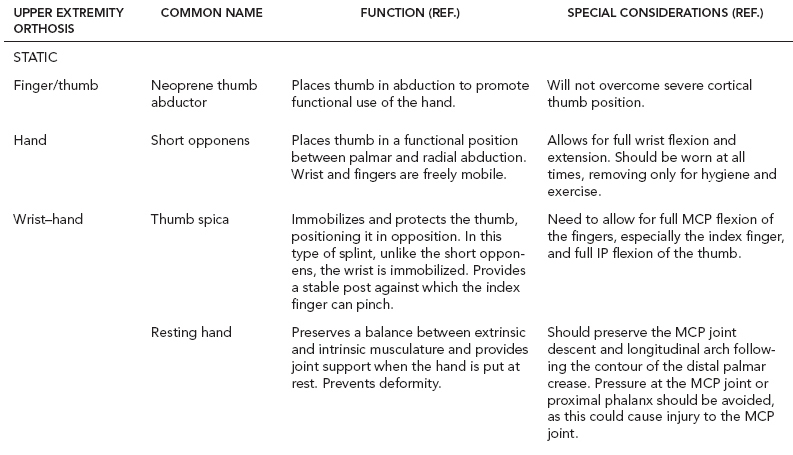
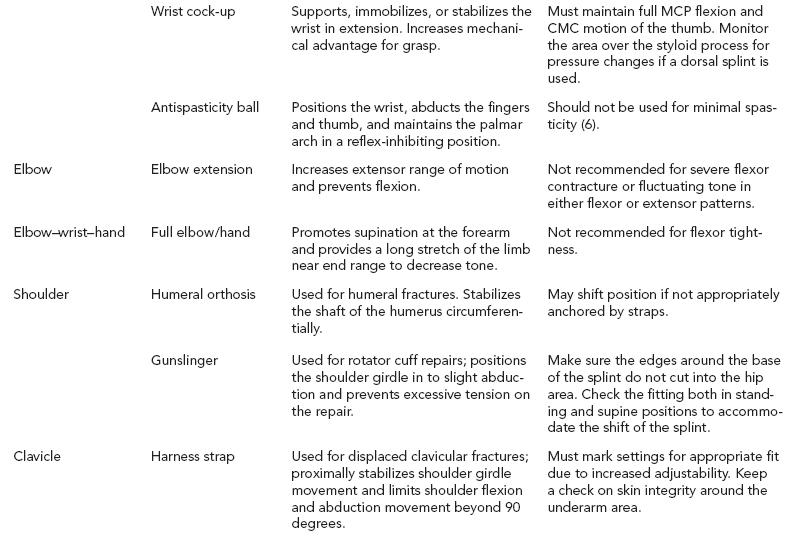
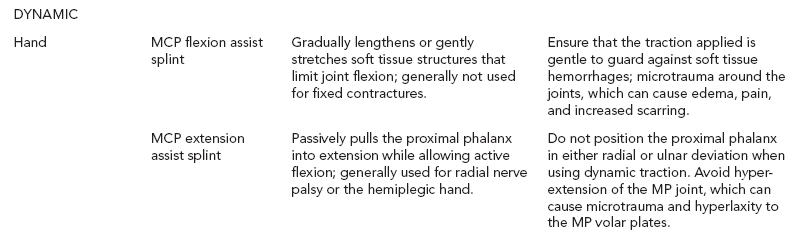
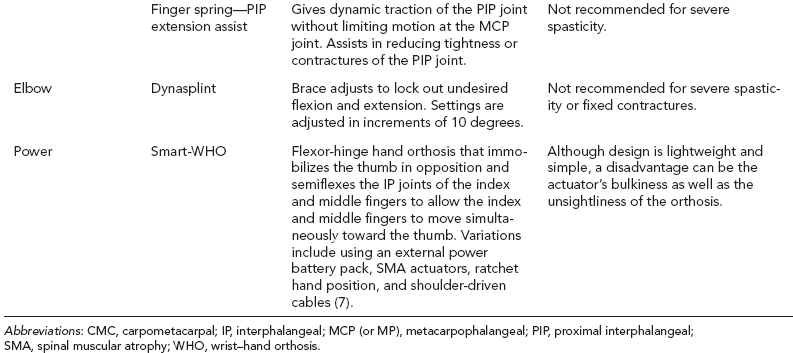
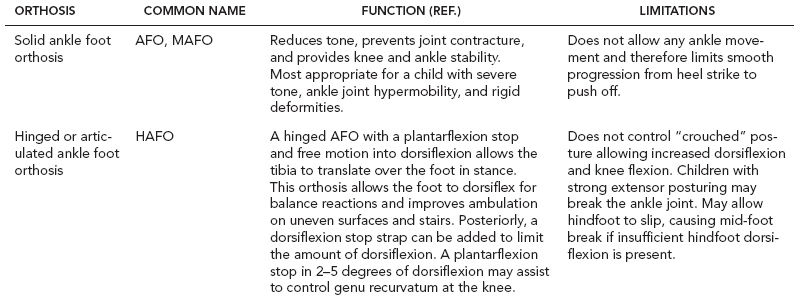
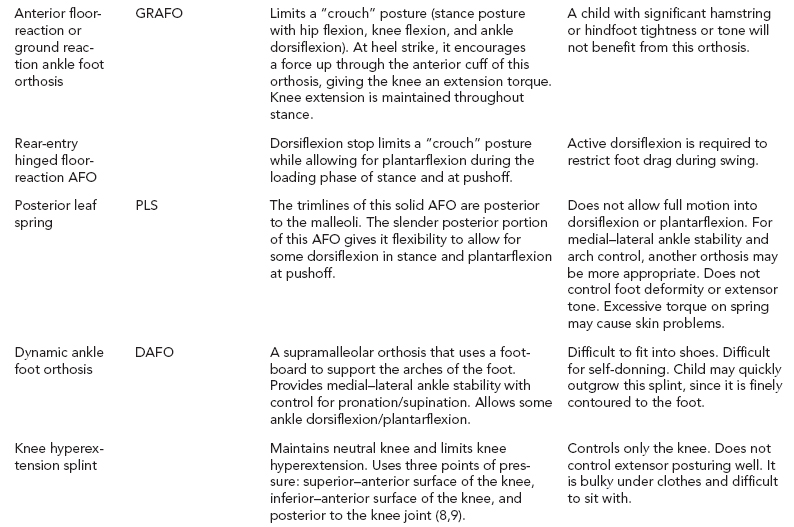
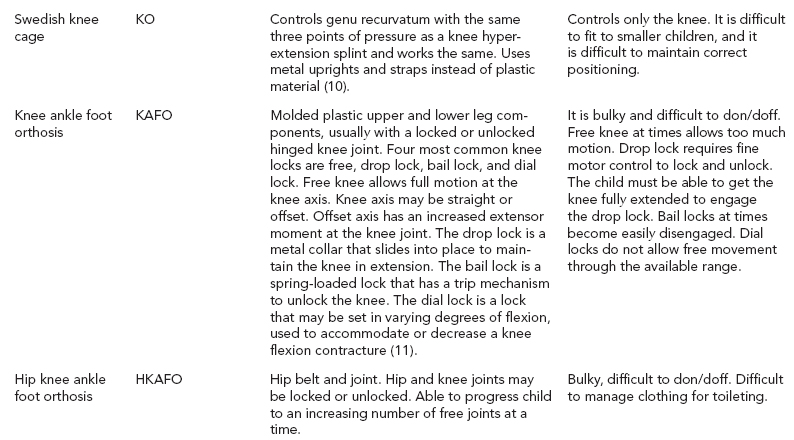
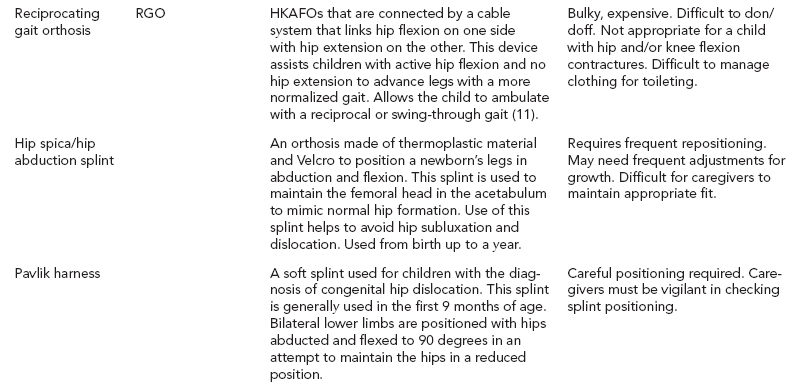
8 ORTHOTICS AND ASSISTIVE DEVICES Elizabeth L. Koczur, Carrie E. Strine, Denise Peischl, Richard Lytton, Tariq Rahman, and Michael A. Alexander Knowledge of orthotic and assistive devices is an important component of rehabilitation practice. Having an understanding of normal upper and lower body movement is fundamental for appropriate recommendation and fabrication of an orthosis. Likewise, clinicians’ understanding of typical language and communication behaviors, literacy skills, and socialization needs is a prerequisite to the recommendation of augmentative and alternative communication (AAC) devices, assistive reading and writing aids, and social media tools. Similarly, the role of orthotic and assistive devices for patients also relates to the overall rehabilitation goal of eliminating, minimizing, or helping them to overcome the limitations imposed by their underlying disorders across areas of physical, cognitive, and psychosocial functions. While some orthotic and assistive devices allow a patient to achieve a degree of independence in a single area of function (such as mobility), pediatric rehabilitation seeks to treat that patient as a whole person across his or her activities of daily living, learning, leisure and recreation, and/or vocational functions. Thus, the role of orthotic and assistive devices needs to be seen not just within the context of independence but also within the context of interdependence with others in a person’s surroundings. Interdependence recognizes that all people have strengths and weaknesses and that all people function most effectively when they do so within social networks that consist of life partners (parents, siblings, children and, often, other relatives); close personal and family friends; teachers and schoolmates; paid workers (such as caregivers, aides, nurses, therapists, physicians, and other health care providers); coworkers; acquaintances; and unfamiliar people. Interdependence occurs when each of us uses our strengths to build relationships that help support our weaknesses. Dr. Al Condeluci in Community & Social Capital asks that we “consider the notion of reciprocity (1). The more you become connected with your community, the more people begin to watch out for each other.” Dr. Condeluci also applies literature from the field of social capital to the rehabilitation vision for people with disabilities: “Social capital refers to the connections and relationships that develop around community and the value these relationships hold for the members… those tangible substances that count for most in the daily lives of people: namely good will, fellowship, sympathy, and social intercourse among the individuals and [others] who make up a social unit.” Thus, an adolescent who has a spinal cord injury (SCI) but can use her head control to independently drive a wheelchair at home, in school, and in the community still cannot participate and contribute to planning the eighth grade class yearbook if her family has not yet been able to buy an adapted van to take her to the Starbucks where her classmates meet to work on the project on Thursday evenings, unless she is perhaps able to participate from home through her head- or speech-controlled computer via Skype, FaceTime, or social media. The key to identifying the most appropriate orthosis, augmentative communication, or assistive technology system is being creative and having a proper understanding of the anatomical, biomechanical, language and communication, and social networking needs of the patient and being sensitive to the patient’s (or the parents’) preferences and desires. The pediatric population adds a further challenge. Early development is heavily based on fine and gross motor skills. Infants and children use these skills to explore and manipulate their environments. Studies have indicated that the inability to master the environment independently may lead to decreased socialization, learned helplessness, and a delay in normal development (2,3). Therefore, an orthosis, augmentative communication device, or assistive learning system should allow for and assist in the growth of the child. Several team members are involved in prescribing, fabricating, and fitting the orthosis, augmentative communication device, or assistive technology system option. The physician, often with input from the therapist, provides patient assessment and a prescription of the recommended device (4). The therapist and/or orthotist are instrumental in its fabrication and fitting. A team including a speech–language pathologist, an occupational therapist, a special educator, and/or a rehabilitation engineer is often beneficial for AAC device recommendations. Finally, the patient and family play an important role in its acceptance and use. If the device is cumbersome and difficult to manage, it will be rejected and find a home on the top shelf in the closet (5). UPPER AND LOWER LIMB ORTHOSES When choosing an orthosis, there are a few key principles to keep in mind. The orthosis should enhance normal movement while decreasing the presence of abnormal postures and tone. It should be simple, lightweight, durable, and strong. It should be easy for the child to use and maintain. Finally, it should augment functional independence. An orthotic device is not successful unless it assists in improving a child’s quality of life. In 2004, a manufacturer new to the rehabilitation field designed a medical device for the hand. The Hand Rehabilitation System was meant for upper limb impairment and paralysis therapy. In addition, the Foot Drop System was presented for those with gait disturbance specific to foot drop impairment. In 2011, Bioness Incorporated developed a device for thigh weakness. The system compliments the foot drop system by aiding and assisting the thigh and knee movement for improved gait performance. Their devices are neuromodulation products that are designed to service populations with multiple sclerosis, traumatic brain injury (TBI), cerebral vascular accident, SCI, and cerebral palsy, and aid in their recovery. Their product can assist both the upper and lower extremity using stimulation to aid in regaining mobility and functional skills so that they can achieve optimal self-care independence, play, and/or work productivity. The upper limb orthosis addresses neurologic impairments, while the lower extremity orthosis focuses on regaining the associated foot drop commonly seen in those clients with central nervous system disorders. Both upper and lower extremity orthoses use mild functional electrical stimulation (FES) to improve loss of function from injury associated with a central nervous system disability. The orthoses can be used in the clinic setting or at home. The overall goal of its use with the involved extremity is to reduce the spasticity, minimize the pain and discomfort during use, increase local blood circulation, prevent muscle atrophy, improve or maintain range of motion in the limb, and reeducate muscle use to enhance functional movement (see the following website for additional information: www.bioness.com/Bioness_for_Hand_Rehab.php). Tables 8.1, 8.2, and 8.3 list some of the more common upper and lower extremity orthoses. Special considerations and limitations are also listed. SHOE INSERTS Many orthopedic and neurologic pediatric disorders have sequelae that require orthotic management. Shoe inserts may be a viable option in many circumstances. There are many commercially available products to control differing levels of impairment in the hindfoot, mid-foot, and forefoot. Heel cups help with shock absorption for joints, heel spurs, bursitis, and tendonitis. In the mid-foot, orthoses assist to maintain the arch of the foot in varying degrees of firmness. Numerous products are also available to control disorders of the forefoot and toes. To relieve metatarsalgia, metatarsal bars are available to unload pressure from the metatarsal arch. Pads are available to help to realign hammer and claw toes, cushion bunions and calluses, and to protect toes from friction and irritation. A limitation to these commercially available products is that many times they do not come in pediatric sizes and must be modified to fit. ORTHOSES FOR POSITIONING, RANGE OF MOTION, AND HEALING Due to immobility, spasticity, and/or abnormal postures, many children are at risk for joint contractures, musculoskeletal deformity, and skin breakdown. Traditionally, caregivers have used pillows and towel rolls to maintain more appropriate postures. Bony areas such as the occiput, scapular spine, coccyx, femoral head, fibular head, and calcaneus are at greatest risk for skin breakdown from prolonged bed rest or maintenance of one position. Gel pads may be used to distribute weight over a larger area. The child may benefit from positioning pieces to maintain neutral positions and decrease pressure on parts of the body. Foam wedges in various lengths and sizes are commonly used for back support to position a child in side-lying. An abduction pillow may be used to decrease scissoring and increase hip abduction. Foam arm and leg elevators help to reduce edema, and foot splints/boots are available to maintain the foot in a dorsiflexed position with relief for the calcaneus to prevent pressure sores. The Versa Form pillow is a semipermanent positioning support. These styrene bead bags are available in a variety of sizes and allow for molding to a child in any position. A vacuum pump is required to remove air from the pillow to make it firm. The bead bags need to be reformed after several weeks of use. This technology gives the practitioner flexibility to change a child’s positioning frequently. It is also a “system” that can be used in multiple environments. TABLE 8.1 UPPER EXTREMITY ORTHOSIS MOBILITY AIDS TRANSFER AIDS There are a number of commercially available patient care lifts to assist caregivers and/or health care professionals with performing safe transfers for children. The Trans-Aid and Hoyer lift are two examples of patient care lifts. They are designed to transfer children from bed to wheelchair, off the floor, onto a toilet, into a car, or from any one room to another. Slings are available with heavy-duty support options to further minimize the effort of the caregiver while maximizing safety during the transfer. There are also institutional lifters available, which offer a 400-pound and 600-pound weight capacity, as well as portable home-care lifts, which are lightweight, portable, and designed for home doorways and narrow halls. Powered overhead transfer lift systems provide families with a unique transfer method. This system enables users to transfer from bed to wheelchair, toilet, or bath using a motorized lift and either manual or motorized lateral movement along a permanent ceiling-mounted track or a free-standing semipermanent rack. However, this transfer system is expensive and usually not covered by insurance. In addition to patient lifts, there are other smaller devices that can assist children with ease of transfers. One option is a transfer board, while another is an overhead trapeze bar attached to an over-bed frame. The most commonly used transfer board is constructed of maple wood measuring approximately 8 inches wide by 24 inches long. It is ideal for all types of transfers (bed, car, bath bench, commode, etc.). Trapeze bars may be attached overhead to bed frames to assist the child with bed mobility skills and positioning changes. The position is individually set and can be altered as needed. Typically, trapeze bars assist with supine to sitting transfers and initiating rolling side to side. They are often appropriate for use initially, but are soon removed after the child’s strength and bed mobility skills improve. STANDERS Numerous passive standing devices are available. These devices offer many potential benefits for the child, including the provision of a sustained muscular stretch, maintenance of trunk and lower limb passive range of motion, facilitation of cocontraction of muscles, decreasing tone, and improvement in trunk and head control. Standers should be used a couple of times a day for up to a total of 1 hour. The child should progressively work to increase tolerance in the standing position. However, passive standing should not take the place of the child exploring his or her environment and body. Three types of standers will be discussed here: supine, prone, and upright. Supine standers go from a horizontal position to approximately 90 degrees upright, depending on the model chosen. Laterals, kneepads, adduction/abduction supports, and head supports all assist to maintain the child’s posture while in this stander. Bilateral upper extremity strengthening can be performed in this position, with or without a tray. However, it does not provide for any upper extremity weight-bearing. A further limitation is that it will not work to improve head and trunk control. This stander is recommended for a child with significant extensor tone and posturing and/or a child with poor or absent head control. It is also preferred over the prone stander for the larger child due to the increased ease in positioning. Prone standers support the child anteriorly. Postural support is supplied through trunk laterals, hip guides, abductor blocks, knee blocks, and shoe holders. These standing devices do come with a chin support to aid children who have limited head control or fatigue easily. However, the child should not be permitted to “hang” on this support; a supine stander is more appropriate if the child lacks fair head control. The stander can be used to improve antigravity head control and promote bilateral upper extremity weight-bearing. Its tray may serve as a functional surface for stimulation. This stander may not be appropriate for some children with increased extensor tone. In these cases, gravity increases the work required for neck and trunk extension as well as shoulder retraction, thus feeding into primitive posturing. Upright standers, such as the Evolv by EasyStand (Figure 8.1) maintain the child in an erect position through supports at the hips, knees, and trunk. Certain standers are available with a hydraulic or manual lift, making positioning of the larger child easier. This stander mimics a normal standing position and permits the child to work on head control and upper extremity strengthening. The seat swings to the side for ease of transfer. FIGURE 8.1 EasyStand Evolv. GAIT AIDS Gait aids are assistive devices designed to improve functional independence and/or expand exercise options through standing and walking. In pediatrics, gait aids assist children to explore and interact with their environment. Improved balance, decreased energy expenditure, decreased impact on joints, improved posture, and decreased pain are all potential benefits of gait aid use. The most common gait aids are canes, crutches, and walkers. Canes are available in different sizes with a variety of handles and supports (ie, straight cane versus quad cane). A quad cane provides a better base for support, but a normal gait cycle is more easily mimicked using a straight cane. A hemicane is a combination of a cane and a walker. It has a four-point base and the largest base of support of all the canes. It gives the greatest amount of stability among the canes, but also encourages the child to lean laterally when ambulating. Crutches generally fall into two categories: axillary and Lofstrand. Axillary crutches are usually constructed of wood or aluminum and have limited adaptability. Some crutches may be modified to offer forearm support to decrease weight-bearing through wrists and hands. The child and family should be cautioned about possible nerve impingement from sustained axillary pressure with improper use. A “Kenny Stick” is an axillary crutch without the underarm piece. In place of the underarm support is a leather armband that fits around a child’s forearm. Lofstrand crutches are much more flexible. They have a variety of forearm cuff styles, including circumferential or half cuff. Functional independence is increased with the use of Lofstrand crutches because the child is able to reach with his or her hands and the circumferential cuff will stay on the forearm. Half cuffs require less reliance on the cuff for balance, but they will not stay on the forearm if the handgrip is released. Handles may be wide and flat, pistol, or rounded. Rounded handles are the most commonly prescribed. The flat, wide handles may be helpful with tonal issues as well as with carpal tunnel inflammation. Pistol grips provide grooves for finger placement. Newer varieties of Lofstrand crutches are lightweight for children who have limited strength or need shock absorption for their joints. Another adjustable option for all crutches is the crutch tip. Crutch tips may be constructed with materials of various flexibilities and in different widths to make the crutches more stable. Tips may include a gel, providing some shock-absorbent qualities. In addition, studded cups, which cover crutch tips, are available to make ambulation in rain and snow easier. Three varieties of walkers are appropriate for the pediatric population: forward, reverse, and gait trainers. Forward walkers are the traditional type of walker. They can be purchased with or without wheels. Children can grip flat handles or use platforms on one or both sides to weight-bear through the elbows and forearms. It should be remembered that forward walkers promote trunk flexion in many children. Reverse walkers, also called posture control walkers, promote an erect posture. The child has increased extension at the trunk and hips when his or her hands are positioned to the sides or slightly in front. A pelvic support can be added to assist with lateral pelvic control and to facilitate trunk extension. Platforms can also be attached to allow forearm weight-bearing. These walkers are widely used in the pediatric population. However, due to increased width, adult-sized children may have difficulty with accessibility. Other accessories available with some walkers are swivel wheels, forearm attachments, hip guides, handwheel locks, baskets, and seats. Gait trainers make ambulation a viable option for children who are unable to ambulate with other aids. Intensive body-weight-supported treadmill training may be an effective intervention for some children with cerebral palsy who are ambulatory (12). A gait trainer is an assistive device that provides significant trunk and pelvic support (Figure 8.2). It consists of a metal frame with adjustable-height metal uprights that support the trunk and arms. Adjustable-height seats, which are either slings or a bicycle-type seat, are attached. The seat is not used to support the entire body weight, but rather to keep the child erect. This gait device has been used to teach a more normal reciprocal gait pattern. It may function as a stepping stone to walking with a walker or crutches. Some limitations of gait trainers include decreased transportability, difficulty with positioning, and decreased accessibility. They are wider and longer than traditional walkers are. Gait trainers do have a place in therapeutic rehabilitation—to provide a child with independent means of ambulation when no other assistive device is appropriate and as a therapeutic tool toward ambulation with a more accessible assistive device. Accessories available with gait trainers are trays, wheel locks, harnesses, forearm supports, and differing lower extremity supports. FIGURE 8.2 Rifton gait trainer. For facility use, weight-bearing and ambulation aids are available. The Lite Gait is a partial weight-bearing gait therapy device. It allows the therapist to control the amount of weight-bearing by supporting the patient in a harness system over a floor treadmill. With other therapeutic modalities, this has been shown to improve ambulation and endurance levels (13). The EVA Walker is a heavy-duty walker that has a manual or hydraulic lift that is easily adjustable for a variety of patients. It allows for significant upper extremity weight-bearing to assist and improve ambulation for more moderately dependent patients. WHEELCHAIRS AND SEATING The degree of limitation in mobility varies across a broad range for people with physical disabilities (5). Over the years, technology related to wheelchair seating and mobility has enhanced the opportunities for people with disabilities. Many more options exist to match technology with the user than ever before. In order to begin the process of matching the child’s needs to a particular wheelchair, it is recommended that a thorough evaluation be made. Many factors contribute to deciding on a particular seating and mobility system for the pediatric population. These include growth, specific disability, medical interventions, and prognosis of future functional and cognitive abilities. Assess the particular needs of the child, collect medical and surgical history, and perform a physical assessment. A multidisciplinary team approach usually works best. Once the assessment is performed, educate the family on various wheelchairs relative to the child’s goals. If possible, simulate the child in as close to the recommended equipment as possible. Finally, determine the particular seating objectives for the child as well as the type of mobility base (4). Every child has a unique set of challenges that will dictate how his or her rehabilitation needs will be met. Proper seating provides stability and support, decreases the likelihood of postural deformities, and enhances upper extremity control. Proximal stability allows for distal control. Within a wheelchair seating system, maintaining proper body alignment is achieved by using various seating and positioning components (14). Seating systems, including both the seat and the back, can be linear, contoured, or molded. Of the three, linear seating systems provide adjustability that allows the seating system to grow as the child grows. Linear seating systems are the most adaptable as the person’s orthopedic needs change. The basic materials consist of plywood for the base, foam (usually viscoelastic, which can vary in density and be combined in layers for pressure relief and distribution) for comfort and pressure relief, and a covering, usually Lycra, Rubatex, or Dartex. Positioners such as laterals, abductors, and adductors are easy to mount on these systems. Contour systems, in contrast to linear systems, conform closer to the actual shape of one’s body. When recommending a contour system, close attention should be given to the growth rate and potential medical interventions, as the shape of the contour may not be an appropriate choice. Custom molded systems provide maximal support and should be considered for children with fixed deformities. Molded systems do not change as the child grows, unless remolding is performed, which is potentially time-consuming and costly. Although this system aids in controlling tone and nicely contours to most deformities, it has the reverse effect of limiting the amount of freedom children have in their seating system. For patients who lack sensation, a variety of cushions exist that assist in alleviating pressure, which will decrease the likelihood of skin breakdown. Cushions fall under several categories, including foam, gel, air, and water (Table 8.4). Cushions should provide pressure relief under bony prominences, provide a stable support surface for the pelvis and the thighs, and function effectively in different climates. They should be lightweight, especially if a person is transferring independently or is a self-propeller, and be durable. Each type of cushion has advantages and disadvantages. FOAM GEL AIR • Lightweight • Lightweight • Provides extremely good pressure relief • Provides a stable base of support • Provides a stable base of support • Various densities available that can improve pressure-relieving qualities • Various densities available that can improve pressure-relieving qualities • Lightweight • Heavy • Heavy • Can be unstable • Conforms to individual shape • Conforms to individual shape • Requires careful monitoring and maintenance Pressure mapping systems are tools used by clinicians to measure interface pressures between two surfaces, such as a seated person and the cushion he or she is sitting on (see an example of a pressure mapping system by Vista Medical at www.pressuremapping.com). A visual output on a computer monitor allows easy viewing and understanding. Using this tool allows clinicians to “diagnose” potential causes of skin ulcers as well as to select a cushion that will provide the most appropriate pressure relief for that patient. Keep in mind that all risk factors, both extrinsic and intrinsic, should be considered before assuming a particular cushion or piece of equipment is causing skin breakdown. POSITIONING COMPONENTS Within a wheelchair seating system, maintaining proper body alignment is achieved by using various positioning components. Evidence supports that children with cerebral palsy should be fitted for wheelchairs that place them in a functional sitting position (15). Lateral supports can be used to encourage midline trunk position when trunk control is poor. Support for those with spinal deformities, such as scoliosis and kyphosis, is carefully evaluated to ensure that corrective forces applied to the individual are tolerable. Scoliosis is managed with the three-point pressure technique. Support pads are placed under the apex of the curve, high on the opposite side and bilaterally at the pelvis. Severe deformities should always be accommodated comfortably, using a seating technique that allows for contact with as much surface area as possible. Usually, when supporting a scoliosis, some degree of tilt (maintaining 90-degree hip angle) is necessary to alleviate some of the effects of gravity on the spine. Also, if the client is not forced to counteract gravity, the lateral supports do not need to be as aggressive and can be made more comfortable and tolerable (16). Chest harnesses assist in stabilizing the trunk by anterior support as well as by preventing forward trunk flexion. Positioning belts are used for pelvic alignment and stabilization. An improperly placed pelvic positioner is more detrimental than no positioner at all. The standard angulation of a pelvic positioning belt is at a 45-degree angle to the sitting surface (3). There are many pelvic positioners available to maintain proper pelvic alignment, such as a double pull padded hip belt, a Hip Grip Pelvic Stabilizer by BodyPoint Inc., and Pelvic Harness by Rifton, to name a few. Subasis bars are used primarily for high-tone patients. Proper placement and position of the bar is critical to the success of the product. Improper positioning can potentially lead to skin breakdown. Additional positioners include abductor pads that reduce or prevent increased adduction and assist in providing proper leg alignment. It should be remembered that abductors are not to be used to block a child from “sliding” out of the wheelchair. This may cause injury to the perineal area (2). Adductors decrease hip abduction and assist in providing proper leg alignment. Shoe holders and ankle positioners help control increased extension or spasms in the lower limbs and correct or prevent excessive internal or external foot rotation. Head position is important for many reasons, including proper visual input, control of tone, and proper alignment for feeding and swallowing. Headrests provide support and positioning for a patient with poor head control due to low tone, active flexion, or hyperextension. They provide posterior and, if necessary, lateral support. They also furnish safety in transport. The size and shape of the headrest depend on individual needs. Total head support can be achieved with the same headrest that allows the child to freely move his or her head to explore his or her environment. When proper seating and positioning components are in place, pediatric wheelchairs provide users with the opportunity to explore and experience the world around them. It encourages social integration as well as enhances the level of involvement in various school and home activities. The majority of wheelchairs can be divided into two main categories: dependent mobility and independent mobility. These categories represent the level of functional mobility the child can achieve. Strollers, recliner wheelchairs, and tilt-in-space wheelchairs typically make up the types of chairs recommended for people who need a temporary means of mobility or who are incapable of independent mobility. Tilt-in-space chairs, such as the Quickie or Zippie IRIS (Figure 8.3) (see website for additional information: www.sunrisemedical.com), are recommended for people who need moderate to maximum positioning when there is little tolerance for an upright position. A reduction of pressure readings at the ischial tuberosities with tilt and recline positioning was shown as a general trend in a study by Pellow (7). Tilt-in-space wheelchairs provide pressure relief by redistributing body weight. The tilt also can assist the caregiver in properly positioning the child in the wheelchair by allowing gravity to assist. Positioning strollers, such as the Kid Kart Xpress, are typically used for younger children in whom independent mobility is less of an issue. Most strollers are also easily transportable. Independent mobility can be achieved by using a manual wheelchair or a power wheelchair. Functional abilities and mobility goals dictate the type of wheelchair recommended. Manual wheelchairs can range from providing minimal support to complete postural support. Manual wheelchairs are lightweight in nature and have a multitude of features that can be adjusted or added to enhance efficient and effective use. Table 8.5 offers a comparative look at the various wheelchair components. Although this is a list of manual wheelchair components, many features can be considered for power wheelchairs as well.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










