Chapter 94 Osteotomy About the Knee
American Perspective
The purpose of realignment osteotomy about an arthritic knee is to transfer weight-bearing forces from the arthritic portion of the knee to a healthier location in the knee joint.21 This redistribution of mechanical force to increase the life span of the knee joint distinguishes osteotomy from other treatment modalities of arthritic knees.37 The prevalence of realignment osteotomy has steadily declined because of the success of total knee replacement (TKR) and the recent resurgence of enthusiasm for unicompartmental knee replacement.13,67,97 Despite this rather significant decline, osteotomy about the knee remains a viable treatment option in carefully selected patients with knee arthritis.6,40,83,84 The use of osteotomy has increased in patients who are undergoing other surgical procedures such as cartilage or meniscal transplantation or ligamentous reconstruction.12,17,62,94 Over the past decade, interest has exploded in the areas of developing modifications of surgical technique,7,49,52 new surgical instrumentation,16,31 and new fixation devices,93,95 along with the use of external fixation devices1,85,104 and computed tomography (CT)-free navigation systems aimed at improving the accuracy, reliability, and safety of realignment osteotomy.47
Patient Selection Process
The process of patient selection is possibly the single most important factor in obtaining a successful result after osteotomy. Thorough synthesis of multiple variables is required to formulate the decision to proceed with osteotomy (Box 94-1). The primary indications for osteotomy include pain relief for degenerative arthritis associated with malalignment or the need for mechanical axis correction in conjunction with ligamentous reconstruction or transplantation of cartilage or meniscal allografts. It is often helpful to start by focusing on the relative and absolute contraindications to corrective osteotomy during the patient selection process (Box 94-2).
Historical Variables
The ideal candidate for osteotomy is a thin, active individual in the fifth or sixth decade of life with localized, activity-related unicompartmental knee pain, no patellofemoral symptoms, a stable knee, and full knee extension with flexion of at least 90 degrees.37,72 Although many patients do not meet all of these ideal guidelines, a careful selection process will optimize clinical outcomes.
Emphasis on the location and character of pain, the desired activity level, and appropriate patient expectations is particularly important when osteotomy is considered. Diffuse and nonspecific knee pain reduces the chance for a successful outcome after osteotomy. Although it was previously believed that symptoms related to knee instability precluded osteotomy, the practice of treating malalignment in conjunction with concomitant ligamentous reconstruction is becoming increasingly common. Interested readers are referred elsewhere in this textbook for more information on the treatment of young active patients with malalignment and instability. An elderly patient with degenerative arthritis and instability would be optimally treated by TKR rather than osteotomy.42
Patients with osteoarthritis fare better than those with rheumatoid arthritis, and realignment osteotomy for inflammatory disorders is not recommended.23 In the presence of secondary degenerative arthritis from a previous fracture, osteochondritis dissecans, or a prior medial meniscectomy, the results of osteotomy do not seem to be adversely affected, whereas patients who have undergone combined medial and lateral meniscectomy have disappointing outcomes.68,87
Degenerative arthritis of the patellofemoral joint has long been cited as a cause of failure after corrective osteotomy.42 Conversely, long-term studies have shown a low incidence of unsatisfactory results attributed to the patellofemoral joint, and it is possible that realignment of the extremity may favorably alter patellofemoral mechanics inasmuch as it has been demonstrated that patellofemoral pain can improve after upper tibial osteotomy.27,35 Significant retropatellar pain should be a cautionary factor during patient selection, but mild retropatellar pain should not preclude osteotomy if the primary indication for osteotomy is unicompartmental tibiofemoral pain.35
Age assessment requires consideration of physiologic status and lifestyle requirements. Many younger and sedentary patients may be better served by arthroplasty, whereas some elderly and active patients may be better suited for osteotomy. Arthroplasty provides more complete pain relief and shorter rehabilitation and is more reliable than osteotomy in most individuals older than 60 years.42 It has been proposed that unicompartmental knee replacement is an ideal temporizing procedure for middle-aged patients in preference to osteotomy.78,97 Others who believe that unicompartmental knee replacement remains a prosthetic arthroplasty option that should not be considered a direct alternative to osteotomy are concerned about increased complications in young, active patients with prosthetic implants.37,82,84,100
Examination
Ipsilateral hip function should always be assessed, and if hip surgery is required, it should be completed before realignment osteotomy. Limb inspection should confirm the presence of axial malalignment and should assess for the presence of lateral thrust because it is a potential risk factor for a poor clinical outcome.77 In patients with high adduction moments, if sufficient correction of alignment is achieved at surgery, these moments of the knee do not seem to correlate with the clinical outcome.102
It cannot be overemphasized that osteotomy is technically more difficult in obese patients, particularly those with peripheral dystrophic weight distribution. Obesity has been associated with lower success rates after high tibial osteotomy (HTO) because the surgical technique and postoperative immobilization are more difficult in these individuals.27 The long-term clinical results are worse in individuals who exceed their ideal body weight by 1.32 times.27 The activity level of these patients should be carefully assessed because sedentary, overweight individuals of any age may be better served by prosthetic replacement. It should be stressed that significant weight loss may provide enough symptomatic relief to defer any operative intervention.
Counseling
The surgeon needs to discuss all treatment alternatives and to convey that neither osteotomy nor arthroplasty provides a “normal joint.” The long-term results, rehabilitation, pain relief, and durability of realignment osteotomy and arthroplasty should be specified for the patient. A longer postoperative recovery period with less pain relief after rehabilitation is expected after osteotomy. These disadvantages need to be balanced against the possible catastrophic complications of infection or prosthetic failure with arthroplasty in a young and active patient.6,90,100
Specifically, realignment osteotomy is based on the concept that certain high-impact and excessive loading activities are not sanctioned with prosthetic arthroplasty.37 Functional analysis of young patients after osteotomy reveals that many are able to participate in running and jumping activities that probably would damage a knee prosthesis.6,69,75 Many patients also value the real potential for technological advances in arthroplasty over the expected survival period of an osteotomy and recognize that “buying time” with an osteotomy is a viable concept.
The expected results of TKR after osteotomy should be considered and discussed with the patient. Potential technical obstacles encountered include difficulty with exposure,106 bony deficiencies necessitating grafts or wedges, difficulty in attaining ligament balance,73 prolonged operative times,36 and increased blood loss.44,45,54 Other authors have noted no significant differences in the technical difficulty or outcome of TKR after HTO.64,79,91 Poorer long-term radiographic results of TKR after HTO occur in a specific subset of patients.76 These patients are younger, heavier, and more active males who are also at risk for early wear of prosthetic components. A well-performed osteotomy in these patients seems reasonable if the goal is to postpone prosthetic replacement to a later stage in their lives, when their activity level and age favor a decrease in the likelihood that they will require multiple revision surgeries. The literature detailing poor results of arthroplasty after osteotomy clearly indicates that technical difficulties or complications associated with osteotomy produce worse results with the subsequent arthroplasty.15,106 Surgeons with only occasional experience performing corrective osteotomy should consider referral because a suboptimal surgical technique that may compromise subsequent procedures should not be the sole criterion used to abandon osteotomy.
Other important variables in this patient population also portend a poor result. Factors that prognosticate a worse outcome in HTO patients (P < .01) include (1) workers’ compensation claim, (2) history of reflex sympathetic dystrophy after HTO, (3) early onset (within 1 year) or no period of relief of pain after HTO, (4) multiple surgeries before HTO, and (5) occupation as a laborer.66
Radiographic Evaluation
The location and severity of arthritis are determined by standing anteroposterior, lateral, intercondylar notch, and skyline patellar views. One should carefully inspect the contralateral tibiofemoral compartment for marginal osteophytes, which indicate the presence of diffuse arthritis. Tibiofemoral subluxation, excessive bony erosion, and diffuse arthritic involvement are associated with poorer outcomes. A full-length, 51 × 14-inch, weight-bearing radiograph is necessary to determine the mechanical axis.89 Although high correlation between anatomic and mechanical axes is generally noted, long films are also helpful in determining whether deformities of the tibia or femur exist, and in revealing the effect that these deformities have on overall mechanical alignment.
Preoperative Planning
The principal considerations in osteotomy planning include the location, direction, and magnitude of malalignment (Box 94-3). These variables need to be weighed concurrently during the planning phase to achieve appropriate angular correction. One of the reasons for premature failure after osteotomy is undercorrection or overcorrection of the deformity, which may be due to deficiencies in the preoperative planning process or the surgical technique.27,80,89 Clearly, philosophy, training, and experience heavily bias preference for a specific osteotomy technique. The rationale for choosing between one of these options is delineated in the discussion of these various techniques (Box 94-4). In recent times, varus deformities have been corrected by HTO, whereas most valgus deformities are corrected by distal femoral osteotomy. Previously, the most pragmatic approach for most surgeons was a closing wedge osteotomy; however, opening wedge techniques are becoming more popular.28,38,49,55
Intra-articular deficiencies require special consideration when the degree of desired angular correction is calculated. Slack collateral ligamentous restraint causes angular deformity, and tibiofemoral separation requires subtraction of roughly 1 degree per millimeter to avoid overcorrection (the correction factor will change depending on the actual width of the proximal tibia).29 It is important to remember that ligamentous laxity will not be detected on standing radiographs when laxity exists in the same compartment that is being overloaded. For example, lateral ligament laxity in a valgus knee or medial collateral ligament (MCL) laxity in a varus knee, not observed on radiographs, may cause overcorrection of alignment after realignment osteotomy once the load has been shifted toward the opposite compartment of the knee.
Some patients with proximal tibial varus deformity have excessive valgus angulation of the distal femoral articular surface. This obliquity of the distal femoral surface affects the magnitude of alignment correction and requires special consideration during preoperative planning because patients with femoral shaft–transcondylar angles less than 9 degrees have an increased incidence of undercorrection.81 Increased valgus orientation of the distal end of the femur can result in deleterious overcorrection after HTO.80 Extra-articular deformities distant from the knee joint may need to be addressed at the apex of the deformity, rather than by periarticular correction.
The magnitude of coronal plane malalignment may dictate the location of the osteotomy or may suggest the use of a particular technique. For example, excessive malalignment may contraindicate HTO if the tibial articular surface will be adversely tilted, and for malalignment exceeding 12 to 15 degrees, a supracondylar femoral osteotomy is recommended.26 Alternatively, a dome or barrel vault osteotomy allows greater correction with less effect on the resultant joint line obliquity and should potentially be considered for varus deformities exceeding 20 degrees.9 For severe deformities, a dual (double) osteotomy of the distal femur and the proximal tibia may be deemed necessary.11 Sagittal plane deformities can be corrected with proper planning and appropriate adjustment of the osteotomy technique. As HTO techniques are becoming more refined, more attention is being directed to the sagittal plane of correction in an attempt to better offload areas with significant cartilage damage.4,59
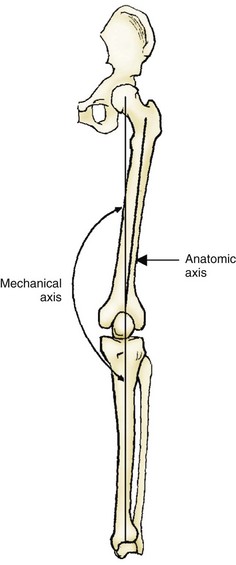
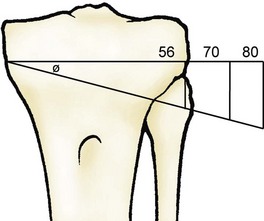
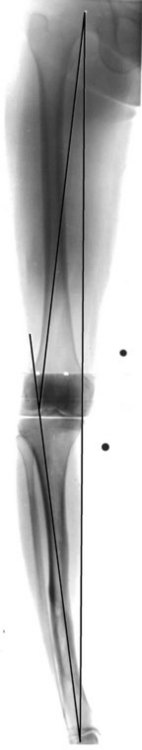
Historically, axial limb alignment was determined by measuring the femoral–tibial (anatomic) angle from standing radiographs and then judging the amount of correction required to restore this angle to normal, which typically averages 5 degrees of valgus (Fig. 94-1). The height of a tibial osteotomy wedge was then estimated by the rule of thumb, so that each millimeter provided roughly 1 degree of angular correction. This method of calculation is accurate only when the actual width of the tibial flare is 56 mm, and it is significantly altered by differences in tibial width or distortion that may result from radiographic magnification.24 Use of this method without consideration of actual tibial width invariably leads to undercorrection because the mean tibial width is 80 mm in men and 70 mm in women (Fig. 94-2). The mechanical axis averages 1.2 degrees of varus and is based on a line connecting the centers of the femoral head and the tibiotalar joint (see Fig. 94-1). This axis is more accurate than the anatomic axis when load transmission forces across the knee joint are defined, particularly when femoral or tibial deformities are contributing to malalignment.
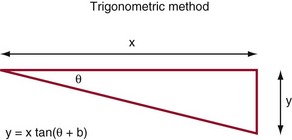
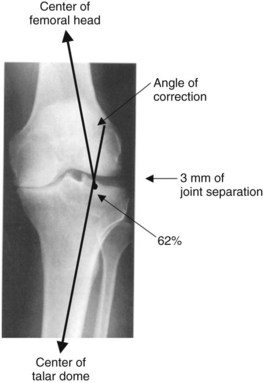
One measurement method for HTO uses the mechanical axis on a full-length standing radiograph with radiographic markers to adjust for magnification. By using trigonometric principles and adjusting for radiographic magnification, the intended wedge height is determined by ascertaining the amount of angular correction required to place the mechanical axis at the desired location within the knee joint. The formula for these calculations is shown in Figure 94-3. A similar method, the weight-bearing line method, divides the tibial plateau from 0% to 100% (medial to lateral) to determine the appropriate coordinate for the mechanical axis to intersect the knee joint (Fig. 94-4).29 Lines to the center of the femoral head and the talar dome connect this coordinate, and the angle formed by these lines is the angle of desired correction. This angle is adjusted accordingly for distraction of the tibiofemoral joint surfaces allowed by ligamentous laxity and articular cartilage deficiency. The height of the wedge is then calculated by tracing the wedge on the radiograph and normalizing the measured height of the wedge by the amount of radiographic magnification. Both of these measurement methods account for the actual width of the tibial plateau.
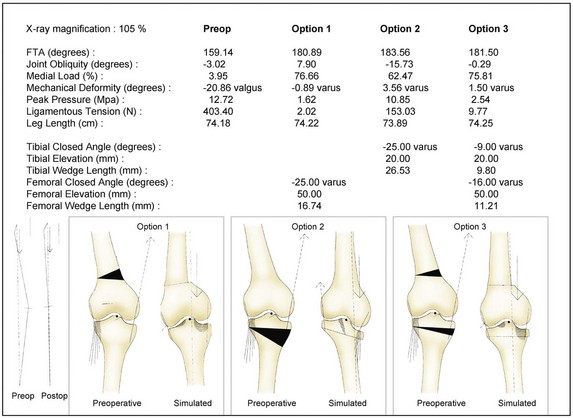
A full-length radiograph used for measurement of mechanical alignment is a static measurement only. Soft tissue tension, joint line obliquity, and upper body gravity shift also affect tibiofemoral plateau pressure distribution during dynamic gait. Software programs are emerging to help with preoperative assessment of these factors and to assist the surgeon’s in final determination of the location, magnitude, and type of knee osteotomy.31,47 The data printout generated by these programs details various osteotomy options and seems most useful for several specific circumstances: (1) in deciding whether to perform a periarticular osteotomy or an osteotomy at the apex of the deformity away from the knee joint, and (2) in determining whether joint line obliquity may be adversely affected after correction of severe malalignment with a particular technique, thereby suggesting the need for a combined dual osteotomy of the tibia and femur. Currently, no data suggest the upper limit of acceptance for resultant joint line obliquity, and we often accept up to 10 degrees of joint line obliquity before proceeding with a dual osteotomy (Figs. 94-5 to 94-9).
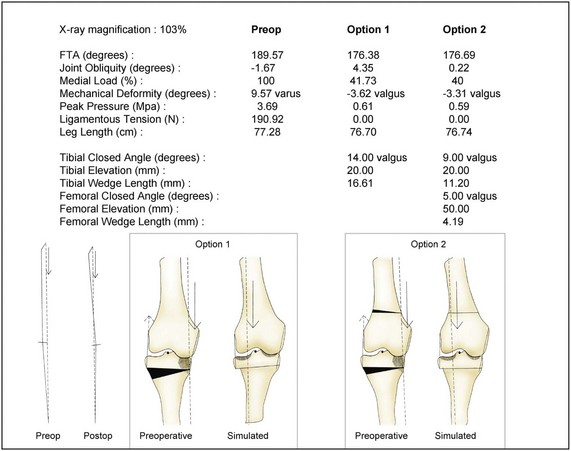
Figure 94-6 An OASIS data printout obtained from the full-length radiograph in Figure 94-5 details several corrective osteotomy options. Option 1, with a proximal tibial wedge resection of 16.61 mm, is calculated to leave 4.35 degrees of resultant joint line obliquity. Option 2 describes a dual osteotomy designed to minimize resultant joint line obliquity. FTA, Femorotibial angle.

Figure 94-9 Spot views of the full-length radiographs presented in Figure 94-8. Note the correction of the mechanical axis from the 95% coordinate in the preoperative radiograph to the 50% coordinate (neutral position) in the postoperative radiograph.
Surgical Techniques
The accuracy of the osteotomy based on preoperative planning and intraoperative technique cannot be overemphasized. With closing wedge techniques, apposition of bone surfaces facilitates prompt healing, whereas proper orientation and resection of bone ultimately determine final mechanical alignment. Opening wedge techniques provide greater versatility intraoperatively, with the surgeon able to manipulate the osteotomy site after the initial bone cut, although this technique also requires special attention to detail and must be carried out meticulously. Jig systems to assist in achieving correct placement and orientation of the osteotomy appear to be particularly useful for many surgeons who have limited experience performing these osteotomies.16,41 The use of intraoperative radiographs and fluoroscopy to document that appropriate alignment has been achieved is recommended.
Historically, loss of patellar height was often seen with closing wedge osteotomy techniques because the knee was subsequently immobilized in a postoperative cast with resultant contracture of the patellar ligament. This complication has become less common because surgeons are now using more rigid fixation methods that allow earlier knee mobilization during the immediate postoperative period.2,16,105 Although loss of patellar height has been seen with opening wedge techniques, the cause of this phenomenon differs in that the opening wedge technique causes an elevation of the joint line that results in patellar migration distally relative to the femoral trochlea rather than patellar ligament contracture.108 The clinical implications of patella infera associated with HTO remain poorly understood.
Varus Deformity
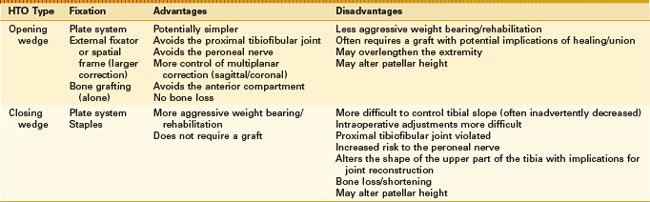
For varus malalignment about the knee, many surgeons continue to prefer a lateral closing wedge osteotomy of the proximal tibia.* Because of its perceived simplicity, medial opening wedge osteotomy is becoming more popular.† Both techniques are used to address varus malalignment with medial compartment arthritis, and each technique has inherent advantages and disadvantages. The decision to use one over the other must be based on the surgeon’s philosophy and clinical experience (Table 94-1). Although they are less commonly performed, dome osteotomies and double osteotomies are viable treatment options in selected individuals.11,48,53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree