feed their loved one under the mistaken impression of doing good |
Endocrine problems | Monitor for hypothyroidism by following up on TSH, free T4; monitor urine output, oral intake output where concerns of diabetes exist; depending on the location and severity of injury, important to monitor for hypopituitarism, DI, and SIADH; precocious puberty can be seen 2–17 months after initial injury |
Hydrocephalus | Change in neurological status, altered mental status, loss of bladder control; loss of balance should prompt a workup for hydrocephalus |
Pressure sores/fractures | Frequent turning, as well as monitoring skin with skin checks, can decrease the incidence of pressure sores from forming. Once developed, care focus should be on early resolution to prevent the worsening complications of infections, sepsis, and osteomyelitis |
Social isolation | Reintegration into school and community is important and should be achieved at the earliest moment possible. Return to school may depend upon the endurance level and may warrant starting off with half days and working up to full days. Community resources should be provided such as local brain injury chapters and so on. Physiatrists should familiarize themselves with the IDEA Act, ensuring education for all handicapped children (Pub law-94-142) |
One of the key components to coordinated care for the patient is the ability to provide a continuum of care. This spans inpatient and outpatient programs. Typically, inpatient programs provide therapies on a daily basis 5 to 6 times a week, particularly during the acute phase of recovery. Once the recovery plateaus off, or slow progress is seen, then outpatient therapies are set up. It is important for the outpatient therapists to have access to documentation to the inpatient progress as this provides a basis for future care. For instance, if the patient had performed certain activities during the inpatient stay that he or she is unable to replicate, then it may indicate either that the recovery has slowed off or a worsening neurological status needing further evaluation is present.
Brain injury is a leading cause of morbidity and mortality in children. The range of severity varies from concussion to persistent vegetative state (3). Despite improvements in care and rehabilitation, the impact of brain injury on children and their families is enormous with regard to finances and caregiver burden, to name a few factors. Children may be left with residual hemiparesis, speech deficits including dysarthria, aphasia, or behavioral problems, all of which impact the patient’s return to school and reintegration into the community. Schools can be preinformed about the limitations that a student has, so that they can be prepared for that child and make return to school as seamless as possible. An educational program can be provided to the patient, family, and school to help facilitate care and understand needs.
Children may recover with residual long-term complications of hemiparesis, vision deficits, spasticity, gait abnormality, behavioral problems, frontal disinhibition, attentional problems, problems with hearing, and cognitive delays.
Discharge disposition should be identified at the time of admission to ensure adequate training is complete by discharge. The process of discharging the patient begins at admission. Based on the recovery a patient makes, appropriate equipment is ordered. A wheelchair may need to be ordered on a rental basis for a child making rapid recovery. For a patient who is able to ambulate by the time of discharge, a wheelchair may be needed only for long distances for endurance. As spasticity evolves during the stay, it may be wiser to order orthoses closer to discharge as they may not fit well otherwise. The same principle also holds for ordering equipment for the patients.
MEDICAL KNOWLEDGE
GOALS
Demonstrate knowledge of differences in pediatric versus adult TBI, and established and evolving biomedical, clinical epidemiological, and sociobehavioral sciences pertaining to the field of pediatric TBI, as well as the application of this knowledge to guide patient-centered holistic care.
OBJECTIVES
1. Describe the pertinent anatomy, physiology, pathophysiology, and epidemiology relevant to pediatric TBI rehabilitation.
2. Identify developmental milestones that should be addressed to develop a successful rehabilitation program.
3. Describe the various diagnostic tests available in the care of children and adolescents with brain injury and their advantages and limitations.
4. Describe the fundamental principles that are relevant to the treatment of children and adolescents with brain injury.
Brain injury is the leading cause of death and disability in children and adolescents. In the United States, three TBIs occur every minute (4); 5.3 million people live with TBI-related disability. TBI costs Americans $76.5 billion in medical care, rehabilitation, and loss of work every year.
According to the CDC, the two age groups at greatest risk for TBI are ages 0 to 4 and 15 to 19 years. Among 0 to 19 years, 62,000 need hospitalization due to motor vehicle accidents, falls, sports injuries, physical abuse, and other causes; 564,000 children are seen in the emergency room for TBI and released. In children between 0 and 14 years, TBI causes 2,685 deaths, 37,000 hospitalizations, and 435,000 emergency department visits. Approximately 1,300. children in the United States experience severe or fatal head trauma from child abuse each year (5).
There are two age peaks for patients with TBI—one below age 5 and the other in mid to late adolescence. Incidence is higher in the males when compared to females (60%:40%). A history of preexisting attention deficit hyperactivity disorder is seen with a prevalence of 10% to 20%. Motor vehicle accidents are the commonest cause of TBI in adolescents at 66% and at 20% in children. Nonaccidental TBI is the cause of brain injury in 17% of infants and 5% of those between 1 and 4 years. Falls account for 39% of brain injury in children less than 14 years. Falls are the leading cause of injury in children less than 4 years. Association of other injuries, such as undetected fractures, is about 50% (1).
Brain injury differs in children when compared to adults. Brain development is a complex process starting in the third gestational week and continuing through early adulthood. Neurulation, proliferation, migration, dendritic development, synaptogenesis, differentiation, and apoptosis transform primitive neural tubes to a series of complex neural networks comprising the central nervous system (CNS) (6). The growing brain is more susceptible to insult and injury with long-lasting effects. Severity of injury, age at injury, and environment (social factors, family support, and interventions) impact recovery. Impact, as well as deceleration and rotational forces due to the large head, weak neck musculature, higher brain water content, and lack of myelination, contribute to the primary injury. The noted factors make it easier to transmit forces to deeper brain structures.
Primary injury includes blunt injury, gunshot wounds, contusions on the brain surface, and shear-type injury associated with deceleration and rotational forces. Primary injury is due to mechanical disruption of axons and membranes (1). Secondary injury occurs due to complications after the initial trauma (Table 30.3).
Diffuse swelling and second impact injury due to diffuse cerebral swelling occur more in children than adults. This is due to increased diffusion of excitotoxic neurotransmitters through the immature brain, with increased blood–brain barrier permeability after injury to the immature brain. Diffuse cerebral edema is associated with poor outcome. Cerebral blood flow varies with age—24 cm/s in healthy newborns, 97 cm/s in children 6 to 9 years, and then decreasing to adult value of 50 cm/s. Possible lower middle cerebral artery perfusion rate in children causes hypoperfusion. Second impact syndrome is due to repeated concussion in children and adolescents.
Causes | Hypotension, vasospasm, infarction, prolonged seizure activity, diffuse edema resulting in increased intracranial pressure, and decreased cerebral perfusion pressure |
Biochemical cascades involved | Cellular power failure, acidosis, overstimulation of excitatory neurotransmitter receptors, lipid membrane peroxidation, increase in intracellular calcium, and cellular damage by free radicals |
Nonaccidental TBI is characterized by a triad of subdural hemorrhage, retinal hemorrhage, and encephalopathy with an incompatible history of mechanism of injury. The history of mechanism of injury does not match the actual injury.
The Glasgow Outcome Scale is a functional outcome scale rating patients into death through vegetative state to recovery (Table 30.4).
Given how common TBI is in the pediatric population, it is important to be able to pay attention to the developmental aspects of rehabilitation. Developmental milestones are critical factors in the development of any rehabilitation program. It is imperative to take growth and development into account while devising any rehabilitation program in children. Infants who suffer nonaccidental TBI do not have the repertoire that older children and adults have to fall back on. For children who have been able to sit, stand, and walk, the rehabilitation program should include developing these skills. It is important to remember that children who have prior developmental delay will have more to work on to reach their baselines.
Primitive reflexes may resurface after a brain injury, causing difficulty in positioning and in therapies. It is important to know what the child was capable of prior to the injury to ensure proper goals are established. Developmental assessment is dependent on parental history. It is important to note if the child had the opportunity to learn the said skill, such as knowing body parts and colors in a 2-year-old. The rehabilitation goals should be individualized to each child and not necessarily based on protocols as each child is different.
Growth and development play a key role in the ever-changing face of brain injury. Not only do children lack the rich experiential knowledge an adult has, but they also have to assimilate the process of development and maturation while striving to achieve altered milestones. Deficits may not be apparent initially and present later as the child grows. This is particularly seen in infants who have suffered brain injury and may initially do well physically but later show cognitive and functional deficits.
Table 30.5 provides a list of tests that can be performed in the care of children with brain injury. It should be noted that this is by no means exhaustive as research is ongoing.
It is important to discuss the extent of the injury with the family so that they understand the intricacies involved in the care of the patient.
Access to proper health care is a desirable goal. Physicians must remember to do no harm in medicine. It is easy to get carried away in our quest for “proper care” of the patient. It is, however, important to remember to take the wishes/beliefs of the patient/family into consideration while making a recommendation. All of the information should be provided to the patient/family. For instance, if a procedure is associated with risk of more harm than benefit, then it should be discussed with the family/patient before being performed. The concept of beneficence should be inbuilt in patient care to ensure that the welfare of the patient is foremost. For example, it would be important to discuss the risks and benefits of performing an ITB pump placement in a patient with severe spasticity. The procedure is not without complications and carries the risks of anesthesia reaction, blood loss during surgery, malfunction of the pump, infection, overdosage or underdosage/withdrawal, and lack of commitment to follow up regularly for maintenance of the pump. These issues have to be discussed, along with an evaluation of the social situation; this includes the family’s ability (i.e., adequate transportation) and determination to keep appointments, as missing a refill can prove fatal.
Also, the limitations of the payer source should be taken into consideration, as the payer source may pay for the procedure and not for the ongoing maintenance of the pump, jeopardizing the patient’s life. It is also important to provide the family/patient with all the information prior to the procedure to enable an informed decision to be made, understanding that what we may recommend may be incongruous with family and patient values. Hence, the recommendations may not be accepted. It is important to be supportive to the patient/family in their autonomous decision. It is crucial to recognize the autonomy of the adolescent patient while addressing family issues as these may differ.
TBI impacts and challenges success in the school system, also affecting the social realm. It is important to educate parents and caregivers about the deficits and provide them with information and strategies on how this can be addressed. Pediatric rehabilitation of brain injury focuses not only on the medical and rehabilitation aspect, but also on the integration into schools and the community.
TABLE 30.4 Rating of Brain Injury Severity
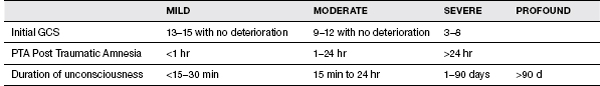
TABLE 30.5 Benefits and Limitations of Procedures in Brain Injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



