High Tibial Osteotomy
Tim Spalding MB, BS, FRCS Orth
Price A.M. Gallie MB, BS, FRACS
High tibial osteotomy remains one of the important options for surgical treatment of knee malalignment and angular deformity about the knee.
Indications for surgery fall into two main groups: (a) for unloading a compartment suffering from early degenerative change, and (b) for controlling instability of the knee resulting from specific ligamentous laxities.
The goal of osteotomy is to relieve pain, to improve function, and to slow down the degenerative process.
Patients older than 60 years would be considered candidates for knee replacement, whereas patients younger than 50 years would be better suited for osteotomy with the intention of “buying time” before knee replacement is required. For patients between 50 and 60 years, a decision has to be made based on activity level, expectations, and degree of degeneration.
A variety of fixation systems are commercially available for opening-wedge valgus high tibial osteotomy. All procedures, however, involve the same principles of exposure of the upper medial tibia; creation and opening of a controlled, incomplete osteotomy above the level of the tibial tuberosity while protecting posterior structures; and previous insertion of a plate-fixation device.
The principle of closing-wedge osteotomy is to remove an appropriately sized wedge from the lateral aspect of the tibia above the tibial tubercle and to obtain accurate apposition of the bony surfaces, achieving union with stable fixation.
The main advantages of opening-wedge osteotomy compared with closing-wedge osteotomy are as follows: (a) no damage to the proximal tibia fibular joint and peroneal nerve, (b) easier to perform two-plane osteotomy, (c) no opening of the anterior compartment of the leg, (d) no alteration in the shape of the upper tibia, and (e) ease of correction intraoperatively.
The disadvantages with respect to closing-wedge osteotomy are as follows: (a) use of a graft, (b) possible delayed union or nonunion of the osteotomy site, and (c) difficulty in managing large corrections.
A concern regarding total knee replacement (TKR) after osteotomy is the additional difficulty of the procedure associated with the previous surgery in obtaining both adequate exposure and optimal soft tissue balancing during total knee arthroplasty.
The main factors that affect outcome adversely are the following: (a) age older than 55 years, (b) extreme obesity, (c) lateral compartment osteoarthritis, (d) correction to less than 7 degrees valgus, not by (e) high adduction moment in walking, and (f) multiple previous operative procedures on the knee.
High tibial osteotomy remains one of the important options for surgical treatment of knee malalignment and angular deformity about the knee. The overall principle is to adjust the mechanical access of the lower limb such that the load is redistributed from one compartment to the other. High tibial osteotomy principally is indicated to correct varus alignment into valgus alignment, but it also can be used for the opposite correction. Indications for surgery fall into two main groups: (a) for unloading a compartment suffering from early degenerative change, and (b) for controlling instability of the knee resulting from specific ligamentous laxities.
Limb malalignment is recognized to accentuate the stress on the articular surface within the involved compartment, resulting in further loss of the articular surface cartilage and increased stress on the subchondral bone, leading in turn to further progressive increase in the degree of malalignment. The goal and aim of osteotomy is to relieve pain, to improve function, and to slow down the wear-and-tear degenerative process. This concept of buying time before possibly needing arthroplasty is an important issue that needs to be grasped by patients to justify the recovery period associated with osteotomy.
In addition to the basic principle of load distribution, recent reports have indicated that the quality of repair tissue after osteotomy can be influenced by combining osteotomy with cartilage repair surgery, including autologous chondrocyte transplantation, microfracture, or even meniscal transplant. The important aspects of the procedure of high tibial osteotomy include careful patient selection and assessment, accurate surgical technique to correct alignment, and prevention of complications.
This chapter outlines the biomechanical principles of osteotomy and correction of alignment in addition to the indications, surgical techniques, and current results of the two main procedures: (a) opening-wedge high tibial osteotomy and (b) closing-wedge high tibial osteotomy.
Valgus High Tibial Osteotomy for Medial Arthritis
Medial arthritis is the most common indication, with patients experiencing symptoms of medial compartment pain usually following earlier partial or total medial meniscectomy or chondral damage associated with chronic deficiency of the anterior cruciate ligament (ACL). Overload of the medial compartment also may result from malalignment caused by an extra-articular fracture malunion. Patients usually complain of localized, activity-related pain in the knee, usually described as pain felt on the medial aspect and radiating down the medial border of the tibia. Patients usually do not have patellofemoral symptoms, and range of movement generally is well maintained. The ideal indications for osteotomy in this group of patients are as follows: (a) age of 60 years or younger, (b) flexion to greater than 100 degrees with no significant loss of extension, and (c) low body mass index (i.e., <25).
The activity level of the patient is an important factor in deciding whether to perform osteotomy. Knee replacement has become an increasingly popular and successful procedure for management of arthritis in less active patients older than 60 years, in whom the knee arthroplastic implant would be expected to last from 20 to 25 years and, generally, outlive the patient. Patients older than 60 years who are particularly active or most patients younger than 60 years would be expected to require revision of a knee replacement, if performed, because of a higher frequency of problems involving loosening or failure of the polyethylene tibial surface. In general, patients older than 60 years would be considered candidates for knee replacement, either total or unicompartmental, whereas patients younger than 50 years would be better suited for osteotomy with the intention of buying time before requiring knee replacement. For patients between 50 and 60 years of age, a decision must be made depending on activity level, expectations, and degree of degeneration.
It also should be recognized that rehabilitation following knee arthroplasty is quicker than that following osteotomy; hence, patients older than 60 years may be better suited for a procedure with a shorter period of rehabilitation and, perhaps, more complete relief of pain than can occur with osteotomy (1). Patients who are obese are do less well following osteotomy, achieving lower activity levels and poorer outcomes. A further relative contraindication to tibial osteotomy is significant laxity of the lateral collateral ligament.
Posterolateral Corner Instability
Patients with injury to the posterior cruciate ligament (PCL) and posterolateral corner of the knee are at risk of developing symptoms of instability, especially with pre-existing physiological varus. The result is a lateral thrust to the knee on walking.
The terms double varus and triple varus (2,3,4,5) have been applied to the situation in which varus malalignment progresses over time following ACL deficiency in the physiologically varus knee or in which varus deformity follows medial arthrosis or medial meniscal injury. Progressive varus leads to stretching of the posterolateral structures, causing double varus, and with further time and repeated anterior translation of the tibia, stretching of the posterolateral structures occurs, leading to hyperextension and recurvatum (i.e., the so-called triple varus). In addition, the neuromuscular or proprioceptive control of the joint provided by the soft tissue structures may be lost when ligamentous disruption occurs. Loss of this control may then exacerbate the malalignment, leading to clinical symptoms of instability (2).
On its own, ligament repair and reconstruction has a low chance of success in controlling instability because of the persistence of deforming forces that stretch the lateral structures and repaired tissues. In this situation, osteotomy is indicated to reduce the lateral thrust, with the intention to shift the weight-bearing line from hip to ankle so that it passes through the lateral compartment. In this way, the knee, on heel strike, is pushed medially rather than laterally, reducing the symptom of instability. Any hyperextension can be corrected through the osteotomy by increasing the posterior slope of the tibia (discussed later in this chapter), which has the added benefit of helping to resist posterior translation forces on the tibia associated with PCL injury. It also is likely that with distraction by opening-wedge osteotomy some tightening of the lateral structures occurs, again helping to improve the laxity (2).
Patients who undergo this procedure generally are in the younger age group and more sporting, because injury usually follows sport or traffic accidents. Often, little evidence of degenerative change exists, and patients may well have experienced some benefit from using a brace, resisting the posterior and lateral thrust on walking.
The basis of osteotomy in the management of osteoarthritis around the knee is to correct the abnormal weight-bearing line or load-bearing line that passes from the center of the head of the femur to the center of the talus at the ankle joint (Fig 43.4-1). Limb malalignment is accepted as a cause of increased stress on damaged articular cartilage, leading to pain, progressive loss of articular cartilage, and increasing angular deformity around the knee.
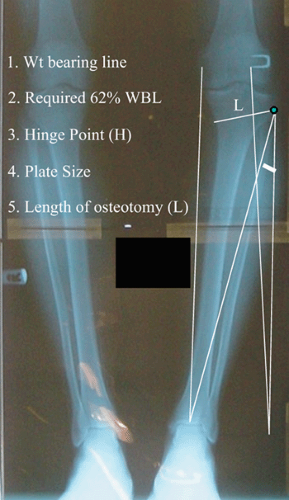
Brown and Amendola (6) reviewed the concept of radiographic evaluation and preoperative planning for high tibial osteotomy in an excellent article. In this article, the authors established how most recommendations point toward the same degree of correction. Confusion lies in the definition of the axes around the knee, and current figures of correction are based on the analysis of papers reporting good long-term results. In 1985, Coventry (7) recommended a correction of anatomical valgus to between 8 and 10 degrees (normal is 5 to 7 degrees). In 1987, Hernigou et al. (8) recommended correction to between 3 and 6 degrees of valgus mechanical axis (lateral angle between the center of the knee and the head of the femur and the center of the tibia at the knee and the center of the ankle; normal is 180 degrees). In 1992, Dugdale et al. (9) recommended correction of the weight-bearing line (center of the head of the femur to center of the talus) to a point from 62% to 66% of the position across the tibia from medial to lateral. The weight-bearing line is reported as a deviation from the center of the knee in millimeters or as a percentage of the tibial plateau width, with convention directing that the medial edge of the medial compartment is indicated as 0% and the lateral edge of the lateral compartment as 100%. The term weight-bearing line generally is preferred to avoid confusion with the other angular axes that are defined around the knee. When the indication for osteotomy is for hyperextension thrust, then the objective is to correct the alignment to neutral, with the weight-bearing line passing through the knee at 50% medial to lateral. The intention is to eliminate the abnormal thrust on walking, while realizing that it does not eliminate the static ligamentous laxity (10).
Miniaci et al. (11) reported a method for planning closing-wedge osteotomy without use of tracing paper or a template. His method (Fig 43.4-2) is modified for the opening-wedge osteotomy as follows:
The mechanical axis is drawn on the long leg alignment radiograph, passing from the center of the head of the femur to the center of the talus.
The required mechanical axis is drawn on the radiograph, passing from the center of the head of the femur through a point 62% from medial to lateral on the tibial plateau. This indicates the new position where the center of talus needs to be and is marked on the radiograph.
The hinge point on the lateral tibial cortex is marked, and a line is drawn from the hinge point to the new position on the talus as determined by the required mechanical weight-bearing line.
The line representing the “old” position from the hinge point to the current position of the talus is drawn.
The planned osteotomy is marked on the radiograph, and the length (L) is noted.
This length L is marked on the new line between the hinge point and the new position of the talus.
The height of the osteotomy plate used in the opening-wedge osteotomy is then measured using the two lines between the hinge point and the old ankle point and the new position of the talus.
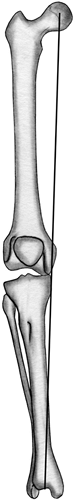 Fig 43.4-1. The weight-bearing line passes from the center of the femur to the center of the head of the talus at the ankle joint. |
The principle of an opening-wedge osteotomy is to perform an osteotomy from the medial side, above the level of the tibial tubercle, correcting the weight-bearing line through the knee while holding the osteotomy apart with a mechanical device either combined with or without bone graft. The methods of fixation include plate-and-screw fixation with or without synthetic, autogenous, or allogeneic bone graft; a technique involving hemicallotasis with external fixation; and application of an external frame with small-wire fixation devices.
Surgical Technique
A variety of fixation systems are commercially available, but all procedures involve the same principles of exposure of the upper medial tibia; creating and opening a controlled, incomplete osteotomy above the level of the tibial tuberosity while protecting posterior structures; and insertion of a plate-fixation device.
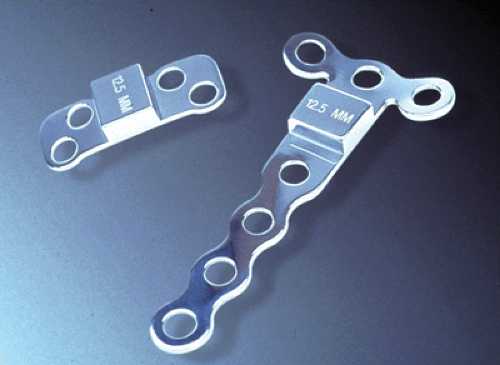
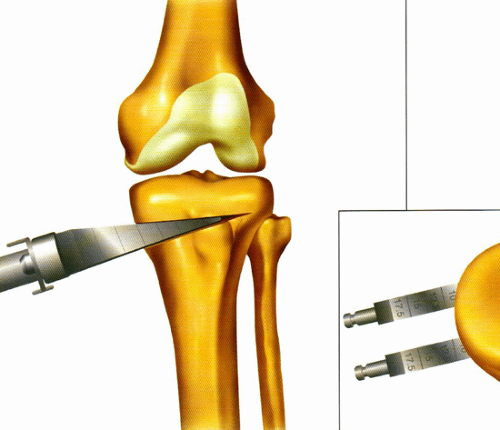
This section outlines the surgical technique using the Puddu plate-fixation device (Arthrex, Naples, FL) for the opening-wedge high tibial osteotomy (Fig 43.4-3) (12). The procedure is performed using tourniquet control on the upper thigh, and the leg is positioned supine on the operating table, with a foot bolster close to the foot such that the leg may be positioned in abduction and external rotation with the knee at 45 to 60 degrees, thereby exposing the upper medial border of the tibia at the level at the knee joint.
Before skin draping, the center of the head of femur is localized using fluoroscopy control and marked with a cardiac monitor dot. This can then be easily palpated through the drapes to reduce radiation exposure. It also is important to undertake tight bandaging of the foot and ankle during draping to allow easy palpation of the center of the ankle of joint.
A skin incision is made on the anterior medial aspect of the tibia halfway between the tibial tubercle and the posterior medial border of the tibia. The incision is taken from the joint line superiorly to a position from 6 to 8 cm inferiorly.
The tibial tubercle is identified, and a longitudinal incision is made just medial to the patella tendon, identifying the important landmark of the junction of patella tendon on the tibial tubercle. A transverse incision in the periosteum and superficial fibers of the medial collateral ligament is made, starting from the superior border of the tubercle (Fig 43.4-4). The periosteal elevator is then used to strip the tissue on the medial aspect of the tibia and around the posteromedial border, allowing insertion of a special, curved retractor to partially protect the vascular structures at the posterior aspect of the knee.
In this approach, the fibers of the deep medial collateral ligament remain attached to the tibia between this incision and the level of the joint line (Fig. 43.4-4). The superficial fibers of the medial collateral ligament, however, are divided down to bone.
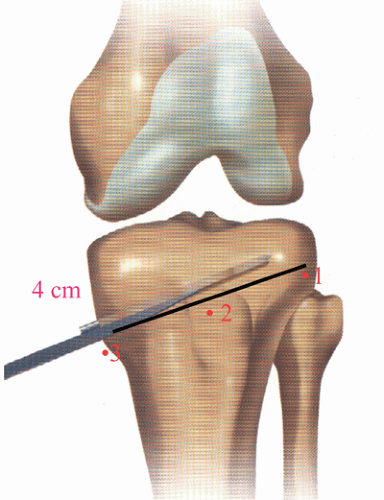
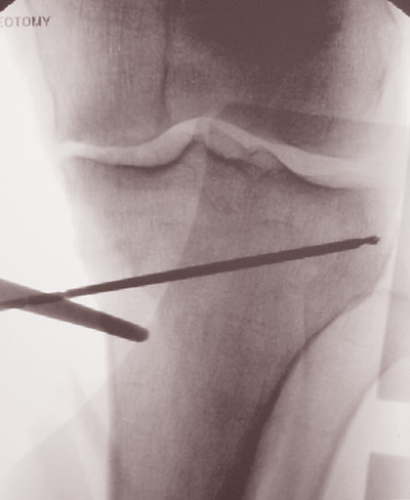
The guide pin for the osteotomy is then inserted freehand, with the position checked by radiography, with the goal for it to be passing just superior to the tibial tubercle ending approximately 15 to 20 mm below the lateral aspect of the tibial plateau. These landmarks are used in the preparation for passing the guide pin. A finger is placed on the head of fibula and a lever retractor placed under the patella tendon to identify the superior part of tibial tubercle. The extrapolation of a line between these two points determines
the start point for the guide wire, which usually is in the middle of the cleared space (Fig 43.4-5), approximately 4 cm below the joint line and midway from anterior to posterior. Take care to ensure that the head of fibula is in a normal anatomical relationship 10 to 15 mm below the joint line. In a patient with a high-lying fibular head, the articular portion of the superior tibiofibular joint usually remains 15 mm below the joint line, and this can be taken in to account during insertion of the wire.
the start point for the guide wire, which usually is in the middle of the cleared space (Fig 43.4-5), approximately 4 cm below the joint line and midway from anterior to posterior. Take care to ensure that the head of fibula is in a normal anatomical relationship 10 to 15 mm below the joint line. In a patient with a high-lying fibular head, the articular portion of the superior tibiofibular joint usually remains 15 mm below the joint line, and this can be taken in to account during insertion of the wire.
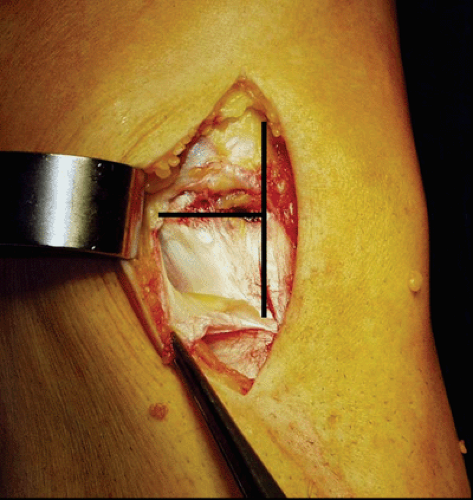 Fig 43.4-4. A transverse incision in the periosteum and superficial fibers of the medial collateral ligament. |
Once the wire is inserted, the knee is moved into a supine position. Then an image is taken to confirm the position, and the wire is adjusted as necessary (Fig 43.4-6).
Osteotomy with the oscillating saw is performed by inserting the saw to a depth of approximately 20 to 30 mm less than the measured length of the guide wire (Fig 43.4-7). It is important to ensure that the oscillating saw is inserted from true medial to lateral, avoiding the temptation to make the osteotomy from anteromedial to posterolateral. The osteotomy is progressed using the thin, sharp osteotome that is supplied with the instrumentation (Fig 43.4-8), again taking care to insert the osteotome from true medial to lateral. The position of the advancing osteotome is assessed by radiography, aiming to end 1 cm short of the lateral tibial cortex. At this point, gentle valgus stress is applied to the tibia, and an assessment of the degree of opening is made. The osteotome is advanced until a relatively easy opening of the medial side is visible on valgus stressing of the knee. As a guide, it should comfortably open between 2 and 3 mm with gentle stress so that the wedge opener, when inserted, will not lead to any propagation of the osteotomy toward the joint surface or into the superior tibiofibular joint.
The wedge opener is inserted and gently tapped into place, gradually increasing the opening of the osteotomy (Fig 43.4-9). Take care at this point to avoid heavy hammering,
because the sudden impact may lead to unpredictable propagation of the osteotomy.
because the sudden impact may lead to unpredictable propagation of the osteotomy.
 Fig 43.4-7. The oscillating saw is inserted to a depth of approximately 20 to 30 mm less than the measured length of the guide wire. |
Once the osteotomy wedge opener is inserted to the point predicted by preoperative planning, the long leg alignment rod is applied from the palpable cardiac monitor dot marker over the hip joint to the center of the talus. Fine adjustments are then made to the wedge opener, allowing accurate positioning of the new weight-bearing line at a point 62% from medial to lateral (Fig 43.4-10). This usually is halfway down the slope of the lateral tibial spine, which is very easily assessed on the fluroscopy screen.
Once the position has been found, the true height of opening is measured, and an appropriate plate is chosen, attached to a joystick, and inserted after removal of the handle of the wedge opener (Fig 43.4-11). If the tibial slope is thought to have been affected by the osteotomy, then a sloped Arthrex plate can be used to compensate. This is best judged by remembering that the height of the osteotomy at the level of the tibial tubercle should be half that of the opening of the medial cortex. If this is not the case, then either the osteotomy must be repositioned to a more posterior aspect on the medial side or an appropriately sloped plate must be chosen.
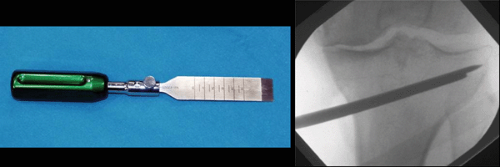 Fig 43.4-8. The thin, sharp osteotome is inserted to a position 1 cm short of the lateral tibial cortex. |
The plate is held in place using four screws. It is best to insert a proximal screw while the wedge opener is still in place to ensure stability of the construct. The opener is then removed, allowing contact of the cortex on to the stepped plate. This is important, because the bone needs to rest on the plate rather than on the screws.
The usual combination of screws is a 6.5-mm, fully threaded, cancellous screw in the proximal tibial metaphysis, with the screws aimed into the good-holding cancellous bone under the tibial spines. Two cortical screws (4.5 mm) are used to hold the lower part of the plate, aiming transversely across the tibia onto the opposite cortex (Fig 43.4-12).
If the space is 10 mm or greater, then a bone or synthetic graft is inserted into the open gap. This graft can be mixed with local bone graft harvested from the tibial metaphysis and diaphysis using a small osteotome. The final alignment position is confirmed by radiography, and the wound is closed over a single drain.
 Fig 43.4-10. With the osteotomy wedge opener in place, the long leg alignment rod is applied over the hip joint to the center of the talus.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|