Osteochondral Lesions of the Talus: Structural Allograft
Mark E. Easley
Samuel B. Adams Jr.
James A. Nunley II
DEFINITION
Large osteochondral defects of the talar dome, typically involving the talar shoulder (transition of superior dome cartilage to the medial or lateral talar cartilage), and also often associated with large-volume subchondral cysts
ANATOMY
Sixty percent of the talus’ surface area is covered by articular cartilage.
The talus is contained within the ankle mortise.
Superior talar dome articulates with the tibial plafond.
Medial dome articulates with the medial malleolus.
Lateral dome articulates with the lateral malleolus.
Talar blood supply
Posterior tibial artery
Artery of the tarsal canal
Deltoid ligament branch
Peroneal artery
Artery of the tarsal sinus
Dorsalis pedis artery
PATHOGENESIS
The pathogenesis for osteochondral lesions of the talus (OLTs) is not fully understood.
Theories include the following:
Trauma
Idiopathic focal avascular necrosis
NATURAL HISTORY
In general, OLTs do not progress to diffuse ankle arthritis.
However, large-volume OLTs may lead to subchondral collapse of a substantial portion of the talus and thus create deformity, higher contact stresses, and a greater concern for eventual ankle arthritis if left untreated.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients may or may not report a history of trauma.
Ankle pain, typically on the anterior aspect of the ankle, is a common complaint.
Pain is usually experienced on the side of the ankle that corresponds with the OLT, but it may be poorly localized to the site of the OLT. In fact, sometimes, medial OLTs produce lateral ankle pain and vice versa.
Pain is rarely sharp, unless a fragment of the OLT should act as an impinging loose body in the joint.
It is typically a deep ache, with and after activity, and is usually relieved with rest.
Antalgic gait
May be associated with malalignment or ankle instability
Typically, tenderness on side of ankle that corresponds with OLT, but not always
Rarely crepitance or mechanical symptoms
With chronic OLT, some degree of ankle stiffness is anticipated.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs
Small OLTs may be missed.
Large OLTs are usually identified on plain radiographs, three views of the ankle, weight bearing.
Radiographs are often limited in characterizing OLTs because the two-dimensional study cannot define the threedimensional OLT.
Particularly useful in assessing lower leg, ankle, or foot malalignment, which needs to be considered in the management of OLTs
May detect incidental OLTs (patient has radiograph for a different problem and an OLT is incidentally identified on plain radiographs)
Magnetic resonance imaging (MRI)
Excellent screening tool when OLT or other foot-ankle pathology is suspected
Will identify incidental OLT but defines other potential soft tissue pathology
Demonstrates associated marrow edema that may lead to overestimation of the OLT’s size
Computed tomography (CT)
Ideal for characterizing OLTs, particularly large-volume defects
Defines OLT size without distraction of associated marrow edema
Defines the character of the OLT and extent of its involvement in the talar dome
Diagnostic injection
Intra-articular
An anesthetic versus anesthetic plus corticosteroid
May have some therapeutic effect, even for several months
If the source of pain is the OLT, then intra-articular injection should relieve symptoms from OLT (and any intra-articular pathology). If the pain is not relieved, then extra-articular diagnoses should be considered.
DIFFERENTIAL DIAGNOSIS
Loose body in ankle joint
Ankle impingement (anterior or posterior)
Chronic ankle instability (lateral or syndesmosis)
Ankle synovitis or adjacent tendinopathy
Early ankle degenerative change
NONOPERATIVE MANAGEMENT
Activity modification
Bracing
Physical therapy if associated ankle instability
Nonsteroidal anti-inflammatories or COX-2 inhibitors
Corticosteroid injection
Viscosupplementation
SURGICAL MANAGEMENT
Preoperative Planning
Indications for this surgery include the following:
Large-volume OLTs not amenable to other joint-sparing procedures
Failed arthroscopic surgery (débridement and microfracture)
Failed open procedures (cylindrical osteochondral transfer)
Large-volume OLTs typically are not amenable to autologous osteochondral transfer (talus or knee).
We favor reconstruction of the large talar defect with an allograft talus. Although we prefer fresh allograft tissue, we have on occasion used fresh frozen tissue.
Scheduling of this procedure with fresh allograft tissue is similar to organ transplantation but with a wider window for implantation after procurement.
Multiple tissue banks have the ability to obtain fresh allograft tali.
Once a donor talus is identified, the tissue bank performs appropriate screening.
If the talus is deemed safe for implantation and represents a match based on radiographic size, on average 14 to 21 days of reasonable chondrocyte viability remains for the talar allograft to be used.
Although fresh structural talar allograft reconstruction for large-volume OLTs has gained a foothold as an accepted treatment among reconstructive foot and ankle surgeons, not all third-party payers cover this procedure. We do not seek an allograft talus for our patients from the tissue banks until our patient has secured insurance coverage for the procedure.
In seeking an allograft talus that is suited for the patient, the surgeon must:
Be sure that the talus is the correct side (right or left).
Provide the tissue bank with the optimal size of talar graft. Tissue banks use different methods for talar sizing.
Plain radiographic dimensions (if the defect in the diseased talus is particularly large, making measurements difficult, radiographs of the healthy, contralateral talus may be needed)
CT scan measurements (may be more accurate, with measurements possible in three dimensions)
The surgeon should check for associated pathology that may need to be addressed at the time of allograft talar reconstruction:
Osteophyte removal
Ligament reconstruction
Corrective osteotomies
Calcaneal
Supramalleolar
The surgeon determines the optimal surgical approach.
In our hands, this depends on the amount of talus that will be reconstructed.
A portion of the medial talar dome (usually posteromedial) typically warrants a medial malleolar osteotomy.
A portion of the lateral talar dome (often centrolateral) typically necessitates ligament releases (anterior talofibular and calcaneofibular) with or without lateral malleolar osteotomy.
Involvement of the majority of the medial or lateral talar dome, particularly if involving its respective talar shoulder, usually can be performed through an anterior approach without osteotomy by replacing one-third to one-half of the talar dome.
Patient education
This is a complex procedure.
The patient must understand that the intent is to implant allograft tissue.
There is a negligible, but real, risk of disease transmission and possible graft rejection by the host.
There is no guarantee that the procedure will work and a revision procedure may be required, such as arthrodesis, which will eliminate joint motion.
Positioning
Before anesthesia and moving the patient into the operating room, the surgeon should inspect the allograft to be sure it is the correct side (right or left) and for cartilage defects that may be present directly at the site that the graft is to be harvested.
The patient is positioned supine.
For a lateral OLT, a bolster under the ipsilateral hip typically affords better access to the lateral talar dome.
We routinely use a thigh tourniquet.
Approach
As noted earlier, the approach depends on the size and location of the OLT.
For medial OLTs amenable to reconstruction of only a portion of the medial talar dome: direct medial approach, similar to that for open reduction and internal fixation (ORIF) of a medial malleolar fracture, with a medial malleolar osteotomy
For lateral OLTs amenable to reconstruction of only a portion of the lateral talar dome: lateral approach, combining typical approaches for ORIF of a fibular fracture and the extensile exposure for a modified Brostrom procedure
For large medial or lateral OLTs, involving the majority of the medial or lateral talar shoulder: anterior approach, similar to that for ankle arthrodesis or total ankle arthroplasty; typically no malleolar osteotomy is required.
TECHNIQUES
▪ Structural Allograft Reconstruction of Contained Medial Osteochondral Lesions of the Talus
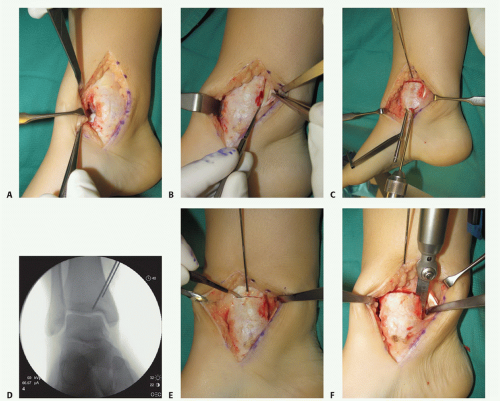
Approach and Oblique Medial Malleolar Osteotomy
Make a curvilinear incision over the medial malleolus, similar to that for ORIF of a medial malleolar fracture.
Protect the saphenous vein and accompanying saphenous nerves.
Anterior ankle arthrotomy (TECH FIG 1A)
Defines anterior joint margin for safe performance of medial malleolar osteotomy
Allows partial visualization of the OLT and allows confirmation that there is no diffuse articular cartilage degeneration
Open the posterior tibial tendon sheath-flexor retinaculum, directly on the posterior margin of the tibia and medial malleolus (TECH FIG 1B). Protect the posterior tibial tendon: It rests in a groove immediately posterior to the tibia and is at great risk with a medial malleolar osteotomy.
Predrill the medial malleolus across the proposed osteotomy site (TECH FIG 1C).
We routinely use two small fragment malleolar screws and predrill with the corresponding drill.
Obtain fluoroscopic confirmation that the drill bits are in the proper trajectory.
Consider passing a tap as well.
Place a Kirschner wire obliquely to define the trajectory of the medial malleolar osteotomy (TECH FIG 1C).
Place it slightly proximal to the desired osteotomy so it can function as a guide but not interfere with the saw (TECH FIG 1D).
Confirm the optimal Kirschner wire trajectory with intraoperative fluoroscopy.
Ideally, the Kirschner wire will extend to the lateral margin of the OLT but with large-volume OLTs that may be too much and unnecessary. However, in our experience, making the osteotomy only to the axilla of the tibial plafond where it meets the medial malleolus will not allow adequate access to perform ideal recipient site preparation.
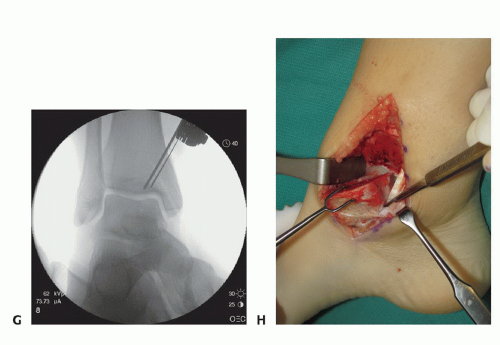
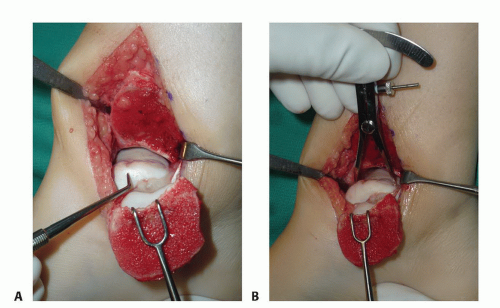
TECH FIG 1 • (continued) G. Fluoroscopic image showing near-complete bone cut. H. Release of posterior tibial tendon sheath from distal medial malleolus to allow mobilization.
Determine a plane for the osteotomy in the anteroposterior (AP) plane that is perpendicular to the longitudinal axis of the tibia. We find it helpful to score the osteotomy in the periosteum from anterior to posterior to determine this level (TECH FIG 1E).
Periosteal stripping is unnecessary; it may be limited to the osteotomy site.
With a microsagittal saw oriented correctly in both planes, the osteotomy is initiated (TECH FIG 1F).
Use cool saline to limit the risk of heat necrosis to the bone.
Obtain intraoperative fluoroscopy shortly after initiating the osteotomy; leave the saw blade in place to confirm proper trajectory. If incorrect, a subtle adjustment is still possible (TECH FIG 1G).
Continue the osteotomy with the saw to the subchondral bone and then complete the osteotomy with a chisel.
A fluoroscopic spot view allows the surgeon to confirm that the osteotomy is appropriate and is not violating the talar cartilage.
There may be some irregularity to the osteotomy at the posterior margin; this is typical as the osteotomy is mobilized. It may be advantageous, as it allows for an interference fit during reduction of the osteotomy and perhaps greater stability.
Reflect the medial malleolus.
The posterior tibial tendon sheath must be released to the distal aspect of the posterior medial malleolus to allow the malleolus to reflect adequately and to gain optimal exposure of the medial talar dome (TECH FIG 1H). Protect the deltoid ligament fibers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree