Patellar instability is a common injury that can result in significant limitations of activity and long-term arthritis. There is a high risk of recurrence in patients and operative management is often indicated. Advances in the understanding of patellofemoral anatomy, such as knowledge about the medial patellofemoral ligament, tibial tubercle-trochlear groove distance, and trochlear dysplasia may allow improved surgical management of patellar instability. However, techniques such as MPFL reconstruction are technically demanding and may result in significant complication. The role of trochleoplasty remains unclear.
Key points
- •
Patellar instability is a common injury that can result in significant limitations of activity and long-term arthritis caused by recurrent injury.
- •
Recognition of the importance of bony alignment (tibial tubercle–trochlear groove distance), patella alta, trochlear dysplasia, and the femoral origin of the medial patellofemoral ligament (MPFL) is important.
- •
MPFL reconstruction requires precision in graft placement and minimal graft tension.
- •
Tibial tubercle osteotomy has a role in the treatment of bony malalignment and patellofemoral arthrosis.
- •
Trochleoplasty is a technically demanding procedure that involves potentially damage to articular cartilage and its role is still under investigation.
Introduction
Patellar instability is a common, debilitating injury that typically affects young active individuals, and can result in significant limitations of activity and long-term arthritis. As such, patellar instability is a significant cause of morbidity in society. In the past, a variety of different treatments have been tried with varying degrees of success. There have recently been substantial advances in the understanding of the pathophysiology of patellar instability. Additional treatments and techniques have been developed as a result of this better understanding and these advances seem to provide superior results for the management of this disorder.
Patellar dislocations account for approximately 3% of all knee injuries. The overall incidence is about 1 in 1000. Most patients who have patellar dislocations are young (aged 10–16 years) and female. The rate of recurrence varies widely in patients treated nonoperatively, but, taken as a whole, first-time dislocators have a low rate of subsequent dislocation. In patients who have had 2 dislocations, the risk of further injury is 50%. In patients with known medial patellofemoral ligament (MPFL) injury confirmed on magnetic resonance imaging (MRI), the rates of redislocation are even higher.
Instability of the patellofemoral joint is multifactorial in cause. Abnormalities resulting in instability include the osseous structure of the patella and trochlea, the overall limb alignment, the integrity of the surrounding soft tissues, systemic conditions affecting connective tissues, and the patient’s overall muscle tone.
Introduction
Patellar instability is a common, debilitating injury that typically affects young active individuals, and can result in significant limitations of activity and long-term arthritis. As such, patellar instability is a significant cause of morbidity in society. In the past, a variety of different treatments have been tried with varying degrees of success. There have recently been substantial advances in the understanding of the pathophysiology of patellar instability. Additional treatments and techniques have been developed as a result of this better understanding and these advances seem to provide superior results for the management of this disorder.
Patellar dislocations account for approximately 3% of all knee injuries. The overall incidence is about 1 in 1000. Most patients who have patellar dislocations are young (aged 10–16 years) and female. The rate of recurrence varies widely in patients treated nonoperatively, but, taken as a whole, first-time dislocators have a low rate of subsequent dislocation. In patients who have had 2 dislocations, the risk of further injury is 50%. In patients with known medial patellofemoral ligament (MPFL) injury confirmed on magnetic resonance imaging (MRI), the rates of redislocation are even higher.
Instability of the patellofemoral joint is multifactorial in cause. Abnormalities resulting in instability include the osseous structure of the patella and trochlea, the overall limb alignment, the integrity of the surrounding soft tissues, systemic conditions affecting connective tissues, and the patient’s overall muscle tone.
Anatomy and evaluation of the patellofemoral joint
Anatomy
The patellofemoral joint comprises the undersurface of the patella and the cartilaginous anterior surface of the distal femur, the trochlear groove. The patella is a sesamoid bone embedded within the tendon of the quadriceps that has a complex gliding articulation with the femur. The patella serves to increase the mechanical advantage of the muscle for knee extension while protecting the knee. The depth and steepness of the trochlear groove affects the inherent stability of the patellofemoral joint.
At 2 months of gestation the patellofemoral articulation is in its adult form with normal knee mechanics and range of motion at birth. With maturation, the cartilage on the undersurface of the patella thickens to 6 to 7 mm, the thickest chondral surface in the body. The undersurface of the patella is composed of 2 unique facets: the lateral facet is longer and less steep to match the lateral aspect of the trochlea. Most patellar articulation with the trochlear occurs between the lateral facet of the patella and the lateral trochlear groove, with the medial facet only contacting the trochlear in deep knee flexion.
Medial anatomic stabilizing structures include the patellofemoral (MPFL), patellomeniscal, and patellotibial ligaments, which are the main ligamentous structures that constrain lateral patellar motion. The strongest of these ligaments is the MPFL. The MPFL is a continuation of the deep retinacular surface of the vastus medialis obliquus (VMO).
Cadaveric studies have shown that the MPFL with a tensile strength of 208 N contributes on average 50% to 60% of the total restraining force against lateral patellar displacement. The MPFL has the greatest strain with the knee in full extension, and becomes lax as the patella enters the trochlea and the bony congruity of the joint provides most patella stability. The patella insertion of the MPFL lies between the superomedial and midmedial border of the patella. Recent attention has been focused on the ideal femoral position to restore MPFL strain. The average width of the femoral attachment is 11 to 20 mm and the center of attachment is between the medial epicondyle and the adductor magnus insertion. Several investigators have described this femoral attachment point with regard to radiographic landmarks. This location, commonly known as the Schottle point, can be described as 1 mm anterior to the posterior cortex extension line, 2.5 mm distal to the posterior origin of the medial femoral condyle, and proximal to the level of the posterior point of the Blumensaat line.
The anatomy of the lateral soft tissue restraints is more complicated. The superficial layer consists posteriorly the superficial oblique retinaculum, and anterior lateral restraints largely consist of the expansion of the vastus lateralis.
The deep layer mirrors the medial structures and consists of the deep transverse retinaculum, epicondylopatellar ligament, and the patellotibial band, which attaches directly to the distal pole of the patella and sends fibers into the lateral meniscus and into the underlying tibia. The epicondylopatellar ligament does not attach directly to the tibia but attaches directly via the proximal and distal attachments of the iliotibial band (ITB). As such, the tightness of the ITB influences the lateral stability force conferred by the lateral retinacular structures. The lateral retinaculum contributes approximately 22% of the soft tissue restraint to lateral translation, and is therefore an important stabilizer against lateral patella dislocation. The medial and lateral retinacular structures are most effective within the range from 20° of flexion to full extension.
Once the patella enters the confines of the trochlea, the bony anatomy allows for inherent stability of the patellofemoral joint. At 20° to 30° of flexion the patella is captured in the trochlea groove. Because of this, symptomatic instability usually occurs before the patella is captured. Conditions resulting in patella alta are associated with an increased risk of recurrent patellar dislocations because the patella does not enter the trochlear grove until higher-than-normal levels of knee flexion are achieved. In addition, patients with patella alta have less surface area for articulation because the patella rides higher in the groove.
Clinical History and Examination
Careful history taking and physical examination are important in the evaluation and treatment of patellar instability. Patient age and gender have relevance to recurrence risk. The number of previous clearly identified dislocation or subluxation events and the circumstances under which these occurred should be elicited. A history of general ligamentous laxity or dislocation in the patient or family should be obtained. Any previous surgery and the type of procedure(s) should also be recorded. Elements of the history that are relevant to the patient’s functional status should be obtained, including types of physical activity engaged in by the patient during daily living, work, and sport; particularly those involving in cutting and pivoting. Identification of sensations of patella subluxation of dislocation should be differentiated from a feeling of giving way of the knee caused by reflex quadriceps inhibition. Pain location and activities that trigger it, particularly those involving loading of the patellofemoral joint, should be identified.
Physical examination of the patient with patellar instability should include an evaluation of overall limb alignment, including hip and knee rotation, and an assessment of generalized ligamentous laxity. Quadriceps muscle bulk, tone, and strength should be assessed, along with dynamic evaluation of limb alignment in single-leg squat maneuvers. The presence of apprehension with lateralization of the patella and the absence of a firm end point to lateral translation suggests previous dislocation and damage to the MPFL. Patella tracking (J sign), tilt, and mobility, as well as the presence of crepitus or effusion should be recorded. The Q angle in full extension may be falsely low in patients with medial side laxity, so a knee-flexed Q angle may have greater reliability and more accurately identify the relationship of the trochlear groove to the tibia. The location of tenderness on the patella or along the MPFL should also be noted.
Imaging
Imaging of the patellofemoral joint can involve multiple modalities, including radiographs, bone scans, computed tomography (CT), and MRI. These different modalities can provide valuable information about the anatomy and also in some cases the cause of pain or instability for these patients.
Radiographs
A significant amount of information can be obtained by the use of carefully obtained radiographs regarding abnormal anatomy that can contribute to patellar instability, as well as information about arthritis and loose bodies. Standard anteroposterior and Rosenberg (posteroanterior 45° weight bearing) radiographs primarily provide information about the femorotibial joint and the presence of arthritis, but if carefully examined may also show loose bodies or small avulsion fractures from the medial patella. Lateral radiographs can provide a significant amount of information related to the patellofemoral joint. When taken appropriately (with the condyles overlapping with <5 mm difference), lateral radiographs can provide extensive information not only regarding the presence of arthritis but also patella height, trochlear dysplasia, and patella tilt.
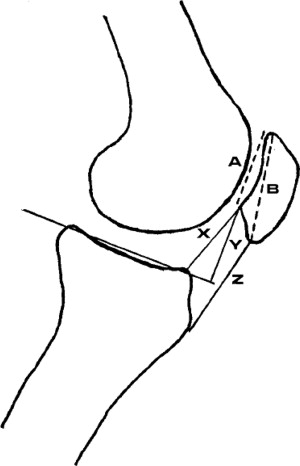
Patella height is typically measured using different ratios of patella size compared with tibial landmarks on a lateral radiograph ( Fig. 1 ). The Caton-Deschamps ratio compares the articular surface length of the patella and its distance with the anterior superior margin of the tibia. The Blackburne-Peel ratio compares the articular surface of the patella and its distance to a line projected forward on the tibial plateau. The Insall-Salvati ratio measures the overall patella length compared with the patella tendon. Normal values are in the 1:1 to 1.2 range, with values of 1:1.3 being considered definitely abnormal patella alta and possibly candidates for a tibial tubercle distalization procedure. The Caton-Deschamps and Blackburne-Peel ratios have been shown to have higher interobserver reliability than the Insall-Salvati ratio, and also have the advantage of being able to show change when a tubercle osteotomy is performed. Therefore, one of these 2 ratios is preferred.
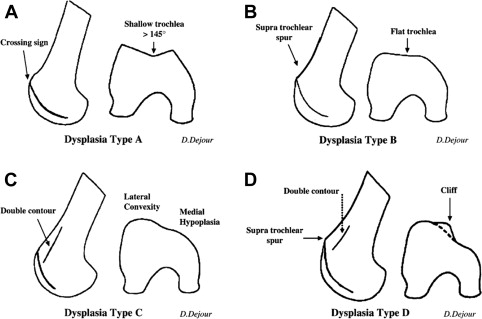
Trochlear dysplasia can be identified on a perfect lateral radiograph by the presence of a crossing sign in which the trochlear groove line intersects the anterior femoral condyle rather than the anterior femoral cortex. The femoral condyles should overlap within 5 mm in order to assess the trochlea accurately. Dejour and colleagues further classified the type of dysplasia by morphologic features of a supratrochlear spur (eperon sus-trochleen) and a double contour line ( Fig. 2 ).
Axial patellar views can provide information about loss of cartilage, spurs, and relative patella tilt and subluxation. The most commonly used in the United States is the Merchant view, taken at 30° to 45° of knee flexion. Multiple angles and indices have been described to measure the trochlea and patella relationship; however, up to 20% of normal knees have subluxation on axial views. In addition, it is difficult to obtain more shallow angles of knee flexion. Because the patella is usually engaged in the trochlea by 30° the value of these views is limited for evaluation of patella instability. The relative importance of these measurements has diminished as improved axial imaging techniques have become available.
Bone Scan
Bone scans typically have less resolution than other imaging modalities, but can provide valuable functional information about metabolic activity of the bone. A diffuse uptake pattern is seen in patients with patellofemoral pain. A more localized pattern can be seen in patients with specific areas of overload or a symptomatic chondral defect causing increased activity in the underlying bone. This pattern can guide treatment such as reducing activity or addressing focal chondral defects that contribute to pain.
CT Scan
CT can provide valuable axial imaging information at high resolution. The primary use has been to evaluate the anterior tibial tubercle–trochlear groove (TT-TG) distance. The mean value is 9 mm. A TT-TG of 20 mm or more has a strong (>90%) association with patella instability. CT imaging can also be used to evaluate relative femoral and tibial version, which can play a role in patella instability.
MRI
MRI has a valuable role in assessing articular cartilage and soft tissue injuries in patella instability. Articular cartilage damage on the medial patella facet and bone bruising of the lateral femoral condyle from relocation impact is common. MRI also has a valuable role in determining the location and extent of medial soft tissue injury that occurs with instability. In many cases, damage to the MPFL is evident. The location of damage to the MPFL injury can be variable, with injury occurring at the femoral origin (∼50%), patella attachment (76%), and also midsubstance (20%); up to 49% have injury at multiple sites. MRI has also been used to measure TT-TG distance using the articular cartilage of the trochlea as the center of the groove. However, MRI TT-TG measurements can underestimate the distance by a mean difference of 3.8 mm compared with CT.
Treatment
Nonoperative Management
Decision making with regard to nonoperative treatment of patients with patellofemoral pain revolves around form and length of immobilization and timing and focus of physical therapy. In broad terms, the goals of early treatment of a patellar dislocation are to reduce swelling, strengthening the surrounding musculature, and improve knee range of motion.
Options for initial immobilization include casting, splinting, or bracing. Patients may either be casted in full extension or in partial flexion. In a long-term study of patients with primary patellar dislocations, those treated the most conservatively in casts for 6 weeks had the lowest risk of redislocation but the highest rates of stiffness. In contrast, patients treated with just a patellar brace had 3 times the risk of redislocation.
Several investigators have compared early operative intervention with nonoperative management of first-time dislocators. A study by Buchner and colleagues with 8-year follow-up of first-time dislocators found no significant difference between the surgically and conservatively treated groups with regard to redislocation, activity levels, functional outcomes, or subjective outcomes. A similar prospective, randomized study by Palmu and colleagues compared 62 patients treated either operatively or conservatively and found no significant difference in subjective outcome, recurrent instability, function, or activity scores.
A smaller study by Arnbjornsson and colleagues followed 21 patients with a history of bilateral patellar dislocations for a mean of 14 years. These patients had 1 lower extremity treated operatively, whereas the contralateral side was treated nonoperatively. In long-term follow-up, the operative extremity had worse arthritis and an increased risk of redislocation.
Physical therapy for patients with patellar instability should center on closed-chain strengthening of the quadriceps and gluteal musculature, patellar taping, and proprioceptive exercises. Closed-chain exercises involving the gluteal musculature tend to increase the external rotation of the femur and as such decrease the Q angle during the gait cycle. Strengthening of the quadriceps musculature, and in particular the VMO, preferentially brings the patella medially in the trochlear groove. Patellar taping has been shown to control excessive patellar motion during therapy and serves to activate the VMO earlier than the vastus lateralis when climbing stairs.
In deciding which first-time dislocators might be better served with early operative intervention, consideration must be given to the patient’s degree of dysplasia and laxity. Patients who have dislocated more than once are likely to dislocate again and continued nonoperative management may not be indicated. As noted previously, patients with MRI-confirmed MPFL avulsion are also at high risk for reinjury and early operative intervention should be considered.
Surgical Management
Indications for surgical management are related to patient pain and function. In many cases, patients have minimal symptoms at rest, but have significantly limited their functional activities because of apprehension. Therefore, risk of recurrence is an important element for consideration in management. Other indications include a symptomatic loose body or cartilage lesions. In general, we have generally avoided surgery on patients who have experienced only 1 subluxation or dislocation event, because many of these patients do not have recurrent dislocation. A survey of National Football League team physicians indicates that most do not recommend immediate surgical management without a loose body. However, if the patient has continued apprehension or a second dislocation event, we typically recommend surgery based on the high rate of recurrence. In addition, for those individuals with significant anatomic abnormalities, we consider early stabilization.
Surgical management of patella instability should be directed at correcting injured structures and, if the risk of recurrence is high, correcting significantly abnormal anatomic features that can contribute to increased risk, without resulting in excessive abnormal loads on the articular cartilage that can ultimately result in arthritis. This approach can include MPFL repair or reconstruction, tibial tubercle osteotomy with medialization and/or distalization, and in some cases trochleoplasty. Current surgical procedures are intended to recreate normal anatomy, rather than impose a nonanatomic constraint to motion. In general, the type and degree of abnormality dictates the particular techniques of surgical management used for an individual.
Arthroscopic and Minimally Invasive Techniques
Arthroscopic and minimally invasive techniques for the treatment of patellar instability include arthroscopic medial plication techniques and miniopen medial reefing techniques, and are typically limited to those patients with minimal amounts of bony malalignment or trochlear dysplasia, or as an adjunct to provide additional soft tissue balancing in patients who undergo bony procedures. The use of isolated arthroscopic lateral retinacular release is not supported by the literature and can result in increased lateral patella mobility and even medial instability. A survey of the International Patellofemoral Study Group resulted in a recommendation that isolated lateral release not be performed for patella instability. For patients that require addressing medial retinacular laxity, we prefer the technique as described by Halbrecht, in which a spinal needle is passed through the substance of the MPFL and a suture is passed through the lumen into the joint and retrieved through a cannula. The needle is then partially drawn back and then advanced the desired amount subcutaneously to pass again through the MPFL, where the suture loop is then retrieved and an arthroscopic knot is then tied intra-articularly. This procedure is repeated 4 to 6 times.
Published results of medial plication techniques have been satisfactory at short-term follow-up. However, this technique in the presence of trochlear dysplasia has been shown to have a high early redislocation rate, and is therefore not recommended as an isolated technique in these patients. It can help successfully reduce residual medial laxity in patients who have a tibial tubercle osteotomy.
Open MPFL repair of femoral side avulsions has also been described with reasonable results, although a recent article from the Mayo Clinic described a 28% failure rate with this technique. Specific technical aspects of this procedure are first to recognize that not all MPFL injuries occur at the femoral attachment, and, second, to clearly identify the femoral origin of the MPFL and verify that the strain behavior of the repaired tissue results in increased laxity of the tissue as the knee flexes. Repair at the femoral attachment if the damage is midsubstance or at the patella insertion does not satisfactorily address the underlying disorder. Nonanatomic or overconstraining repair is likely to either fail or result in excessive overload of the patellofemoral joint, and are to be avoided. We recommend careful identification of the general area of the femoral origin by radiographic imaging of the Schottle point, followed by an adequate incision to assess the anatomic landmarks of the adductor tubercle and medial epicondyle and the femoral origin of the MPFL, which lies in the saddle-shaped depression between them. The MPFL tissue can be brought to this point, and should show less tension as the patella engages the trochlea and the knee flexes. A suture anchor can be placed at the appropriate location and the ligament whip stitched to ensure that the tissue is firmly held. At best, this merely recreates the original, low-strength attachment of the MPFL. We currently consider this in patients with minimal bony malalignment or dysplasia who have a clearly identifiable femoral avulsion of the MPFL, or as an adjunct to a distal realignment procedure in which residual medial soft tissue laxity can be related to a femoral avulsion.
MPFL Reconstruction
MPFL reconstruction is a technically demanding surgical procedure that is intended to rebuild the primary medial restraint to lateral patella translation. Various techniques have been described to replace the often atrophic or lax MPFL, typically with a graft that has significantly higher stiffness and ultimate load to failure than the native tissue. Grafts that have been used include free semitendinosus tendon or gracilis tendon autografts and allografts, bone-patella tendon-bone grafts, partial quadriceps tendon grafts, partial adductor magnus tendon grafts, and tibialis anterior allografts. Different techniques of attaching the graft to the patella have also been proposed, including looping the graft through tunnels in the patella, docking of the graft into a tunnel with an arthroscopic cortical button, anchoring the graft into tunnels with interference screws, attaching the graft to the patella using suture anchors, or suturing it to the retinaculum. Femoral attachment techniques include docking into a tunnel, suture anchors, or looping the graft around the adductor magnus tendon.
Although a variety of different techniques have been proposed, it is critical that any reconstruction respects underlying biomechanical principles in order to be successful. Particularly with strong and stiff grafts, accurate placement and tensioning of the graft is important in order to provide the necessary constraint without limiting knee motion, overloading the medial patella articular cartilage, or causing medial patella subluxation. The normal strain behavior of the MPFL allows approximately 10 mm of lateral translation with the knee in full extension. The MPFL is under less strain after the patella is captured by the bony trochlea. Modeling of MPFL reconstructions has shown that as little as 5 mm of proximal malpositioning or 3 mm of shortening can lead to significant (>50%) increases in load on the medial patella facet. Tension of 10 N can significantly increase patellofemoral contact pressures. Abnormal placement can lead to significant complications such as patella fracture, loss of motion, or arthrosis. However, nonanatomic placement of the MPFL is common, with one recent article reporting that 64% of tunnels were malpositioned. It is difficult to determine how many patients have abnormal tension applied to the graft, but a systematic review of the literature found a 26.1% reported complication rate and a 15.8% reoperation rate following MPFL reconstruction.
Results of MPFL reconstruction show that, in most cases, good patella stability is achieved. Our recommended technique of MPFL reconstruction is used for patients with medial soft tissue laxity or atrophy and who have mild to moderate alignment abnormalities and dysplasia. A skin incision is created at superomedial to midmedial patella border, and dissection is carried through layer 1 to the medial border of the patella superficial to the synovial lining. Soft tissue is cleared from the superomedial corner to the midpatella in this area, and a bony trough is created using a burr. Suture anchors are then placed at the superomedial corner and midpatella.
The femoral insertion of the MPFL is initially identified using fluoroscopy to identify the Schottle point. A longitudinal skin incision is created that allows adequate dissection to clearly identify the adductor tubercle and medial epicondyle, and a guide pin is placed under a combination of fluoroscopic and anatomic guidance into the femoral insertion. The sutures from the suture anchor are then passed under layer 1 inferior to the VMO to the proposed femoral insertion of the MPFL. They are looped around the pin and set at an appropriate tension, and the strain behavior of the sutures is observed as the knee goes through a range of motion. If the femoral insertion site has been appropriately selected, the sutures should have decreased tension as the knee flexes.
Once the appropriate point has been selected, attention is again drawn to the patella. A semitendinosus graft is sutured into the prepared groove using the suture anchors. The free ends are brought under layer 1 to the guide pin, and again the strain behavior of the graft is evaluated through a range of motion. A tunnel of appropriate diameter is reamed over the pin, and the graft ends docked into the tunnel with the knee in 30° flexion and a spacer (such as a closed pair of Mayo scissors) can be used to avoid over tensioning. The graft is then secured with a soft tissue screw. The tension of the graft can be assessed as the knee goes through a range of motion; it should permit lateral motion at all points in early flexion, with approximately 1 cm of lateral motion with the knee in full extension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






