Osteochondral Autograft/Allograft Transfer
William H. Satterfield MD
Darren L. Johnson MD
History of the Technique
Joint pain and dysfunction are among the most common causes of morbidity and disability in today’s population. Articular cartilage in synovial joints is vital for joint function and longevity. Its unique and highly organized structure, including a predominance of type II collagen, enables it to resist significant force and distribute exceptional loads.1 Chondrocytes are responsible for the synthesis, maintenance, and organization of the cartilage matrix.2 The structure of articular cartilage is divided into four distinct zones superficial to the subchondral bone. The superficial zone consists of flattened chondrocytes and a high relative ratio of collagen to proteoglycans arranged parallel to the joint surface. This confers high tensile stiffness and enables this tangential zone to resist significant shear force.3 The transitional zone is the second zone, which contains more rounded chondrocytes along with higher proteoglycan content and larger diameter collagen fibrils. The middle or radial zone has columns of cells, the largest diameter collagen fibrils, the highest concentration of proteoglycans, and the least amount of water. This zone is arranged more perpendicular to the cartilage surface, and collagen fibrils pass into the basophilic tidemark.4 The deepest zone is the zone of calcified cartilage with fewer cells of smaller volume surrounded by mineralized matrix. This zone separates the articular cartilage from subchondral bone. This complex arrangement of chondrocytes and surrounding matrix provides for the unique tensile and compressive strength of articular cartilage. This tissue undergoes continuous remodeling and responds to both chemical and mechanical stimuli to maintain its function in synovial joints.
Trauma and aging lead to alterations in matrix composition and chondrocyte function. Alterations in the structure and function of articular cartilage lead to symptoms of pain, swelling, stiffness, and mechanical complaints.5 Of paramount importance is the response of cartilage to chondral and osteochondral injury. Investigators have studied this for centuries and have concluded that articular cartilage has limited ability to repair structural damage and does not have the capacity for regeneration.6,8 Most agree that the response to injury depends on whether the injury is superficial or penetrates to subchondral bone. Superficial injuries have been found to remain static over time, lacking any vascular response or ability for tissue regeneration.9,10,11,12,13 Deeper injuries that penetrate subchondral bone disrupt subchondral vessels, leading to a fibrin clot and granulation tissue that fills the defect.14,15
Undifferentiated mesenchymal cells migrate into the defect and proliferate, forming fibrocartilage repair tissue.11,12,16,17 This fibrocartilage lacks type II collagen and thus the durability and strength of normal hyaline cartilage are not reproduced.18 Despite inherent limitations, fibrocartilage repair tissue does distribute load and serve to protect the underlying subchondral bone. Isolated chondral and osteochondral defects typically occur from trauma in young people who maintain a high level of activity19 (Fig. 57-1).
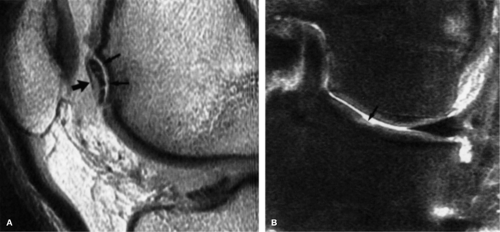
Clinical experience has shown that left untreated many of these lesions do not heal and cause symptoms including pain, swelling, and mechanical dysfunction. Over time these focal defects may lead to joint degeneration and disability. Detection of chondral lesions has increased over the past three decades with the evolution of arthroscopy and magnetic resonance imaging (MRI)20,21 (Fig. 57-2A,B). Curl et al.20 found chondral lesions present in 63% of over 31,000 arthroscopies reviewed with an average of 2.7 lesions per knee. Articular cartilage injuries most often occur with concomitant knee pathology, including meniscal tears, ligament ruptures, and
fractures. Occult subchondral bone bruises have been found in up to 80% of patients with complete anterior cruciate ligament (ACL) tears.22 Johnson et al.23 biopsied the cartilage overlying these bone bruises and demonstrated histologic changes present in these areas of chondral damage. Bobic24 found 77% of 250 knees undergoing anterior cruciate ligament reconstruction for chronic deficiency had some chondral damage to the femoral condyle or tibial plateau. Isolated chondral lesions are known to occur and one report estimated a prevalence of 4% in a series of 312 knees.19,25
fractures. Occult subchondral bone bruises have been found in up to 80% of patients with complete anterior cruciate ligament (ACL) tears.22 Johnson et al.23 biopsied the cartilage overlying these bone bruises and demonstrated histologic changes present in these areas of chondral damage. Bobic24 found 77% of 250 knees undergoing anterior cruciate ligament reconstruction for chronic deficiency had some chondral damage to the femoral condyle or tibial plateau. Isolated chondral lesions are known to occur and one report estimated a prevalence of 4% in a series of 312 knees.19,25
Many other chondral lesions occur in the absence of trauma and are part of the early process of osteoarthritis. The progressive loss of articular cartilage in this disease process occurs secondary to alterations in the cartilage matrix, the chondrocytic response to tissue damage, and the inability of chondrocytes to initiate a proliferative response capable of stabilizing and restoring normal tissue.13,26 While primary osteoarthrosis develops without a known etiology, it becomes much more prevalent with increasing age.
Multiple procedures have been developed to treat focal chondral and osteochondral lesions due to the inability of the articular cartilage to regenerate itself. Increasing interest in these techniques is not surprising considering the prevalence of articular injury in today’s active society and the propensity for these injuries to lead to progressive loss of function. One must differentiate between repair and regeneration when discussing methods of restoring damaged articular cartilage. Repair refers to healing of damaged or lost tissue with new tissue that is similar to hyaline cartilage but does not replicate its structure or function.27 Regeneration means the formation of new healthy tissue that duplicates the lost or damaged articular cartilage precisely.27,28
It has been established that the cartilage’s response to injury is limited in superficial cartilage injury and that
fibrocartilage is formed when injury reaches the subchondral plate. This repair mechanism is something many techniques utilize when treating chondral lesions. Attempts to enhance fibrocartilage repair is the basis of many marrow stimulating techniques that violate the subchondral bone to stimulate a pluripotential cell response. These include Pridie drilling, abrasion arthroplasty, and microfracture of the subchondral bone.29,30,31 Pridie29 described subchondral drilling in 1959, which employed drilling within the lesion to create vascular access channels. Limitations of this procedure include drill access to the lesions and heat necrosis of surrounding bone and cartilage. Magnuson discussed abrasion of the cartilage and underlying bone in the lesion to the depth of bleeding bone as far back as 1941. Many others have expanded on this idea with the emergence of arthroscopy, and motorized shavers are now used, precluding the need for arthrotomy.32,33
fibrocartilage is formed when injury reaches the subchondral plate. This repair mechanism is something many techniques utilize when treating chondral lesions. Attempts to enhance fibrocartilage repair is the basis of many marrow stimulating techniques that violate the subchondral bone to stimulate a pluripotential cell response. These include Pridie drilling, abrasion arthroplasty, and microfracture of the subchondral bone.29,30,31 Pridie29 described subchondral drilling in 1959, which employed drilling within the lesion to create vascular access channels. Limitations of this procedure include drill access to the lesions and heat necrosis of surrounding bone and cartilage. Magnuson discussed abrasion of the cartilage and underlying bone in the lesion to the depth of bleeding bone as far back as 1941. Many others have expanded on this idea with the emergence of arthroscopy, and motorized shavers are now used, precluding the need for arthrotomy.32,33
Microfracture was developed to eliminate the need for drilling and utilizes curved awls to create small tunnels in the exposed bone of the lesion to stimulate a marrow response.34 All of these techniques have been shown to produce fibrocartilaginous repair tissue in the defect that lacks the biomechanical characteristics of normal articular cartilage.18 The goal of treatment for focal traumatic or degenerative lesions is to regenerate tissue that duplicates the biomechanical function and behavior of hyaline cartilage. Marrow stimulation procedures fail to do this and have limited value due to the poor biomechanical properties of fibrocartilage. Attention has turned to more restorative options including periosteal and perichondrial grafting, autologous chondrocyte implantation, osteochondral allografts, and autologous osteochondral transplantation.35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54
Periosteal and perichondrial transplantation are considered by many to be experimental with no proven efficacy for long-term durable repair tissue. Autologous chondrocyte implantation has evolved and is being used more extensively today; however, it requires two operations and comes at significant economic cost. Furthermore, studies vary on the quality of repair tissue generated with some noting predominantly fibrocartilage and others finding a more hyalinelike cartilage in the filled defect.55,56,57
Long-term outcomes have been reported for osteochondral allografts with some deterioration in results over time. Beaver and Gross58 found 75% and 63% good results after 5 and 10 years, respectively. Meyers et al.59 noted similar outcomes using allograft with 77% success after 2- to 10-year follow-up. Documentation of chondrocyte survival after allograft transplantation has been reported, although cell viability decreases with time.60 Issues such as cost, disease transmission, and immunologic reaction continue to plague osteochondral allograft surgery, although it provides a plentiful source of tissue that can be used to match chondral lesions congruently.
Autologous osteochondral autograft/allograft transfer (OATS or mosaicplasty) has emerged as a reproducible technique to resurface chondral and osteochondral lesions in synovial joints. Prior clinical and experimental work has demonstrated that autogenous grafts have a good rate of healing and hyaline cartilage survival in the recipient bed.48,49,50,51 Throughout the past century autologous osteochondral grafts have been used to repair defects in articular cartilage.50,51,61,62,63,64,65 Early autogenous grafts presented the dilemma of choosing a donor site that could be sacrificed without significant morbidity. Further challenges include matching the graft to the lesion and achieving graft stability while maintaining congruency with the surrounding articular surface. Articular cartilage has a variable surface topography within any joint. The goal of resurfacing chondral lesions is choosing a graft capable of re-creating the normal three-dimensional surface anatomy of the damaged area. An additional concern with autologous grafting is the variable thickness of articular cartilage in different areas of the joint, and the “ideal” donor site for osteochondral grafting has not yet been determined. Benefits of osteochondral grafts include a ready-made hyaline cartilage matrix and viable chondrocytes to maintain this matrix.
Hangody et al.52,53,66 proposed the idea of using multiple small cylindrical grafts that would limit the morbidity of donor site harvest. They found that multiple small grafts better enabled progressive contouring to fill the lesion and achieve congruency with the surrounding intact cartilage bed. Experimental work with this concept began in the early 1990s with transplantations on dogs, horses, and cadavers. The technique of mosaicplasty was performed harvesting multiple small grafts from less weight-bearing areas in the patellofemoral joint and sequentially implanting them into defects of the weight-bearing femoral condyles.53,67 Evaluations were made of both recipient and donor areas in the joint. These demonstrated survival of transplanted hyaline cartilage at the graft sites and matrix integration of the transplanted cartilage with the surrounding native cartilage. Areas between grafts were remodeled with fibrocartilage “fill” tissue that integrated with the osteochondral grafts but was not true hyaline tissue. Donor sites were filled with cancellous bone and fibrocartilage repair tissue overlying the lesion.68 This technique was first applied in clinical practice around 1992 for the treatment of focal lesions in the femoral condyles and patellofemoral joint. Once good outcomes were documented, expansion of the initial procedure was made to include treatment of the proximal and distal tibia and talus. More recently some authors have applied this concept to resurface focal injuries of the femoral head and capitellum of the humerus.68
Indications and Contraindications
The natural history of chondral lesions has not been clearly defined. Treatment often is reserved for those lesions considered to be symptomatic and correlating to the patient’s complaints. It has been shown that even small lesions in
active patients can cause significant symptoms19 (Fig. 57-3). On the other hand, focal lesions in low demand patients may undergo repair with fibrocartilage with cessation of symptoms.
active patients can cause significant symptoms19 (Fig. 57-3). On the other hand, focal lesions in low demand patients may undergo repair with fibrocartilage with cessation of symptoms.
Increasing use of arthroscopy and MRI has led to higher detection of partial and full thickness lesions. It is unknown how many of these would otherwise remain asymptomatic and go unrecognized. It is of significant concern what happens to an untreated occult lesion over the lifetime of the joint. Clinical and arthroscopic experience has led to the belief that untreated chondral lesions will progress to larger osteochondral defects over time, leading to clinical symptoms and eventual joint deterioration.69 This has created a role for prophylactic treatment of cartilage lesions found during arthroscopy in order to prevent future joint degeneration.
OATS is a single stage resurfacing procedure for focal defects of the femoral condyles, trochlea, patella, proximal and distal tibia, and talus. It has been used for treatment in some patients for similar lesions in the elbow, humeral head, and femoral head, but these indications have no long-term follow-up.68 It may be used for both focal chondral defects as well as cases of osteochondritis dissecans.70 Ideal lesions are small, focal, full thickness chondral or osteochondral defects measuring 10 to 20 mm2 in diameter.71 Others have extended the indications to include defects of up to 30 or 40 mm2 as it has been shown that the knee can provide this amount of donor tissue without significant morbidity.68 The primary limiting factor when using autologous tissue is the availability of donor tissue. Allograft tissue may be used for more extensive lesions, including larger and deeper defects of cartilage and subchondral bone. The depth of the lesion is also a limiting factor and ideally should be no greater than 6 to 8 mm. Lesions deeper than this make it difficult to reconstruct subchondral bone while achieving coverage and maintaining congruency of the transplanted cartilage surface.
There have been reports using this technique as a salvage procedure for larger lesions,72 although these are best approached with other techniques including bulk osteochondral transfer.48,49,50,51 Traumatic, unipolar, grade IV lesions by the Outerbridge73 classification are the best candidates for OATS. Age limitations are roughly 15 to 50 years and preferably the body mass index is less than 30.
Patients with generalized osteoarthritis, rheumatoid arthritis, or other inflammatory arthritis are not candidates for this procedure. Noncompliant patients should also be excluded as the postoperative regimen is critical for obtaining good outcomes. Other absolute contraindications include tumors, infection, and the lack of an appropriate donor area for the osteochondral grafts. Bipolar lesions present a relative contraindication to performing OATS as does increasing age between 40 and 50 years.
Many cartilage lesions occur in association with other joint abnormalities. These include meniscal tears, ligamentous instabilities, and malalignment of the lower extremity. Meniscectomy leads to increased tibiofemoral contact forces and can create chondral injury or lead to progression when a defect already exists. There is a high incidence of articular cartilage injury in ACL-deficient knees.Acute ACL tears are reported to have a 33% incidence of chondral injury,74 and 79% of knees with chronic deficiency have been found to have cartilage damage24 (Fig. 57-4). Posterior cruciate deficiency leads to increased shear and compression forces, causing chondral injury of the medial femoral condyle and the patellofemoral joint.75,76 Malalignment of either the patellofemoral joint or the tibiofemoral joint leads to abnormal stress concentration and the development of cartilage injury.77 It is imperative that contributing factors associated with articular cartilage disease be treated either staged or simultaneously with the OATS procedure. Failure to address associated joint pathology dooms the cartilage repair as persistent overload and shear stress will continue. The postoperative rehabilitation for mosaicplasty patients may be easily incorporated with that of ligament, meniscal, and realignment procedures such that combined surgery may be successfully performed.68
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree