Patellar Problems in Athletes
Jeffrey Halbrecht MD
The patella is the largest sesamoid bone in the human body.
Unlike most animals, humans often load the knee near full extension with the patella out of the confines of the trochlea and susceptible to instability.
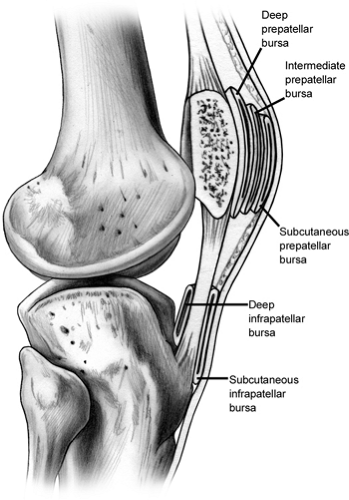
There are at least five bursas about the patella. The most clinically relevant is the subcutaneous prepatella bursa, which may become inflamed or infected.
The patella articular cartilage is usually close to 5 mm thick, making it the thickest cartilage in the body.
The medial patellofemoral ligament is the most important stabilizer of the patella to lateral translation.
The physical examination of the patella is the most important part of the diagnostic workup and is often performed improperly. The knee is a kinetic chain and forces on the patella can be dramatically affected by anatomic derangements or asymmetries proximal or distal to the knee.
There is evidence that bracing improves pain for patients with patellofemoral syndrome even if the brace does not appear to alter the biomechanical load on the patella.
The standard imaging evaluation of patients with patellofemoral symptoms will include an anteroposterior (AP), lateral, and a 45-degree tangential view of the patella. The lateral view is useful to evaluate for loose bodies, patella alta or baja, and will reveal the presence of early degenerative changes with inferior or superior patella osteophytes.
An acute dislocation of the patella is commonly confused with an anterior cruciate ligament (ACL) tear. The patient will present with a large hemarthrosis and will be tender to palpation along the medial retinaculum.
When surgery is selected as the treatment option for patella dislocation, initial arthroscopic evaluation is recommended to confirm the diagnosis and address any loose chondral or osteochondral fractures.
The treatment for recurring instability of the patella may differ from the treatment of an acute initial dislocation. Recurring instability may indicate a severe underlying anatomical dysplasia or predisposition that may require more aggressive treatment such as osteotomy of the tibial tubercle.
One of the most common causes of anterior knee pain is the patella compression syndrome. This syndrome refers to excess pressure along the lateral facet of the patella, usually associated with a tight lateral retinaculum and radiographic evidence of patella tilt.
Chondromalacia patients will present with pain, crepitus, and possibly a joint effusion. The history is usually that of insidious onset, although it may include a history of direct trauma such as a direct fall onto the patella or a blunt injury against a dashboard.
The patella is the largest sesamoid bone in the human body (1), and like other sesamoid bones, most likely evolved as a mechanism to protect the quadriceps tendon from abrasion and to improve distribution of forces across the tendon (2). In addition, the patella acts to improve the biomechanical leverage of the quadriceps during extension, acting as a fulcrum (3) with greatest effect seen at 20 degrees of flexion (4).
Most animal species load the knee in a flexed position and have a well stabilized patella maintained within the
confines of the trochlea throughout the range of motion. Humans, on the other hand, often load the knee near full extension with the patella out of the confines of the trochlea and are susceptible to instability. Interestingly, in greater apes the femoral diaphysis is straight and the trochlea is flat with no elevation of the lateral trochlea ridge and yet the patella remains stable due to the flexed angle of the knee in this species. In humans, the distal femur evolved into an obliquity angle of 8 to 10 degrees, necessitating the development of a deeper trochlea sulcus with an elevated lateral trochlear lip to stabilize the patella (5).
confines of the trochlea throughout the range of motion. Humans, on the other hand, often load the knee near full extension with the patella out of the confines of the trochlea and are susceptible to instability. Interestingly, in greater apes the femoral diaphysis is straight and the trochlea is flat with no elevation of the lateral trochlea ridge and yet the patella remains stable due to the flexed angle of the knee in this species. In humans, the distal femur evolved into an obliquity angle of 8 to 10 degrees, necessitating the development of a deeper trochlea sulcus with an elevated lateral trochlear lip to stabilize the patella (5).
Bursas
There are at least five bursas about the patella (Fig 40-1). The most commonly described is the subcutaneous prepatella bursa, which is the one that is most clinically relevant and may become inflamed or infected. The prepatellar tendon bursa can also rarely become clinically symptomatic. The intermediate and deep prepatellar bursa as well as the deep infrapatellar bursa are mostly just of anatomical interest. Recently, Dye et al. (6) have redescribed the three prepatella bursas as the prepatella subcutaneous bursa, the prepatella subfascial bursa, and prepatella sub aponeurotic bursa.
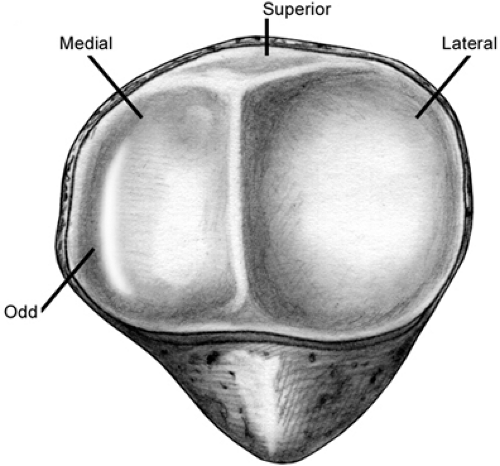
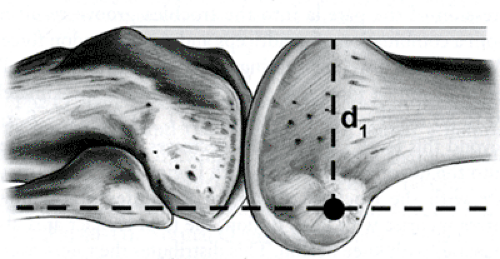
The typical patella is an asymmetrical sesamoid bone with a large flat lateral facet and a more sloped medial facet separated by the central ridge. A much smaller, more vertically shaped odd facet extends from the medial facet and makes contact with the medial trochlea only in maximum flexion (Fig 40-2).
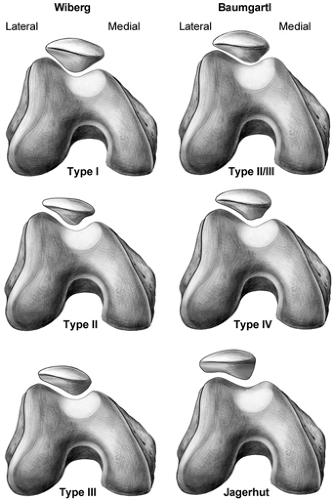
Different Shapes
Several authors have attempted to classify patella morphology into various shapes and types and correlate these types with the risk of patella chondromalacia and instability (Fig 40-3). Wiberg (7) has described three basic types, and Baumgartl (8) has added a fourth and fifth with patella shape progressing from symmetrical medial and lateral facets (Type 1) to a vertical medial facet and flat lateral facet (Type 5). The Wiberg Type 2 is felt to be the most common type according to Hennsge (9).
Ratio of Patella to Tendon
The height of the patella relative to the trochlea can have functional significance and is easily measured with a simple lateral radiograph. The normal patella position can be measured in various ways, most commonly by comparing the patella length to the patella tendon length (10) (Fig 40-4), although other methods have been described. A patella that sits too proximally, or patella alta, does not make as reliable contact with the trochlea and is often more mobile, resulting in an increased risk of instability. On the other hand, a low riding patella, or patella baja, can block knee flexion and place excessive loads on the patella, resulting in pain and progressive articular cartilage degeneration.
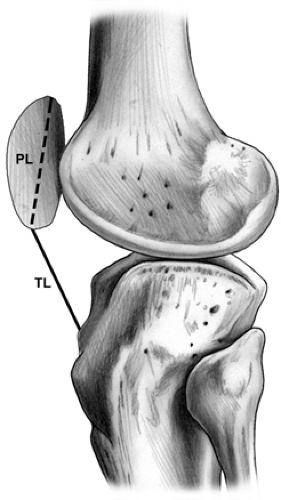 Fig 40-4. Measurement of patella position using the Insall-Salvati method. (From Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101; with permission) |
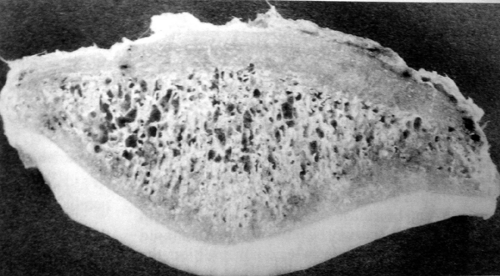
Cartilage Thickness
The patella articular cartilage is the thickest in the body and usually close to 5 mm thick (11). A recent study that carefully measured cartilage thickness of the patellofemoral (P/F) joint in 14 normal human knees using stereophotogrammetry and magnetic resonance imaging (MRI) revealed the average trochlea cartilage thickness to be 2.2 mm (+/-0.4) with a maximum of 3.7 mm, and the patella cartilage to be 3.3 mm (+/-0.6) with a maximum thickness of 4.6 mm (12) (Fig 40-5).
Patellofemoral Contact Forces
The main biomechanical function of the patella is to lengthen the extension moment arm of the knee at full extension (13) (Fig 40-6). Knee extension torque is the product of the quadriceps force multiplied by the length of the moment arm through which it acts. The patella shifts the quadriceps tendon anteriorly, increasing the length of the moment arm, and thus increasing knee extension torque.
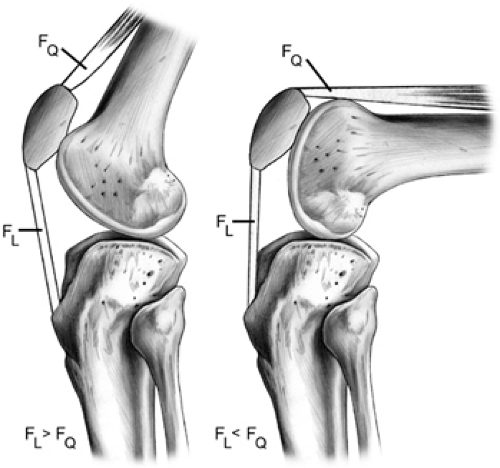
Although frequently described as a pulley, the patella has been shown to function more like a balance beam. Depending upon the degree of knee flexion, the patella is free to tilt. This results in a variable force on the quadriceps and patella tendons depending upon flexion angle. Thus unlike a
pulley, where the force on the patella tendon and quadriceps tendon would be equal, the force on the patella tendon is greater near extension, while the force on the quadriceps is greater with knee flexion (14,15) (Fig 40-7). This understanding is of great help in planning proper rehabilitation for injuries to the patella or quadriceps tendons.
pulley, where the force on the patella tendon and quadriceps tendon would be equal, the force on the patella tendon is greater near extension, while the force on the quadriceps is greater with knee flexion (14,15) (Fig 40-7). This understanding is of great help in planning proper rehabilitation for injuries to the patella or quadriceps tendons.
The location of contact forces across the patella also varies depending upon knee flexion angle. Due to patella tilt, as well as a shifting moment arm, the distal patella is loaded more in lesser degrees of knee flexion, and the proximal patella is loaded more at greater degrees of knee flexion (16). Due to changing lever arms, quadriceps force and patella tendon force also vary with knee flexion angle, with greater quadriceps force occurring at high flexion angles (Fig 40-8).
Patellofemoral compression force is the result of compression of the patella into the trochlea groove resulting from a combination of quadriceps and patella tendon forces. With standard weight bearing activities, maximum patella femoral contact force is thought to occur at approximately 70 to 80 degrees of knee flexion (17). As the knee flexes beyond this level, patella forces decreases as force is shifted onto the quadriceps tendon which begins to directly articulate with the trochlea. Although patellofemoral contact forces increase with knee flexion, the total contact area also increases with knee flexion. This distributes the forces over a greater contact area resulting in a less significant increase in force per sq mm, or contact pressure.
Patellofemoral contact force is generated by increased quadriceps torque. The quadriceps torque will increase based on the subject’s body weight and the distance of the center of the body mass from the center of the knee joint (torque = force × distance). This has important implications for understanding how patients with patella disorders compensate their body position during stair climbing in order to unload the patella (Fig 40-9).
Because patella pressure increases with knee flexion, the patella articular cartilage is thicker at its midpoint, where greatest contact pressure occurs.
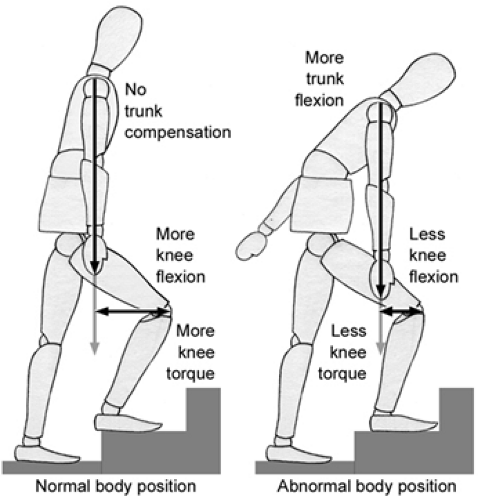 Fig 40-9. Patella femoral contact force is affected by body position, decreasing as patients forward flex at the hip during stair climbing. |
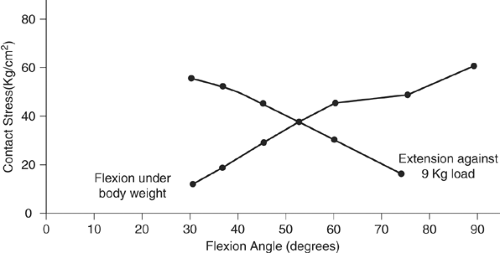 Fig 40-10. Patella femoral contact force increases four fold with leg extension exercises at 30 degrees. |
Until now, we have been discussing the biomechanics of normal weight bearing or closed chain activities. With knee extension (open chain) exercises, the patellofemoral contact forces actually increase with extension rather than flexion, due to the application of weight so far from the knee joint and the increase lever arm. The resulting large contact force over the relatively small contact area present during knee extension results in excessive patellofemoral contact pressure (force per unit area). Performing a knee extension exercise at 30 degrees of flexion using a 20 pound weight will result in pressure that is four times that present during physiological loading (15) (Fig 40-10).
Chondromalacia is thought to result from excessive patellofemoral contact pressure. After articular cartilage breakdown occurs, local contact pressure is reduced by up to 90%, resulting in concomitant increase in adjacent contact pressure of 90% (17). This may explain the often rapid progression of chondromalacia after it begins, and provides rationale for recommendation for activity modification for athletes with chondromalacia.
It is helpful to understand the relative patellofemoral forces associated with various activities. Various authors have evaluated these forces, with somewhat different conclusions based on experimental design. Reilly and Martens (18) showed that walking results in a PF force of 0.5 × body weight similar to straight leg raising (Table 40-1). Stair climbing results in a force of 3.3 × body weight, and squatting in a whopping 7.6 × body weight. More recent studies have suggested that squatting may only increase forces to 3 × body weight (4,17,19). Jogging increases PF force to 6 × BW (20) and jumping to 12 × BW (20a).
Patella tracking is dependent upon a multitude of anatomic factors. Static factors include bony anatomy and ligamentous structures. Dynamic factors include muscular interaction and change in anatomical relationships related to range of motion of the knee. Static bony anatomy that contributes to PF stability includes the depth and shape of the trochlea, the shape of the patella, femoral anteversion, and tibial rotation, along with the relative valgus alignment of the femoral-tibial articulation.
TABLE 40-1 Patellofemoral Forces Associated with Physical Activity | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
The Q angle is defined as the angle between the quadriceps mechanism and the patella tendon and is a helpful measure of patella tracking. The greater the anatomic valgus, or the greater external rotation present in the tibia, the larger the Q angle will be, resulting in laterally directed force vector (Fig 40-11). Normal Q angle is typically considered to be <15 degrees. Increased femoral anteversion will also result in a high Q angle by causing internal rotation of the femur relative to the tibia.
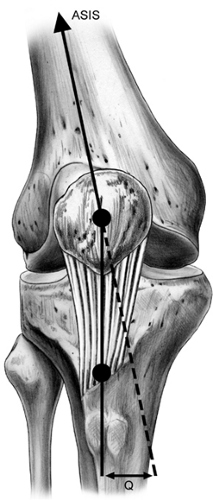 Fig 40-11. The Q angle is a helpful measure of patella tracking. There are differing opinions as to whether the Q angle is best measured in extension, 30 degrees, or 90 degrees of flexion. |
From full knee extension to approximately 20 degrees of flexion, the patella rests superior to the trochlea groove, and is stabilized by a combination of ligamentous and muscular forces. Patella stability at this point is determined by overall quadriceps tension, with medial sided stability contributed by Vastus Medialis Obliquos (VMO) contracture and medial patella femoral ligament tension, and lateral stability contributed by the lateral retinaculum. After approximately 25 degrees of flexion, the patella becomes engaged in the trochlea groove and stability is maintained by bony congruity with the trochlea.
Disruption or distortion of any of the anatomic factors previously mentioned can result in patellofemoral instability.
Trochlea Dysplasia
Trochlea dysplasia is felt to be a contributor to patella instability, but is often difficult to measure accurately. A recent MRI study showed a 100% sensitivity and a 96% specificity when a criteria of <3 mm trochlea depth was utilized as a measurement, done 3 cm above the femorotibial articulation (21). Trochlea dysplasia is rare, and even when present, does not usually require direct treatment. For patella instability associated with severe trochlea dysplasia, several procedures have been described to deepen the trochlea (trochleoplasty) including osteotomy and elevation of the lateral trochlea with bone grafting (22) or undermining and deepening of the trochlea groove (23). It is our experience that even in the presence of trochlea dysplasia, trochleoplasty is usually not necessary, and the vast majority of patella instability can be managed with either proximal soft tissue realignment, or osteotomy of the tibial tubercle
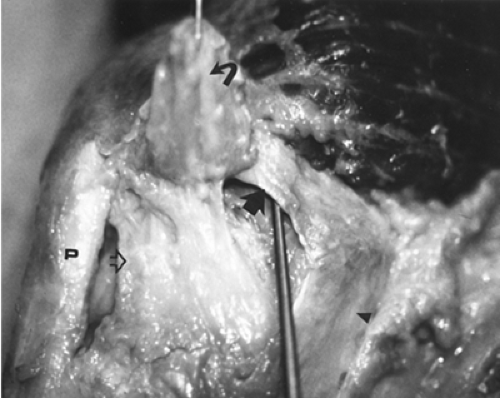
Medial Patellofemoral Ligament Insufficiency
Numerous studies have shown that the medial patellofemoral ligament (MPFL) is the most important stabilizer of the patella to lateral translation. Hautamaa et al. (24) showed in a cadaver biomechanical study that with serial sectioning, the MPFL contributes 50% of the patellofemoral stability (24) (Fig 40-12). In a similar study, Desio et al. (25) showed that the MPFL contributes 60% of the stability, with the medial patellomeniscal ligament contributing an additional 1%. Clinical studies on patients with patella dislocation also seem to confirm this finding, with both surgical and MRI evidence of disruption of the MPFL after patella dislocation (26,27,28).
Excessive Femoral Anteversion
An increase in femoral anteversion will result in relative external rotation of the tibia. This will result in an increase in the Q angle and a tendency toward lateral tracking of the patella. Correction of patella malalignment in this situation can theoretically be accomplished through a femoral osteotomy. Because of the obvious invasiveness and risks, however, this procedure is not recommended. Treatment is directed at the relative external rotation of the tibia by osteotomizing the tibial tubercle and moving it medially to decrease the Q angle.
Excessive Tibial External Rotation
Excessive external rotation of the tibia will result in lateral displacement of the tibial tubercle and an increased Q angle. When felt to be the cause of patella instability, this can be corrected by osteotomy and medialization of the tubercle.
Weak Vastus Medialis Obliquos
The VMO is a distinct muscle grouping of the vastus medialis that has a distinct nerve supply (29) and whose fibers insert into the superior medial aspect of the patella at approximately 65 degrees to the longitudinal axis (16). There can be anatomic variation on the insertion site to the patella. The more medial the insertion, the more of a medial stabilizing effect. A more superior insertion changes the force vector, providing less medial stabilizing force, and may be a contributor to lateral instability. Weakness of the VMO removes a significant dynamic stabilizing influence on the patella. Strengthening of this muscle is an important component of any rehabilitation program. The VMO contracts maximally in the terminal range of extension, and can be best strengthened with terminal, short-arc extension exercises.
Identifying the correct diagnosis is critical for the successful treatment of patella problems in the athlete. Typically, all patients complaining of anterior knee symptoms are lumped into a general category by physicians and therapists and treated with a standard, nonspecific, “patellofemoral” protocol. A careful history and physical examination is crucial before an effective focused and specific treatment plan can be initiated.
History
There are important questions that must be asked when evaluating a patient with anterior knee complaints. Important questions along with some common examples are presented as follows.
Location: Identifying the exact location of symptoms is critical. Inferior pain will suggest patella tendonitis, while proximal pain could indicate quadriceps tendonitis or a partial tear. Superficial pain may suggest prepatella bursitis, or bursal scarring, while deeper pain would suggest an intra-articular etiology such as chondromalacia, a chondral defect of the trochlea, osteochondritis dissecans (OCD) of the patella, or peripatella synovitis.
Sports History: What activities bring on symptoms? Pain with twisting activities would suggest possible patella instability; pain on stair climbing would suggest chronic myofascial pain [chondromalacia patella (CMP)], and pain with jumping sports would suggest patella tendonitis. Pain with kneeling might suggest prepatella bursitis.
Duration: Anterior knee pain since adolescence, particularly in a female athlete, would suggest a developmental tracking abnormality. Recent knee pain from a traumatic fall on the patella might suggest a patella chondral defect or occult fracture.
Timing of Symptoms: Occurs only during repetitive prolonged activity [plica, iliotibial band syndrome (ITBS)]; worse with prolonged sitting? (“movie sign”) (CMP); aggravated by stair climbing (CMP); pain immediately upon kneeling (prepatella bursa).
Past History: A past history of Osgood Schlatters could indicate residual pain from a persistent ossicle at the tibial tubercle. A history of previous patella dislocation might indicate the presence of a loose body, chondral injury, and of course persistent instability. A history of previous knee surgery might suggest painful scar tissue, catching/rubbing of adhesive bands, or scarring of the retropatella fat pad.
Occupation: Patients who work on their knees such as carpenters and carpet layers often develop prepatella scaring and chronic bursitis.
Trauma history: Try to elicit past history of seemingly unrelated trauma, such as fractures, leg length discrepancy (overload patella due to asymmetry); angular/rotational deformity (affecting patella alignment); chronic atrophy (weak quadriceps affects patella tracking), blunt trauma, thickened plica; scar; muscular injury (myositis, ossificans, chronic atrophy).
Sport-specific history: Has there been any change in the frequency or duration of sports activity, such as training errors (excessive increase in mileage causing overuse); recent decrease in sports activity causing atrophy; VMO weakness (any change in equipment used in the patient’s sport); new running shoes; change in playing/running surface (concrete vs wood or grass). Is the patient a bicycle rider (cleat position that affects knee rotation and bike frame/seat position that affects PF force); abrupt increased running distance, speed, times per week; or jumping sports, (think of patella tendonitis from overload) (Fig 40-13).
The physical examination of the patella is the most important part of the diagnostic workup and unfortunately is rarely performed properly. The first step in the proper evaluation of a patient with anterior knee complaints is to insist that they undress and put on a gown so that a complete examination of the lower extremities can be performed. The knee is a “kinetic chain” and forces on the patella can be dramatically affected by anatomic derangements or asymmetries proximal or distal to the knee.
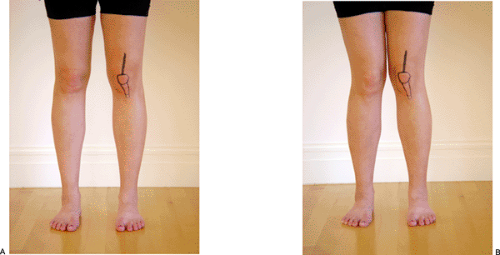
Standing Evaluation: Static
The patient must be asked to stand for the initial portion of the examination. Careful assessment of limb alignment and symmetry should be performed. This includes leg length assessment, pelvic balance, Q angle, varus-valgus alignment, knee recurvatum, flexion deformities, and foot position as it interacts with the floor during weight bearing (Fig 40-14).
Limb Length
Limb length asymmetry can lead to excessive force on the anterior knee and is a common source of knee pain in runners due to the repetitive loading involved in this sport. Studies indicate that an asymmetry of up to 1 cm may be normal, but even subtle amounts of asymmetry may lead to problems in runners.
Alignment
Increased valgus knee angulation results in an increase in Q angle and can result in increased pressure on the lateral patella facet. Excessive varus may lead to medial joint overload and possible medial patella plica irritation. ITBS may be more common due to increased tension on the lateral aspect of the knee.
Recurvatum may cause anterior mensical abutment syndrome which can cause pain just medical to the medial border of the patella tendon (30). In addition recurvatum may indicate generalized ligamentous laxity and suggest a patella tracking abnormality.
A flexion deformity causes the patella to be fixed in the trochlea even in the heel strike phase of running resulting in excessive P/F pressure and chondral breakdown.
Measure leg length by assessing pelvic symmetry. A leg length discrepancy will cause an elevated hemi pelvis, a secondary flexible scoliosis, and may be a cause of knee pain in repetitive loading sports, particularly running.
Foot Position: The Role of Orthotics in Treating Patellofemoral Syndrome
Pronation
Excessive pronation of the foot leads to increased valgus of the knee and is thought to be one of the reasons why hyperpronation can cause patellofemoral pain (31,32,33,34) (Fig 40-15). Authors have also suggested that prolonged pronation leads to external tibial rotation and thus increases the Q angle through this mechanism (33,34). To the contrary, however, other researchers believe that hyperpronation results in internal rotation of the tibia which would actually decrease the Q angle. Tiberio (35) has explained this discrepancy by suggesting that prolonged internal rotation of the tibia leads to compensatory internal rotation of the femur, which results in a secondary, relative increase in lateral tracking of the patella. This theory was also felt to be most plausible by Sims and Cavanagh (36). Another contributing factor is the effect of quadriceps activity during pronation. Electromyographic data show that the quadriceps begin contracting prior to heel strike and continue firing well into midstance, overlapping with the pronation phase of the gait cycle (37). The combination of the lateral tracking caused by pronation along with the increased patella compression associated with the increased quadriceps activity associated with the pronation phase of gait may best explain the deleterious effects of pronation in runners.
Use of Orthotics
Assuming that a relationship exists between excessive pronation and patellofemoral pain, the next controversy addresses the benefit of orthotics in controlling pronation and relieving patella femoral symptoms. A number of studies support the use of orthotics to alter lower extremity mechanics (38,39,40). James et al. (41) demonstrated that an orthosis corrects pronation in the injured foot to close to that of a normal foot without an orthosis.
Other studies have shown that mean pronation is reduced by a modest 2.5 degrees with the use of rigid orthotics, and only 1 to 2 degrees with semirigid devices (31,42,43,44). Soft orthotics may not alter maximal pronation at all (43), although other studies suggest that they do (45,46). Soft and semirigid orthotics may actually work by controlling maximal velocity of pronation rather than maximal degree of pronation (43). Although these studies suggest that correction of pronation is possible with an orthotic and that patella pain appears to be relieved by orthotic use in pronation runners, the complete scientific explanation for this effect is still lacking.
The scientific explanation for the association of pronation and patellofemoral pain remains vague; however, the clinical relationship of these two entities is supported by a number of studies.
Lutter (38) found that 77% of knee injuries in runners were associated with an abnormal foot position, of which 43% were hyperpronation. Of those runners with pronation related injuries, 28% had symptoms involving the patella, 15% had medial joint pain, and 57% had diffuse medial knee pain. Gross et al. (47) interviewed 347 runners of whom 12.6% had patellofemoral symptoms. Although data were not presented on the degree of pronation in these patients, 78% reported improvement of other with the use of orthotics. Similar benefits of orthotics have been reported by other authors (48).
More recent studies continue to support the benefit of orthotics to address patellofemoral pain (Fig 40-16). Gross and Foxworth (49) have suggested that patients with patellofemoral pain may benefit from foot orthoses if they
also demonstrate signs of excessive foot pronation and/or a lower-extremity alignment profile that includes excessive lower-extremity internal rotation during weight bearing and increased Q angle. The mechanism for foot orthoses having a positive effect on pain and function for these patients may include a reduction in internal rotation of the lower extremity; a reduction in Q angle; reduced laterally directed soft tissue forces from the patellar tendon, the quadriceps tendon, and the iliotibial band; and reduced patellofemoral contact pressures and altered patellofemoral contact pressure mapping. Kuhn et al. (50) have shown that custom flexible orthotics can correct the Q angle in male subjects with hyperpronation. Saxena and Haddad (51) found that 76% of patients with chondromalacia and patellofemoral syndrome had significant improvement in pain after treatment with semirigid orthotics.
also demonstrate signs of excessive foot pronation and/or a lower-extremity alignment profile that includes excessive lower-extremity internal rotation during weight bearing and increased Q angle. The mechanism for foot orthoses having a positive effect on pain and function for these patients may include a reduction in internal rotation of the lower extremity; a reduction in Q angle; reduced laterally directed soft tissue forces from the patellar tendon, the quadriceps tendon, and the iliotibial band; and reduced patellofemoral contact pressures and altered patellofemoral contact pressure mapping. Kuhn et al. (50) have shown that custom flexible orthotics can correct the Q angle in male subjects with hyperpronation. Saxena and Haddad (51) found that 76% of patients with chondromalacia and patellofemoral syndrome had significant improvement in pain after treatment with semirigid orthotics.
 Fig 40-16. Orthotics may benefit patients with a combination of foot pronation and patella femoral symptoms. |
In summary, there appears to be satisfactory evidence to implicate hyperpronation as a cause of patellofemoral pain; however, one needs to consider other causes of pain before attributing symptoms to pronation alone. In combination with other treatments, we support the judicious use of semirigid orthotics in hyperpronators to relieve patellofemoral pain, and we have had success in our own clinical practice with this approach.
The benefit of bracing for PF pain and instability is controversial; however, there appears to be good evidence that bracing improves pain for patients with patellofemoral syndrome, even if the brace does not appear to alter the biomechanical load on the patella (52) (Fig 40-17). Another elegant study using dynamic MRI imaging has shown that at least one type of patella brace can objectively improve patella tracking (53). Another interesting study showed that a patella brace could be used prophylactically to prevent patella pain in patients embarking on a rigorous training program (54).
Standing Evaluation: DYNAMIC
Single leg loading
Stresses P/F joint (Pain, crepitus)
Step up / step down
Several simple stress tests can be performed in the office to elicit PF symptoms and confirm a diagnosis of chondromalacia or PF compression syndrome. Have the patient stand on the affected leg and perform a single leg 30-degree knee bend with the examiners hand resting gently on the patella (Fig 40-18). In the presence of chondromalacia, crepitus will be audible as well as palpable. With PF compression syndrome, pain may be elicited with this maneuver in the absence of crepitus. Another version of this stress test is to have the patient step down slowly from a step stool. Eccentric loading of the trailing leg will usually result in pain and crepitus. Concentric loading with a step up maneuver is somewhat less reliable. Unlike meniscal pain, patellofemoral symptoms will usually decrease with deep squatting as the patella disengages from the trochlea in maximal flexion.
Seated Evaluation:
Active ROM
Seated Q angle
 Fig 40-18. Single leg loading is a good stress test for patella femoral compression syndrome and chondromalacia. |
Seated evaluation is performed next. Have the patient sit with their legs over the edge of the examination table. Measure the seated “Q” angle, which some authors find more reliable than in the supine position. Have the patient actively extend the knee and evaluate for a “J” sign (a terminal lateral tracking of the patella as the knee approaches full extension). Palpate the patella once again for crepitus with active knee extension. This may be caused by articular cartilage irregularity similar to the crepitus elicited during single knee loading, or occasionally by lateral compression and pinching of synovium between the patella and lateral trochlea edge, resulting in “synovial crepitus” and pain that is localized laterally. With the patient in the seated position, the examiner should passively flex and extend the knee while palpating along the edge of the medial femoral condyle to evaluate for a symptomatic painful plica (Fig 40-19).
Supine Evaluation: Passive
Inspection
Q angle
Swelling
Effusion
Old scars
Osgood Schlatters
Passive Rom (including hyperextension vs opp knee !!!)
Now have the patient lay supine. Measure the Q angle in this position. Measure leg length again from the anterior superior iliac spine (ASIS) to the medial mallelolus. Compare this to the standing assessment to determine if a true leg length discrepancy exists. Although standing assessment of leg length may be confused by associated scoliosis, muscular spasm, and posture, supine evaluation tends to eliminate the influence of these factors.
 Fig 40-19. Careful examination may reveal a thickened painful plica snapping over the edge of the medial femoral condyle. |
The knee should then be examined for a joint effusion. A fluid wave will indicate a small effusion (20 cc) while a bollatabel patella will suggest a more significant effusion (2,6,11,48,55,56,57,58,59,60,61).
Careful evaluation should be made of the prepatella tissues. Acute prepatella bursitis is easy to diagnose with swelling warmth and occasional erythema. A more subtle cause of prepatella symptoms may be due to scarring to the prepatella bursa resulting in thickened fibrous bands within the bursa that remain intermittently painful with direct loading activities such as kneeling.
Localized palpation should be performed over the bursa attempting to roll the thickened band under the examiner’s finger which will recreate the patient’s complaints.
The patella tendon is another source of potential pain and needs to be carefully evaluated. Inspection will usually reveal any evidence of old Osgood Schlatter’s syndrome with obvious prominence of the tibial tubercle. Tenderness over the tubercle and occasionally a mobile painful ossicle will confirm the diagnosis (Fig 40-20). Although most adults are not symptomatic from this entity, occasionally an old ossicle can reactivate and become symptomatic and needs to be kept in the differential of patella pain.
Patella tendonitis is best evaluated in the supine position. With the quadriceps relaxed, the examiner displaces the
patella distally delivering the inferior pole of the patella to more direct examination. Direct palpation over the inferior pole of the patella will cause exquisite tenderness in patients with patella tendonitis. The findings must be compared to the opposite knee, however, because some discomfort during this maneuver is normal. A similar examination can be performed on the superior pole of the patella to rule out the much less common quadriceps tendonitis. In this case, the examiner displaces the patella proximally and palpates along the superior border of the patella.
patella distally delivering the inferior pole of the patella to more direct examination. Direct palpation over the inferior pole of the patella will cause exquisite tenderness in patients with patella tendonitis. The findings must be compared to the opposite knee, however, because some discomfort during this maneuver is normal. A similar examination can be performed on the superior pole of the patella to rule out the much less common quadriceps tendonitis. In this case, the examiner displaces the patella proximally and palpates along the superior border of the patella.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree