7
Orthoses
Essential Concepts
Donald Greg Pitts and Elaine Ewing Fess
• What is the historical perspective for orthotic intervention provided by therapists?
• What factors guide orthotic design?
• What tools and materials are used to fabricate orthoses?
• How do wound healing stages guide orthotic intervention?
• How are orthoses named/classified?
Rationale for Orthotic Application
Reasons for orthotic intervention directly correlate with injury-specific and/or disease-specific patient diagnoses. In a review of published literature spanning over a fifty-year time frame, twenty-seven different rationales for orthotic intervention were identified; with the six most frequently cited reasons, listed in rank-order, including to (1) increase function; (2) prevent deformity; (3) correct deformity; (4) protect healing structures; (5) restrict motion; and (6) allow tissue growth/remodeling.1
Materials and Equipment
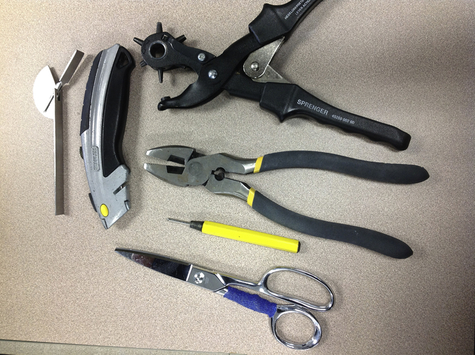
Basic equipment for fabricating orthoses includes, but is not limited to, a water heat pan, several pairs of sharp scissors, a heat gun, a rotary hole-punch, box cutter, wire cutters, an awl, and a goniometer (Fig. 7-2). Scissors that are used for cutting Velcro should be segregated and used only for this task since they tend
to become “gummy” from the Velcro adhesive, making them unsuitable for cutting heated thermoplastic materials.
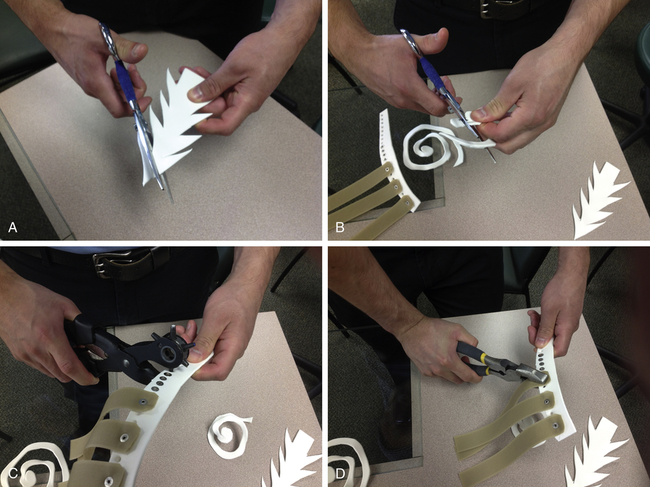
Ergonomic use of tools and equipment is essential to producing orthoses that are professionally assembled and finished. Simple practices, like rounding orthotic corners and strap-end eliminates uncomfortable pointed ends and edges (Fig. 7-3).

Factors That Allow Orthoses to Work Effectively
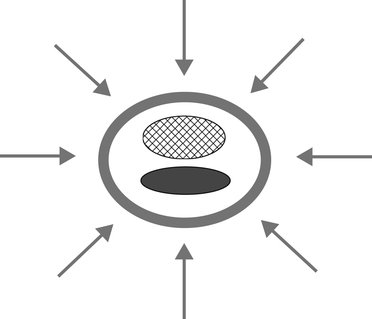
In mechanical terms, orthoses function either as lever systems that apply three-point pressures in reciprocal patterns (Fig. 7-4); or they apply two-point pressures in opposing patterns (Fig. 7-5). The vast majority of orthotic designs utilize three-point pressures. Although less frequently used, the most common reasons for applying two-point pressure orthoses are to support stable fractures (for example, humerus; metacarpals) or to support healing/repaired pulleys of digital flexor tendons.

See Table 7-1 for mechanical principles for creating effective orthoses.2
TABLE 7-1
Mechanical Principles of Orthotic Fabrication and Fit
| Principle | Implication |
| 1. Understanding force systems | Know when to use three-point pressure orthotic designs and when to use two-point pressure orthotic designs. |
| 2. Increase the area of force application | Wider orthotic components decrease pressure and increase comfort. |
| 3. Increase mechanical advantage | Longer orthotic components decrease pressure and increase comfort. |
| 4. Use optimum rotational force | Application of corrective force is most efficient at a 90-degree angle. |
| 5. Consider torque effect | The further away from the main focus joint a force is applied, the greater the torque on that joint will be. Be careful to not exceed tissue and/or pain thresholds. |
| 6. Control reaction at secondary joints | Prevent subluxation of joints proximal and/or distal to primary focus joints within longitudinal rays. |
| 7. Consider reciprocal parallel force effect | • Middle reciprocal pressure in a three-point pressure orthosis equals the sum of proximal and distal forces. • Monitor the area under middle-reciprocal-pressure components carefully for soft tissue breakdown. Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|