Patella Fractures: Open Reduction Internal Fixation
Matthew R. Camuso
INTRODUCTION
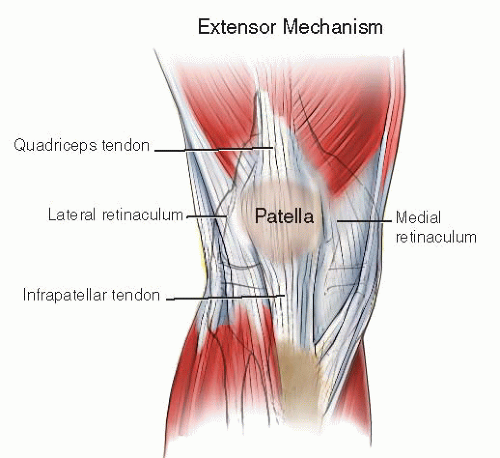
The patella is the largest sesamoid bone in the body and is a key component of the extensor mechanism, adding a distinct mechanical advantage for optimal knee function. Between the massive quadriceps muscle and the sturdy patellar tendon (ligament), the patella transmits three to seven times body weight through the patellofemoral joint during deep knee flexion. In the absence of a patella, the extensor mechanism loses nearly 60% of its strength during terminal extension. The surrounding retinacular tissues are also a key component of the extensor mechanism complex; when intact, they can transmit loads to the leg even in the presence of a displaced patella fracture (Fig. 25.1).
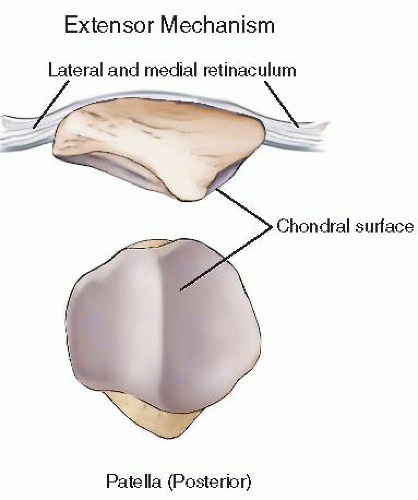
The patella has two chondral facets, each articulating with the patellofemoral groove of the distal femur. The thickest portion of cartilage is in the central third; the patella thins out near its periphery both medially and laterally. Between two-thirds and three-fourths of the undersurface is covered with articular cartilage, with the distal most portion being nonarticular. Understanding the dimensions of the patella will help the surgeon avoid penetration of the articular surface with implants during surgery (Fig. 25.2).
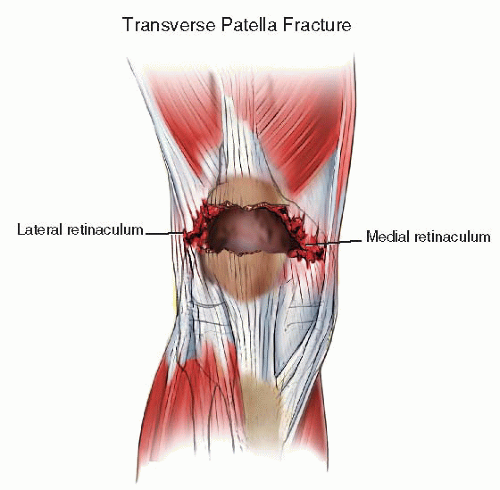
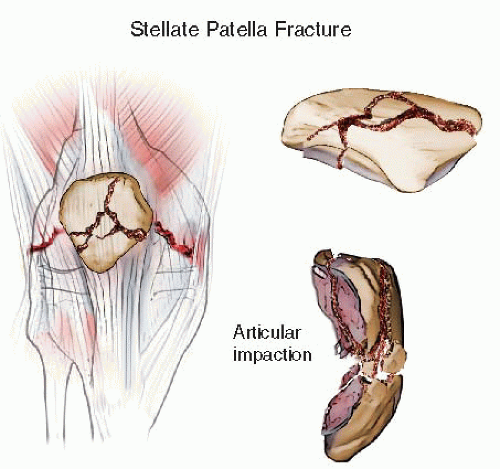
Fractures of the patella are commonly the result of an eccentric load to the knee. An extreme tensile moment results in failure of the patella in the form of a transverse fracture. The injury continues both medially and laterally, tearing the retinaculum, causing a complete disruption of the extensor mechanism (Fig. 25.3). In this setting, fracture fixation is relatively straightforward and is combined with repair of the retinaculum. Alternatively, the patella can fracture when a direct force is applied to its surface, such as when the knee strikes the dashboard in a vehicle crash (Fig. 25.4). Associated injuries are common, and these stellate multifragmentary impacted patella fractures can be very difficult to manage.
CLASSIFICATION
Patella fractures are classified in many ways. The AO/OTA classification groups the fractures into three types.
Type A fractures are extra-articular and are associated with disruptions of the extensor mechanism. These require surgery to restore the continuity of the extensor mechanism. However, articular reconstruction is not necessary. Most commonly, these are fractures of the inferior pole of the patella (Fig. 25.5).
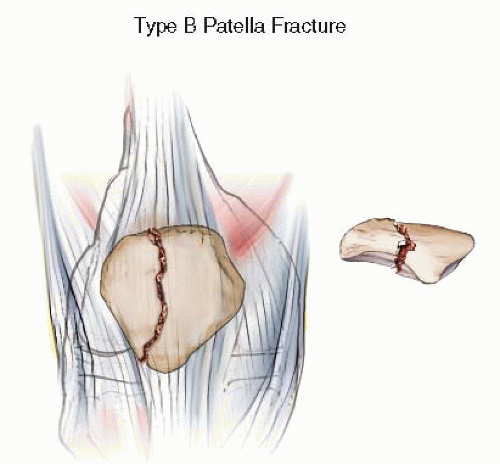
Type B fractures are partial articular fractures. These vertically oriented fractures can often be confused with bipartite patellae. When significant articular displacement is present, operative treatment is recommended to reduce the risk of patellofemoral arthrosis. In these injuries, the extensor mechanism remains intact and therefore does not require repair (Fig. 25.6).
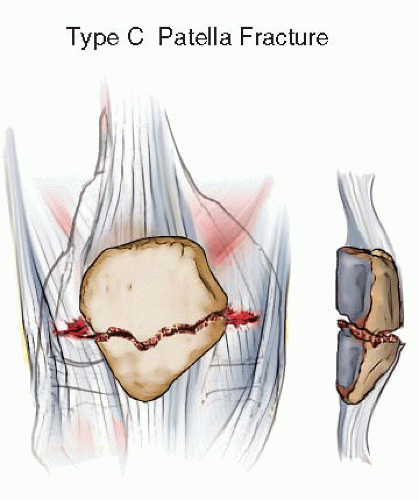
Type C fractures are complete articular fractures, often resulting in displacement of the articular surface with disruption of the extensor mechanism. These fractures occur from a direct fall or blow to the patella, causing a more complex comminuted fracture pattern. Simple fractures are considered C1 fractures. Comminution of one segment of the patella is termed C2. When both poles are comminuted, the fracture is categorized as C3.
These injuries require realignment of the articular surface and repair of the extensor mechanism, making them the most challenging to treat (Figs. 25.4 and 25.7).
INDICATIONS AND CONTRAINDICATIONS
Regardless of the mechanism of injury, a disruption of the knee extensor mechanism leaves the lower limb severely disabled. Surgery is necessary to restore active leg extension and to repair the articular surface of the patella.
A displaced fracture of the patella usually indicates that a significant disruption of the extensor mechanism has occurred. For this reason, surgical treatment should be considered for most displaced patella fractures. Nondisplaced fractures and those with an intact extensor mechanism can be managed nonoperatively in a knee immobilizer, hinged knee brace, or cylinder cast for 4 to 6 weeks.
The goals of surgery are twofold: to repair the extensor mechanism and to restore the articular surface. Restoration of extensor mechanism is necessary for normal gait and independent ambulation. Articular congruity is important to reduce the risk of patellofemoral arthrosis, a condition that is difficult to treat. For this reason,
patella fractures with articular displacement of more than 1 to 2 mm in adults should be considered for repair. The multiply injured patient with a patella fracture, even when minimally displaced, may benefit from internal fixation to allow for early mobilization during rehabilitation.
patella fractures with articular displacement of more than 1 to 2 mm in adults should be considered for repair. The multiply injured patient with a patella fracture, even when minimally displaced, may benefit from internal fixation to allow for early mobilization during rehabilitation.
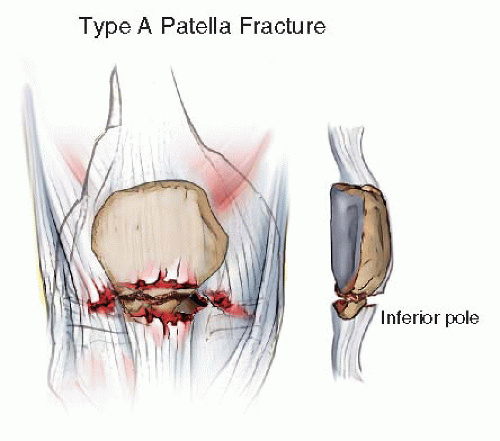 FIGURE 25.5 Type A: Extra-articular, inferior pole patella fracture with disruption of extensor mechanism. |
Relative contraindications for patella fracture surgery include medically frail patients whose surgical risk is high, severe osteoporosis, fractures in nonambulators, and soft-tissue injury or infection that would preclude safely operating on the extremity.
PRE-OP PLANNING
History and Physical Examination
A thorough history is an important part of the initial patient evaluation. A patient with a suspected fracture of the patella presents with pain over the anterior aspect of the knee. Understanding the mechanism of injury (direct force vs. indirect load) gives important information as to the severity of the injury as well as the fracture pattern. Medical history, prior activity level, and patient expectations are important factors that may affect decision making.
Physical examination includes an evaluation of the entire extremity. Gentle palpation and rotation of the hip, thigh, leg, and ankle are important to rule out associated fractures. A careful neurovascular examination with a methodical evaluation of the lower leg compartments should be documented. Knee swelling and ecchymosis are commonly present. Soft-tissue swelling can be significant due to the hemorrhage associated with the fracture and its subcutaneous location. The soft tissues should be thoroughly inspected for abrasions, blisters, or degloving injuries. All wounds around the knee must be appropriately investigated to rule out an open fracture or traumatic arthrotomy, which requires urgent treatment (Fig. 25.8).
In many patients, there is a palpable gap in the patella on examination; however, its absence does not rule out a patella fracture. The hallmark of a patella fracture with disruption of the extensor mechanism is the inability to actively extend the lower leg from a flexed position at the knee. Unfortunately, in most patients, this is difficult or impossible to perform because of pain with displaced fractures. The ability to perform a straight leg raise may suggest an intact extensor mechanism when it’s integrity is in question. Joint aspiration with instillation of local anesthetic can aid in the physical examination for fractures that are not significantly displaced.
IMAGING
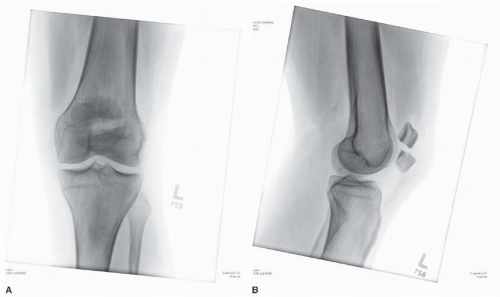
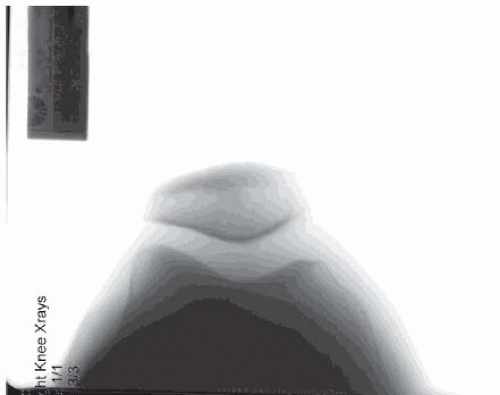
In a patient with a suspected patella fracture, radiographs of the knee, femur, and tibia should be obtained. Plain films are usually sufficient to confirm the diagnosis of patella fracture. The anteroposterior (AP) view can be difficult to interpret secondary to the overlying distal femur. The lateral projection provides the most information regarding the magnitude of articular involvement and fracture displacement (Fig. 25.9A,B). Oblique images and tangential views are rarely necessary but may add information about the extent of comminution. The axial or sunrise view may diagnose a vertical fracture of the patella, which can be difficult to see on traditional views (Fig. 25.10). Comparison views may be helpful when a bipartite patellae is suspected. Other studies such as CT or MRI scans are rarely indicated in isolated injuries to the patella, but may give a better understanding of the extent of comminution in selected cases. In minimally displaced fractures where nonsurgical management is being considered, a MRI scan may give useful information about the integrity of the retinaculum.
TIMING OF SURGERY
The timing of surgery varies depending on the patient’s medical condition or associated injuries. Open fractures require early administration of intravenous (IV) antibiotics, tetanus prophylaxis, débridement of nonviable tissue followed by thorough irrigation and fracture fixation. In closed fractures, fixation is delayed until all other life or limb-threatening conditions have been addressed.
In nonmultiply injured patients, the status of the soft-tissue envelope determines surgical timing. If soft tissues are good, fracture surgery is performed on a semielective basis, usually within the first week following injury. Timely surgery allows for earlier mobilization of the limb and rehabilitation of the quadriceps mechanism. Unnecessary delays in surgery should be avoided to minimize the potential for knee stiffness.
Prolonged delays can result in proximal migration of the patella and shortening of the extensor mechanism associated with spasm of the quadriceps, making reduction and fixation of the fracture more difficult. However, if the soft-tissue envelope is compromised, delay in surgery is warranted to minimize the risk of infection.
Prolonged delays can result in proximal migration of the patella and shortening of the extensor mechanism associated with spasm of the quadriceps, making reduction and fixation of the fracture more difficult. However, if the soft-tissue envelope is compromised, delay in surgery is warranted to minimize the risk of infection.
SURGICAL TACTIC
Patient positioning, the need for intraoperative fluoroscopy, reduction tools, and implants must be clearly communicated to the operating room staff. Large-pointed reduction clamps are necessary for compression of the major fracture fragments; medium and small clamps should be available for smaller fracture fragments. Smalldiameter Kirschner wires (K-wire), size 1.25 to 2.0 mm, are often necessary to hold very small fragments of comminution. In addition, small and minifragment screws (1.5 to 3.5 mm) and plates should be available. Double-ended 1.6-mm K-wires can be helpful for accurate longitudinal wire placement when employing a modified tension band technique with wires. Small fragment-cannulated screws (3.5 to 4.0) can also be used for a modified tension band technique with screws when the fracture pattern allows. Stainless steel wire (16 to 20 gauge) for cerclage or tension band placement, wire tightening devices, and wire cutters are routinely required for patella fracture surgery. Suture and wire passing devices, such as a Hewson suture passer or a 14-gauge angiocatheter, facilitate suture passage through the soft tissues of the extensor mechanism and patella itself. Bank bone graft should be available to support disimpacted articular surfaces. Mersilene tape and/or fiberwire suture should be available if the surgeon believes that augmentation might be necessary.
SURGICAL TECHNIQUE
Anesthesia, Positioning, Imaging
Surgery can be performed using general, spinal, or regional anesthetic techniques. The patient is placed supine on a radiolucent operating room table with the affected limb elevated slightly on a bump (Fig. 25.11). This allows for unobstructed lateral fluoroscopy to be performed without interference from the contralateral limb while bringing the injured limb closer to the surgeon’s view. A tourniquet should be positioned at the proximal end of the thigh, so as not to interfere with draping or the surgical exposure. A towel bump is placed beneath the ipsilateral flank to minimize external rotation of the leg and keep the patella facing upward (Fig. 25.12). A cephalosporin antibiotic is given within 1 hour of the incision and prior to the inflation of the tourniquet.
The entire limb from tourniquet to toes is prepped and draped free (Fig. 25.13). The leg is elevated and exsanguinated with an Esmarch bandage, and the tourniquet is inflated. Care should be taken to ensure that the quadriceps does not get bound up proximally in the tourniquet, preventing distal translation of the superior patellar pole. The fluoroscopic unit is brought in from the opposite side of the patient (Fig. 25.14). Sterile half-sheet drapes will be necessary to maintain sterility for lateral imaging (Fig. 25.15). Remaining in the lateral position, the image intensifier can be moved toward the head of the table, allowing the surgeon to work on the fracture and easily return the unit into position for repeated lateral fluoroscopic views as necessary (Fig. 25.16).
The entire limb from tourniquet to toes is prepped and draped free (Fig. 25.13). The leg is elevated and exsanguinated with an Esmarch bandage, and the tourniquet is inflated. Care should be taken to ensure that the quadriceps does not get bound up proximally in the tourniquet, preventing distal translation of the superior patellar pole. The fluoroscopic unit is brought in from the opposite side of the patient (Fig. 25.14). Sterile half-sheet drapes will be necessary to maintain sterility for lateral imaging (Fig. 25.15). Remaining in the lateral position, the image intensifier can be moved toward the head of the table, allowing the surgeon to work on the fracture and easily return the unit into position for repeated lateral fluoroscopic views as necessary (Fig. 25.16).
FIXATION
Type A Fractures
Type A fractures (Fig. 25.17A,B) require reattachment of the extensor mechanism to the adjacent patella. The vast majority of these fractures occur at the inferior pole of the patella and represent an avulsion of the inferior nonarticular pole of the patella. A much smaller number of cases involve avulsion of the quadriceps muscle from the superior pole. They are often associated with tears in the retinaculum, which may require repair.
Repair strategies for type A fractures fall into two categories:
Securing the small avulsion fractures back to the patella with screw fixation. Screw fixation may be possible when the avulsed fragment is large and noncomminuted. However, this technique may require
supplemental fixation to reduce the tensile stress seen at the repair site during initial healing and rehabilitation.
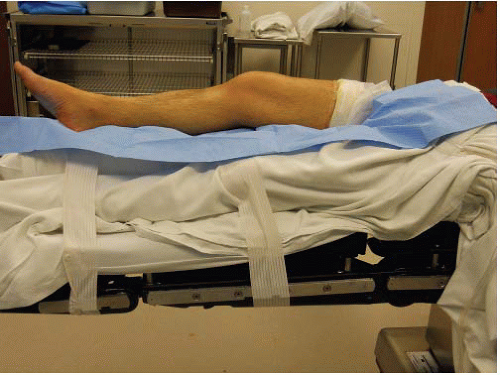
FIGURE 25.11 Patient positioned with injured extremity elevated on a bump and contralateral limb secured beside the bump, keeping it out of the operative field.

FIGURE 25.13 Tourniquet placed at proximal extreme end of thigh allows for full exposure of the operative zone without interference from draping.
Suturing the patellar tendon back to the patella through drill holes. Suture fixation, while maintaining the piece of avulsed bone if possible, allows for bone-to-bone healing while securing fixation in the distal aspect of the disrupted extensor mechanism. A heavy, nonabsorbable suture is used to resist the significant tensile forces seen during knee extension.
With the knee in 5 to 10 degrees of flexion, an anterior approach to patella is performed, extending from 2 to 3 cm above the superior pole of the patella down to just above the tibial tubercle (Fig. 25.18). This allows access to the entire length of the patellar tendon for suture fixation and easy access to the superior pole for knot tying. Full-thickness flaps are created down to the extensor fascia, preserving vascularity to skin layers. The paratenon is incised so that the medial and lateral borders of the patellar tendon are visible. Both medially and laterally, the retinaculum is visualized and inspected for injury. The proximal pole of the patella may be everted to inspect the articular surface. The corresponding trochlear groove of the distal femur is also inspected for articular injury. The inferior pole of the patella is evaluated to determine if it is amenable to screw fixation versus suture repair. In most cases, the inferior pole fracture fragment is too small or fragmented for screw repair alone and requires suture fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree