Fig. 12.1
Most common types of patellar tendon lesion: injury at the osteotendinous insertion (red line) and mid-substance injury (blue line)
12.3 Clinical and Diagnostic Examination
The first step in the diagnosis of a patellar tendon rupture is a good anamnesis. Typically, the patient refers an unexpected pain and subsequent knee impotence that can be sometimes associated to a fall, during a fast movement. The surgeon should ask for previous episodes of pain, in order to find a history of patellar tendinosis. Besides the attention should focus on other comorbidities or risk factors for patellar tendon ruptures (diabetes, rheumatoid arthritis, corticosteroid injection, etc.). At clinical inspection, the knee is usually swollen and, frequently, the patella cannot be recognized because of the edema. Palpating the knee, it is possible to evidence a defect in the patellar tendon and a patella alta, especially in complete breakings. Intraarticular hematoma is usually considerable and can be evacuated in emergency. The limit of the clinical inspection is the patients’ discomfort and pain during knee examination. In cases of partial patellar tendon ruptures, active extension may be possible with pain, but, in cases of complete tears, the surgeon should search for an extension leg sign. Besides, both passive and active and under opposition forces, extension strength should be evaluated.
In an emergency, it is important to exclude first a bone fracture and to analyze anatomical landmarks of the knee. A plain radiograph in two projections (anteroposterior and latero-lateral) has always to be done. A patellar avulsion, a patella alta or a tibial tuberosity fracture can be suggestive for extensor mechanism rupture. When there is suspicion of a patellar tendon rupture, it can be useful to perform an ultrasound scan (US) that can show a hypoechoic area within the proximal patellar tendon. The advantage of US is the possibility of a dynamic study of the lesion while flexing and extending the knee. The limitations of this diagnostic test are the subjectivity rendered by the physician performing the exam and the lack of reproducibility.
The gold standard for tendon rupture still remains MRI but it is considered to be more expensive and less available [24]. MRI sensibility is higher and has to be performed when the diagnosis is not fully clear; this happens more frequently in obese and very muscular patients. CT scan can be useful when suspecting a patellar avulsion to better visualize the amount of bone attached to the tendon, but it is not useful if a mid-substance lesion occurs.
In conclusion, ultrasonography may not be a reliable method in establishing the diagnosis of acute injuries to the extensor mechanism of the knee, particularly the quadriceps tendon ruptures in the obese and the very muscular patients.
12.4 Treatment Strategy
12.4.1 Acute Ruptures
Incomplete ruptures of the patellar tendon with intact function of the extensor apparatus may be treated nonoperatively. The period of immobilization in full extension has to be 2–3 weeks, followed by progressive range of motion with active flexion and extension for 4 weeks; strengthening has to be started after 6 weeks [11]. If the incomplete lesion is associated to functional deficits, or in cases of complete patellar tendon rupture, the surgical treatment is indicated regardless of age and physical activity. It should be performed as soon as possible: acute repair has the best chance to achieve a tension-free tendon apposition [7]. When treating acute patellar tendon injuries, isolated suture repair is generally not recommended because of the high rate of re-rupture. Most of lesions occur closed to the osteotendinous junctionalong the inferior pole of the patella: this localization facilitates transosseous sutures [25–27]. The surgical approach normally suggested for a patellar tendon repair is the anterior one with a midline incision. After a careful dissection, the peritenon is longitudinally split, the retinacular tears are dissected out, and the tendon ends are debrided. Then, the inferior pole of the patella, the most common site of injury, is decorticated with a curette or a burr to improve bleeding. This is made in order to improve the healing process. A pair of continuous, locking heavy (No. 2 or 5) nonabsorbable sutures is then placed in the tendon using a Krackow or similar suture technique. Three parallel bone tunnels are drilled with a 2.5 mm drill from distal to proximal in the patella; a suture passer is used to pass the free suture ends in the bone tunnels, with the central one containing two sutures.
Some authors proposed to create the tunnels using an ACL tibial guide [28]. The suture ends are temporarily fixed to check patellar tracking and to avoid a patella infera. Once the correct position and tracking of the patella have been checked, the strands are tensioned with the knee fully extended to approximate the tendon to the inferior pole of the patella. The retinacula are now closed with an absorbable suture, and the knee is flexed at 90° to test the repair [11]. As well as for quadriceps tendon ruptures, suture anchors can be used for patellar tendon acute repair [29]. Some authors described a technique using three suture anchors incorporated into a six-stranded Krackow technique. Some authors concluded that this technique could result into a low-profile construct, with better recreation of the tendon’s insertion into the inferior pole of the patella. This minimizes the possibilities of loosening through bone tunnels and abnormal stress forces [30]. Other authors demonstrated that with suture anchors, compared to trans-patellar sutures, there were less gap formations after cyclic loading [31, 32]. If the rupture occurs in the mid-substance of the tendon and there is enough proximal and distal substance, it can be repaired with continuous locking stitches; a Krackow or similar repair can be used [33]. In these cases, bone tunnels can be used in the patella to hold the proximal fragment [9]. Alternatively, a neutralization nonabsorbable wire or heavy sutures can be placed transversely through the patella and through another bone tunnel in the proximal tibia; this technique have been used to provide additional stability to the primary repair [33, 34]. When the primary repair is tenuous, it can be augmented using different surgical techniques. McLaughlin et al. described a technique of primary repair augmented with a tension wire anchored to the patella [35]. Kasten et al. describe their results comparing an augmentation with a metal wire or a strenuous PDS one, reporting no differences in terms of clinical results [36]. Other authors described an augmentation using semitendinosus autograft, nonabsorbable vascular graft, or nonabsorbable tape [37–40]. The augmentation using semitendinosus or gracilis autograft is one of the most commonly described in literature. The tendon is isolated and stripped, maintaining its tibial insertion. A tibial tunnel is normally drilled from medial to lateral to the anterior tibial tuberosity, and the tendon is passed through it. A second tunnel is then drilled in the patella, and the tendon is passed through it from lateral to medial. At this point, the end of the tendon is sutured back to its tibial insertion with nonabsorbable stitches [41]. Figure 12.2 shows some steps of this technique. However, the need for an augmentation in primary patellar tendon repair is still debated in literature. Some authors demonstrated better biomechanical resistance in augmented repair; other clinical studies showed similar results in patients with or without augmentation during the primary repair [42–44].
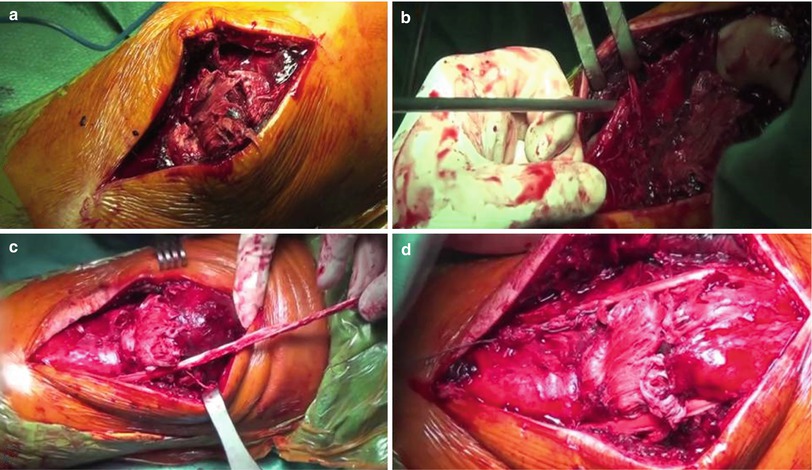
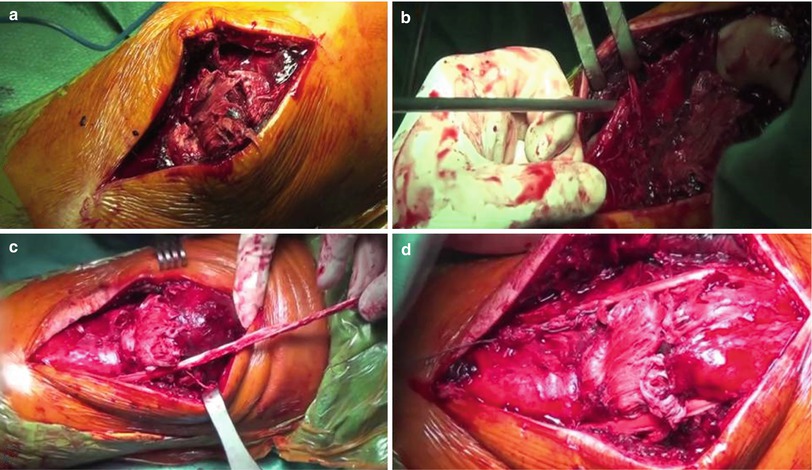
Fig. 12.2
Augmentation of patellar tendon rupture with semitendinosus tendon. (a) The osteotendinous insertion lesion. (b) Identification of the semitendinosus tendon and stripping, leaving the tibial insertion intact. (c) A tibial tunnel is drilled in from medial to lateral to the anterior tibial tuberosity, and the tendon is passed through it. Another tunnel is then drilled into the patella. (d) The tendon is passed through the second tunnel and then sutured back to the tibia with nonabsorbable stitches
12.4.2 Chronic Ruptures
In the chronic setting, primary repair is difficult because of tendon retraction, tendon quality, and adhesion formation [11]. Some authors described a primary repair with fascia lata or hamstrings augmentation; sometimes, reconstruction is the only surgical option [45, 46]. In chronic patellar tendon rupture or re-rupture, the hamstrings can be used with techniques similar to the one described for augmentation. The tendons are normally left inserted, the tibial tunnel is then drilled, and the tendons are passed all around the patella in a circular or figure-of-eight fashion and then sutured back to their insertion [47–50]. Some authors also described a percutaneous technique with good clinical results, but in a small case series [51]. Other authors described a technique using hamstrings passed through a longitudinal bone tunnel and then fixed to the superior pole of the patella with an Endobutton® (Smith & Nephew) [52]. However, in cases of chronic rupture, the augmentation is always suggested, even in cases in which a primary repair is possible.
Some authors suggest the use of the contralateral central third of the patellar tendon with proximal and distal bone plugs for the reconstruction of chronic patellar tendon rupture [7, 53]. Wiegand et al. proposed their technique using a Y-shaped flap folded back from the vastus lateralis fascia with good clinical and functional results [54]. Recently, different surgical techniques have been proposed using allograft tissue in patellar tendon reconstruction. Probably, the most commonly used allograft is the Achilles tendon [55]. The bone plugs of the allograft are normally fixed to the tibial tubercle after a squared trench is performed. The tendon is split into three parts: the central one is passed through a longitudinal patellar tunnel and sutured to the superior pole of the patella, and the other two parts are sutured to the lateral and medial retinaculum with nonabsorbable stitches.
In chronic settings, also synthetic grafts have been used. Naim et al. in a case report described a surgical technique using LARS ligament for the reconstruction of a patellar chronic tendon rupture in a low-demand patient [56]. However, because of the low biological profile of synthetic grafts, they are normally indicated in low-demanding patients.
12.5 Outcome
Outcomes following patellar tendon repair or reconstruction are favorable. Siwek and Rao in 1981 reported good results in 80 % of patients treated with acute patellar tendon rupture repair using sutures augmented with a Steinmann [45].
Dejour et al. were the first to report on using contralateral patellar ligament for chronic patellar tendon reconstruction, with good results on 13 patients at 8.6 months of follow-up [57]. Hsu et al. examined 35 patients treated with primary repair associated to a neutralization wire. Using the same criteria proposed by Siwek and Rao, there were 57 % of excellent outcomes, without any re-rupture [33]. Marder and Timmerman reported on 14 patients treated with primary repair without augmentation with 86 % of excellent results allowing them to resume their previous activity [44]. Kasten et al. compared two different augmentations after a direct suture of the tendon: the first using a wire cerclage and the second with PDS. They concluded that both the techniques were reliable and demonstrated good intermediate to long-term results [36].
Bhargava et al. reported good results with an average range of motion (ROM) of 1,378° in patients treated with repair and cerclage augmentation [58]. Ramseier et al. showed no differences in terms of muscle strength between injured and uninjured leg in a series of 19 cases of acute patellar tendon ruptures [26]. Bushnell et al. described their technique using suture anchors in 14 cases to repair acute patellar tendon lesion, with good or excellent results in 11 patients [27]. West et al. reported on 30 patellar tendons in which they perform a primary repair augmented with a nonabsorbable suture and early postoperative mobilization, with the patients reaching their pre-injury activity level in 6 months [59]. Massoud et al. described a new reinforcement suture called “suture line tension-regulating suture,” with the aim to reduce forces on the primary suture using an absorbable device. They reported good results using this technique, with good ROM and Insall-Salvati ratio [60]. In 2013, Wiegand et al. described a new technique for chronic patellar tendon rupture using a Y-shaped flap folded back from the vastus lateralis fascia. The authors reported good physical and ultrasound healing, with increasing in the mean Knee Society pain and function scores as well as the average ROM [54]. Maffulli et al. in 2013 described their surgical technique in which they performed an autologous ipsilateral hamstring tendon reconstruction for the management of chronic patellar tendon rupture. The authors concluded that all patients returned to their pre-activity level, and 14 out of 16 patients were very satisfied with the procedure [48].
Recently, Jain et al. described a percutaneous technique using semitendinosus tendon for reconstruction of chronic patellar tendon rupture, with all patients showing quadriceps strength 80 % or more compared to the contralateral leg.
In conclusion, in literature small case series of different techniques for both acute and chronic patellar tendon rupture are reported; in most of the cases, the authors described good results, without significant differences between the techniques.
Table 12.1 briefly describes the case series reported on literature.
Table 12.1
Brief description of the case series reported on literature with their results
Author | Year | Number | Median age (range) | Median follow-up | Technique | Results |
|---|---|---|---|---|---|---|
Siwek [45] | 1981 | 31 patients (25 acute/6 chronic) | <40 years | 2–11 years | Acute: Bunnell pull-out wire augmented with a Steinman | Acute repair: 20 excellent results, 4 good, and 1 re-rupture |
Chronic: initially treated with traction | Chronic repair: 2 excellent results, 3 good, and 1 unsatisfactory result | |||||
Dejour [57] | 1992 | 13 (chronic) | Not reported | 8.6 months | Contralateral bone-patellar-bone tendon | Correction of the extensor lag in all the cases and mean postoperative flexion of 91° |
Hsu [33] | 1994 | 35 patients (all acute) | Not reported | Not reported | Primary repair with a neutralization wire | 57 % of outcomes excellent; 28.6 % good; and 14.2 % unsatisfactory. No re-rupture of the tendon |
Marder [44] | 1999 | 14 patients (acute) | 33 years | 2.6 years | Primary repair with Krackow and patella tunnels | 86 % excellent results with patients resuming their previous activity level |
Kasten [36] | 2001 | 32 patients | Not reported | 8.1 years (1–18) | End-to-end suture augmented with wire cerclage or PDS | 2 of 22 patients had an extension lag in group A (wire cerclage) compared with no extension lag in group B (PDS cerclage). Average flexion in group |
A was 130° (SD 29°) compared with 137° (SD 12°) in group B. The average Hospital for Special Surgery Knee Score was 92 (SD 17) in group A and 96 (SD 12) in group B. Three patients were dissatisfied to determine whether this phenomenon can be reproduced | ||||||
Bhargava [58] | 2004 | 11 patients (acute) | 42 years | 26 months (14–38) | Suture repair of the patella tendon and retinacula protection by a cerclage wire | The mean Lysholm knee score at review was 97 (range 92–100). The mean Insall-Salvati measurement was 1 (range 0.95–1.1). No patients had fixed flexion deformities or demonstrated an extensor lag, and the average range of motion was 0–137°. Mean loss of power of 6 % (range 2–11) when measuring concentric extension and a mean loss of 7 % power in concentric flexion |
Ramseier [26]a | 2006 | 19 | 46.1 years | 57 months | Suture repair associated to McLaughlin cerclage | No difference between the range of motion and muscle strength when the injured leg was compared to the non-injured leg. Multiple injured patients had a significant reduction in muscle strength (p = 0.017) and circumference (p = 0.019); however, patient satisfaction did not differ from the non-multiple injured patient group |
Bushnell [27] | 2008 | 14 | 34 years
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




