Chapter 96 Osteotomy About the Knee
International Roundtable Discussion
Michael Stuart
I don’t have any experience with osteotomy computer navigation, but it may be helpful for intraoperative verification of multiplanar corrections in complex cases. I routinely use the weight-bearing line method because it is a simple and reproducible technique for determining the desired coronal plane correction angle (Fig. 96-1) (see Dugdale TW, Noyes FR, Styer D: Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res 274:248–264, 1992). The surgeon chooses the desired coordinate, which equals the angle of correction according to the specific clinical situation (typically 62%; range, 50% to 75%). Remember that standing radiographs can overestimate the magnitude of correction as the result of osseous defects and/or attenuated ligaments. Compare the amount of lateral joint space opening (in millimeters) with the contralateral knee and subtract the difference from the calculated angle (1 degree per millimeter) to avoid overcorrection.
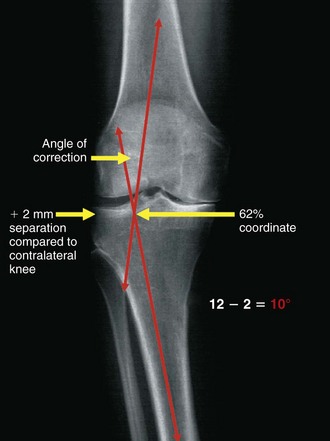
Figure 96-1 The weight-bearing line method is a simple technique for determining the coronal plane correction angle.
(From Stuart MJ: Opening wedge-proximal tibial osteotomy. In Lotke PA, Lonner JH [eds]: Knee arthroplasty, ed 3, Baltimore, 2009, Wolters Kluwer Health/Lippincott William & Wilkins [Master Techniques in Orthopaedic Surgery], pp 361–371.)
David Backstein
Pearls
Thomas Muellner
Pearls
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








