Osteochondritis Dissecans of the Knee
Dawn L. Swarm MD
Robert A. Pedowitz MD, PhD
Traditionally, osteochondritis dissecans (OCD) is divided into juvenile (open physes) and adult (closed physes) formed based on skeletal maturity.
Typically, the skeletally immature patient initially is treated nonoperatively and has a better overall outcome.
Because operative intervention is the treatment of both adult OCD and an osteochondral fracture, most surgeons do not bother to differentiate the two.
The etiology of OCD remains unclear. Growth disorders, epiphyseal ossification abnormalities, endocrine imbalances, ischemia, genetic predisposition, and repetitive microtrauma have been theorized to be causes. In addition, OCD has been associated with other musculoskeletal abnormalities.
One common characteristic in patients with juvenile OCD is a high level of athletic activity.
The prevalence of OCD seems to be increasing, with the mean age decreasing and more females being affected. A contributing factor may be increased participation in higher competitive levels of organized sports by younger children.
In juvenile patients, the initial complaints are of vague, nonspecific, poorly localized anterior knee pain that worsens with activity and improves with rest. These symptoms are difficult to distinguish from those of patellar femoral syndrome.
Initial plain-film radiographs should include anteroposterior, lateral, and notch views of the knee, with an additional Merchant view if a patellar or trochlear lesion is expected. The notch view demonstrates the most common areas of OCD.
Comparison views should be obtained in pediatric and adolescent patients to prevent confusion with normal bone development.
Computed tomography provides bony detail of OCD lesions and are helpful in determining the size of the defect or if loose bodies are present.
Magnetic resonance imaging (MRI) can give an accurate estimation for the size of the lesion as well as the status of the cartilage and underlying bone.
The critical issue is to determine the stability of the lesion itself, if the cartilage over the lesion is intact or has fractured, and if the subchondral bone has separated from its base.
Any unstable lesion must be treated surgically.
Mechanical stabilization of fragments can be performed with a variety of devices, such as Kirshner wires, compression screws, bone pegs, bioabsorbable screws, and fibrin glues.
Fresh osteochondral allografting has been proposed as a viable option for treatment of osteochondral defects. Patient selection is critical to the success of this procedure. Patients should be active and well motivated, and any limb malalignment must be corrected before transplantation.
The term osteochondritis dissecans, or OCD, was first used by Konig in 1888, when he described loose bodies, or “corpora mobile,” involving the articular surface of the joint. He initially speculated that these were caused by an inflammatory reaction that led to spontaneous necrosis of the subchondral bone and overlying cartilage (i.e., “dissecting inflammation”) (1,2). Although Konig later retracted inflammation as the cause, the term is still commonly used today to describe the separation of an articular cartilage subchondral bone segment from the remaining articular cartilage (1,3,4,5,6,7,8).
Traditionally, OCD is divided into juvenile (open physes) and adult (closed physes) forms based on skeletal maturity (1,5,7). This distinction is useful in determining treatment options, because typically, the skeletally immature patient initially is treated nonoperatively and has a better overall outcome (1,3,5,7).
Some believe that adult OCD is a progression of an unresolved juvenile OCD lesion, but it is difficult to differentiate from a traumatic osteochondral fracture (1,4). Because operative intervention is the treatment of both adult OCD and an osteochondral fracture, however, most surgeons do not bother to differentiate the two (1).
The etiology of OCD remains unclear, and multiple hypotheses have been proposed. Growth disorders, epiphyseal ossification abnormalities, endocrine imbalances, ischemia, genetic predisposition, and repetitive microtrauma have been theorized as causes (1,2,3,4,6,7,8,9,10,11,12,13,14,15). In addition, OCD has been associated with other musculoskeletal abnormalities, such as Legg-Calve-Perthes disease, ligamentous laxity, genu valgum, genu varum, tibial torsion, patellar malalignment, and Sinding-Larsen-Johansson and Osgood Schlatter disorders (3,16,17).
One common characteristic in patients with juvenile OCD is a high level of athletic activity (3,5,7,13,18,19). It is two- to threefold more common in males than in females, usually presenting between 10 and 20 years of age (5,8,13). It may be bilateral in up to one third of cases (4,13).
The incidence of OCD is unknown. Most published reports involve small numbers of patients referred to large centers, a lack of uniformity in the classification systems, and inconsistency in diagnosis and management (4,7).
The prevalence of OCD, however, seems to be increasing. A contributing factor may be increased participation in higher competitive levels of organized sports by younger children. Many children are engaged in organized sporting leagues year-round. The mean age is decreasing, and more females are involved. The advancement of arthroscopy and the widespread use of MRI also may have contributed to the increase in prevalence, because more patients with this disorder are being recognized (3,4).
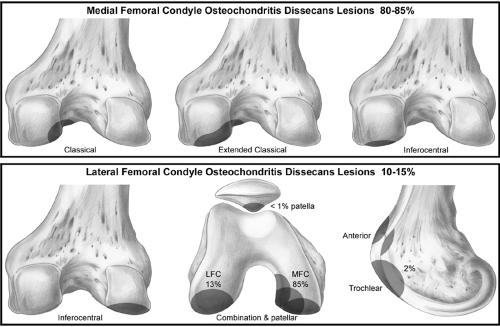
Knee OCD lesions are seen most commonly (70% to 80%) in the “classic” or extended classic location (4,5,7,8,20). The classic site is the posterolateral aspect of the medial femoral condyle, and the extended classic site extends into the weight-bearing portion of the medial femoral condyle (Fig 43.2-1). Inferocentral lateral condylar lesions are seen in 15% of cases (8,21,22). Lateral condylar lesions also have been associated with lateral discoid menisci (19,23,24,25,26). Patellar involvement is uncommon (<5%) but, when present, is located in the inferior pole. Femoral trochlear lesions account for less than 1% of cases (4,5,8,12,27,28).
In juvenile patients, the initial complaints are of vague, nonspecific, poorly localized anterior knee pain that worsens with activity and improves with rest (18). These symptoms are difficult to distinguish from those of patellar femoral syndrome. A high index of suspicion should be maintained for active juvenile patients with these complaints (7). Other patients may be asymptomatic, with lesions being discovered incidentally when radiographs are obtained for unrelated reasons. In a European multicenter study of more than 500 juvenile cases of OCD, 32% of patients had no or little pain at the time of diagnosis (2).
In both the juvenile and adult forms, symptoms are preceded by trauma to the knee in from 40% to 60% of cases (5,29). Patients may complain of stiffness with or after activities and occasional swelling, and there may be tenderness over the affected condyle with the knee flexed. An unstable lesion may cause grinding, catching, or locking and, thus, a decrease in range or motion and/or an effusion. The patient may walk with an antalgic gait, externally rotating the involved lower extremity to prevent impingement of the lesion on the tibial spine when the lesion is in the classic location (1,4,5,13).
In 1967, Wilson (30) described a clinical test that is specific for diagnosing the classic medial femoral condyle lesion termed the Wilson sign. The test is performed by flexing the knee to 90 degrees, then slowly internally rotating the leg and extending it. Patients with a positive Wilson sign complain of pain at 30 degrees of flexion when the tibial spine abuts against the medial femoral condyle. The pain is relieved with external rotation (5,8,18,31). Unfortunately, however, this test is unreliable. Multiple studies found that from 70% to 75% of both juvenile and adult patients with OCD lesions had a negative Wilson sign during clinical evaluation (2,7,31).
Using the appropriate sequences and modalities will aid in the accurate assessment of the stability of OCD lesions and prevent unnecessary invasive procedures.
Plain-film Radiographs
Initial plain-film radiographs should include anteroposterior, lateral, and notch views of the knee, with an additional
Merchant view if a patellar or trochlear lesion is suspected. The notch view improves the yield, because it demonstrates the most common areas for OCD (1,10,11,13,27,28,33) (Fig 43.2-2). If the lateral view is scrutinized in the posterior half of the condyle, then the lesion usually can be identified. Characteristic findings include a well-circumscribed area of subchondral bone separated by a crescent-shaped, sclerotic, radiolucent outline of the fragment. The lesion may be entirely radiolucent, but it often contains a central fragment of bone (7,8).
Merchant view if a patellar or trochlear lesion is suspected. The notch view improves the yield, because it demonstrates the most common areas for OCD (1,10,11,13,27,28,33) (Fig 43.2-2). If the lateral view is scrutinized in the posterior half of the condyle, then the lesion usually can be identified. Characteristic findings include a well-circumscribed area of subchondral bone separated by a crescent-shaped, sclerotic, radiolucent outline of the fragment. The lesion may be entirely radiolucent, but it often contains a central fragment of bone (7,8).
Comparison views should be obtained in pediatric and adolescent patients to prevent confusion with normal bone development or areas of irregular ossification (5,8,13). In younger children (age 7 to 12 years), irregularities of the
distal femoral epiphyseal ossification center may simulate OCD. These irregularities, however, actually are benign anatomical variants of normal ossification. They are located on the posterior portion of the condyles and are best seen on a tunnel view, or posterior to a line coincident with the posterior femoral cortex intersecting the femoral condyle in the lateral view (4,5,7,13). An MRI may help to differentiate the two, and a bone scan will be normal in patients with irregular ossification variants.
distal femoral epiphyseal ossification center may simulate OCD. These irregularities, however, actually are benign anatomical variants of normal ossification. They are located on the posterior portion of the condyles and are best seen on a tunnel view, or posterior to a line coincident with the posterior femoral cortex intersecting the femoral condyle in the lateral view (4,5,7,13). An MRI may help to differentiate the two, and a bone scan will be normal in patients with irregular ossification variants.
A plain-film radiograph may localize the OCD lesion, rule out other bony pathology, and evaluate skeletal maturity, but routine radiographs are poor tools for determining the stability of the lesion or the state of the overlying cartilage (4,8,34). Therefore, additional studies are necessary to develop a treatment plan.
Scintigraphy
Technetium bone scans have been used to localize the lesion to a specific joint and to follow the progression of healing in juvenile patients, but it cannot delineate the state of the cartilage (4,7,15). Cahill and Berg (35) proposed that the degree of osseous uptake on bone scans was related to the regional blood flow or osteoblastic activity and, therefore, to the potential for healing. Those authors developed a protocol that included a bone scan for initial diagnosis with serial scans every 6 to 8 weeks to evaluate healing in the nonoperative patient as well as a qualitative classification scheme comprised of four stages. They used both scintigraphy and serial clinical examinations to follow the progress of healing. If three serial scans remain at the same stage, then healing of the lesion without surgery is doubtful.
To further evaluate the use of scintigraphy for the treatment of OCD, Paletta et al. (36) retrospectively reviewed the records of 12 patients and found that bone scans were 100% predictive for the prognosis of nonsurgical OCD management in six patients with open physes. A bone scan was less useful, however, in six patients with closed physes, showing a predictive value of only 33%.
The adolescent patient nearing skeletal maturity is the most difficult to treat. Bone scans do not seem to be a good method for determining treatment in this age group. In addition, the isotopic tracer remains in the area in question for a significant amount of time even after healing, which makes interpretation difficult (4). Serial bone scans have not been widely adopted. Possible reasons include the time required for the study, the need for intravenous access, the perceived risk of the isotope, and the emergence of MRI (4,7,15).
Computed Tomography
Computed tomography provides bony detail of OCD lesions and is helpful in determining the size of the defect or loose body, if present (8,37). Adding a contrast agent increases the accuracy and ability to stage OCD lesions. If the contrast agent infiltrates into the cleft, then the computed tomographic scan depicts a loose or unstable fragment (15). Because MRI provides more detailed information, however, computed tomography rarely is used in determining the treatment plan.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree