“shoulder”; these lesions often require more reconstructive procedures, so three-dimensional imaging is helpful to assess this integral lateral cortex (Fig. 16-2).
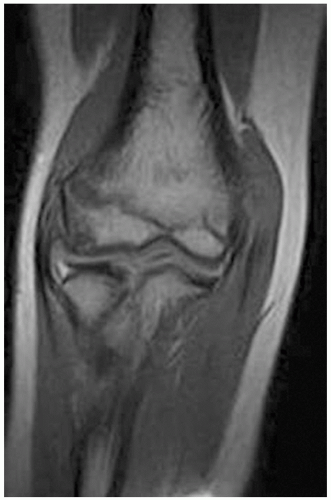 FIGURE 16-1 This MRI demonstrates an early capitellar OCD lesion, as noted by the destruction of the cartilage cap, but no evidence of ring enhancement of the lesion. |
fragment viability (Fig. 16-1). Dye leaking between the fragment and surrounding bone indicates a break in the cartilage, and therefore, operative stabilization or excision is required. Type II lesions demonstrate more advanced disease on radiographs, such as sclerosis surrounding the lesion, and the patient may complain of mechanical symptoms from a loosely attached lesion (Fig. 16-2). Type II lesions are differentiated from type III lesions by the chronicity and presence of intra-articular loose bodies, though both types normally warrant operative treatment to stabilize and/or debride the lesion. Lastly, Bradley and Petrie (5) described the rare type IV lesions as those with a “bipolar” lesion noted on the radial head, which can be simultaneously treated with debridement, curettage, and subchondral drilling at the time of capitellum surgery.
TABLE 16-1 The Arthroscopic Classification System of the Elbow for Osteochondritis Dissecans. | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
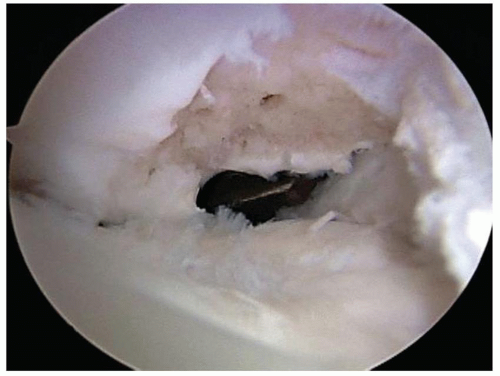
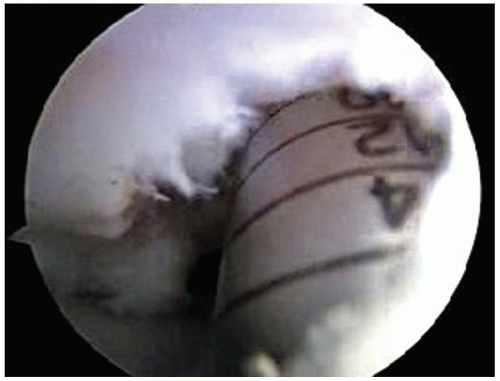
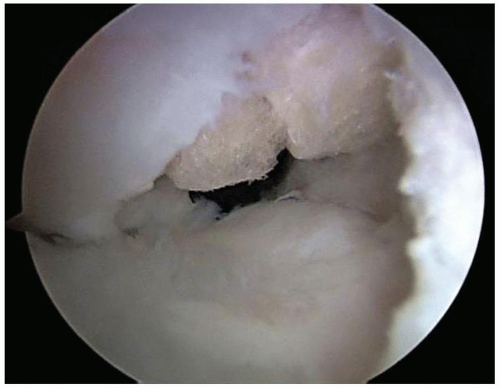
of the anterior compartment, debridement and removal of any loose bodies is performed through a proximal or standard anterolateral portal. It is important to look at the coronoid fossa for occult loose bodies. The arthroscope is removed from the proximal anteromedial portal, but the inflow cannula remains in this portal, allowing inflow to “wash” debris toward the posterior lateral gutter and away from the anterior compartment. Attention is then turned to the posterior compartment, first addressing the olecranon fossa for any loose bodies, which are removed via a posterior central or posterolateral portal, and then visualizing the lateral gutter (Fig. 16-4). The inflamed posterolateral plica is removed first to allow better visualization of the capitellum. Usually, the capitellar lesion is best viewed through a 70-degree arthroscope in the superior posterolateral portal, thereby leaving the standard and distal soft spot portals and the direct lateral portal available for instrumentation (Fig. 16-5). Some surgeons prefer to visualize from the distal soft spot portal, but the authors prefer to use that portal for drilling, microfracture, and grafting (Fig. 16-6). One additional portal that may be used in unconstrained lesions is the straight lateral-distal portal used for horizontal grafting. The elbow may be flexed and extended to aid in visualization, and flexion to 120 degrees or 130 degrees usually allows visualization of the entire lesion. The cartilage cap may be probed for soft spots and fissures and then a curette used to remove the loose and damaged tissue. A shaver or ring curette is then used to debride all necrotic bone to a stable bed, surrounded by a stable rim of cartilage. It is vital to preserve the lateral aspect of the capitellum to maintain a constrained lesion, as the unconstrained lesions that involve the lateral shoulder of the capitellum have a much worse prognosis. This aspect of the capitellum is necessary to provide both bony stability and lateral ligament and capsular attachments. Upon completion of debridement, the base of the lesion is then drilled or microfractured with a small awl to stimulate a bleeding response (Figs. 16-7 and 16-8).
 Get Clinical Tree app for offline access 
|