Chapter 12 Orthotics of the hand
KEY POINTS
 There is no evidence to indicate that static orthoses can prevent deformity from occurring nor correct established deformity
There is no evidence to indicate that static orthoses can prevent deformity from occurring nor correct established deformity Orthotics that immobilise joints may contribute towards a reduction in range of motion. Teaching a hand exercise programme should be considered when providing these.
Orthotics that immobilise joints may contribute towards a reduction in range of motion. Teaching a hand exercise programme should be considered when providing these.INTRODUCTION
Static hand orthotics have been used in rheumatology for many years (Rotstein, 1965). They are recommended for helping individuals manage their arthritis (Scottish Intercollegiate Guidelines Network 2002) and are a popular, commonly used intervention (Henderson & McMillan 2002).
Hand orthotics are used in rheumatology:
PRINCIPLES OF ACTION
RESTING THE JOINT AND PAIN REDUCTION
During periods of acute synovitis, resting affected joints in a biomechanically sound position may reduce joint friction and temperature. At a cellular level this may contribute to a reduction in the pro-inflammatory chemical environment within the joint (Hendiani et al 2003).
IMPROVE HAND FUNCTION
By adding support to proximal joints, applying counterbalanced force to deforming joints and improving biomechanical advantage splints have the potential to improve hand function (Prosser & Conolly 2003). In particular improving support to the wrist can improve grip strength and gross hand function (Nordenskiöld 1990).
Hand orthotics have some biological and biomechanical rationale for their use and action, however, evidence to support and clarify the clinical effectiveness of orthotics in rheumatology is still emerging (Adams et al 2005). This evidence is considered below in regard to five types of orthotics.
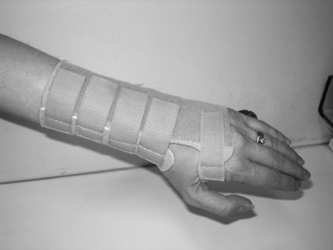
THE WRIST EXTENSION ORTHOSIS
Wrist extension orthoses may be custom-made using either thermoplastic or neoprene material or commercially manufactured from a soft or reinforced fabric with a possible addition of a volar metal support (Fig. 12.1). They may be prescribed to limit wrist circumduction and decrease torque during heavy tasks involving the wrist (Cordery & Rocchi 1998). They may also be used to increase the mobility of the arthritic hand. Wrist extension orthoses can stabilise the wrist in a functionally effective position (10-15 degrees of extension), and facilitate the action of the extrinsic finger flexors to improve handgrip strength (Stern et al 1996). Wrist orthoses provide support to the carpals and wrist joint and several designs of commercial wrist splints have been shown to significantly reduce the electrical activity of the wrist extensors during lifting tasks in people without RA (Stegink- Jansen et al 1997). This may serve to reduce potentially deforming forces on the wrist and carpals.
When worn these orthosis can provide immediate pain relief and significantly reduce pain on functional use of the hand (Haskett et al 2004, Kjeken et al 1995, Nordenskiöld, 1990, Pagnotta et al 2005). Kjeken et al’s (1995) randomised controlled trial analysed splint wear versus non-splint wear over 6 months (n = 69). There was no difference by group on pain, joint swelling, grip or hand motion. However, the control group (n = 33) without splints showed statistically significant improvement in wrist range of motion that was not evident in the splinted group. Both Kjeken et al (1995) and Sharma et al (1991) comment that these wrist orthoses can reduce wrist movement when worn over a number of months and the effects of this should be considered on provision.
In small-scale studies, elastic wrist orthoses have been shown to improve power grip strength for individuals with moderate to severe RA (Backman & Deitz 1988, Haskett et al 2004, Nordenskiöld 1990). However, they have been reported in a small sample (n = 36) to transiently reduce grip strength when first worn and to offer no improvement in grip strength (Stern et al 1996). Although both commercially available and custom made splints have contributed towards improvements in pain and grip strength after four weeks wear in the most able male patients elastic orthoses can hinder maximum grip strength (Sharma et al 1991).
Studies examining hand function have shown that these orthoses are particularly task specific, i.e. they may be able to assist one particular hand skill but reduce another (Pagnotta et al 1998, Stern et al 1996). Functional grip strength has been seen to increase significantly by up to 29% in a woman with RA when these orthoses were worn (Nordenskiöld 1990) yet dexterity, fine finger movement and speed of hand activity have not (Backman & Deitz 1988, Stern et al 1994, 1996).
In summary, wrist extension orthosis have been seen to increase handgrip strength, hand function and provided immediate hand pain relief in some patients. However, they may also contribute to a less dextrous and less mobile hand. There is little evidence to demonstrate the long-term effectiveness of these splints and the quality of evidence available to indicate the clinical effectiveness of these splints is weak (Egan et al 2003).
METACARPAL ULNAR DEVIATION ORTHOSES
These may be small palm-based orthoses or have the additional support of a wrist and forearm component. They may be used early in the rheumatoid disease process to limit the physical factors predisposing the MCPJs to ulnar deviation. By providing a medial force to the proximal phalanges, these orthotics can realign the metacarpals and phalanges during use to improve functional ability of the hand and to prevent further MCPJ ulnar drift and volar subluxation (Adams et al 2005). Therapeutic exercise MCP splints have also been designed to provide exercise options for extrinsic hand extensors and flexors and combat intrinsic plus deformities in the rheumatoid hand (Wijdenes et al 2003).
There is limited evidence for the clinical effectiveness of metacarpal ulnar deviation (MUD) orthoses. In a small repeated measures six months study patients (n = 26) rated them as highly acceptable and satisfactory (Rennie 1996). When worn they realigned the MCPJs and maintained that alignment during functional use of the hand and significantly improved ulnar drift in middle, ring and little finger. They also significantly improved three-point pinch grip strength but did not significantly improve scores on the Sollerman test of hand function (Sollerman 1984), reduce visual analogue pain levels nor improve gross power grip strength. There was no evidence to suggest that they had any long-term effect on correcting MCP joint alignment nor delayed the progression of ulnar deviation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree