Operative Treatment of Thumb Carpometacarpal Joint Fractures
John T. Capo
Joshua T. Mitgang
Colin Harris
DEFINITION
The first carpometacarpal (CMC) joint comprises the thumb metacarpal base and the trapezium.
The thumb CMC joint is vital to the function of the hand, and injuries can result in pain, weakness, and loss of grip or pinch strength.
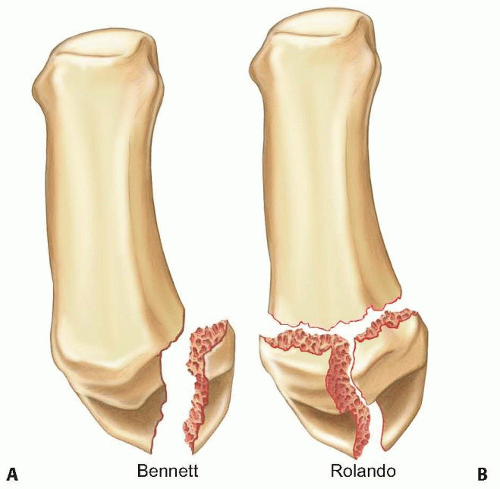
Two fracture-dislocation patterns commonly result from trauma to the thumb CMC joint: Bennett and Rolando fractures.
Bennett fractures are intra-articular fractures in which the metacarpal shaft is radially displaced by the pull of the abductor pollicis longus (APL) tendon, leaving an intact ulnar fragment at the base of the thumb metacarpal that is held reduced by the strong volar beak ligament (FIG 1A).
ANATOMY
Understanding the deforming forces in these fracture-dislocations is important when deciding on treatment options and determining prognosis.
The thumb metacarpal serves as the site of attachment for several tendons, including the APL at the proximal base, the adductor pollicis distally, and the thenar muscles volarly.15
The articular surfaces of the thumb metacarpal base and trapezium resemble reciprocally interlocking saddles and allow motion in many planes.11,15
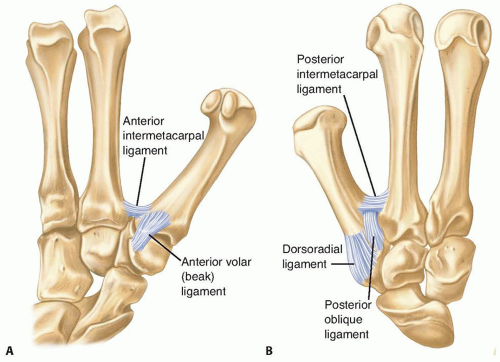
Joint stability is maintained by five primary ligaments: the anterior volar (beak), the posterior oblique, the dorsoradial, and the anterior and posterior intermetacarpal ligaments (FIG 2).7
Zone 2 represents the central portion of the joint that is normally loaded.
Zone 1 includes the volar aspect of the joint.
Zone 3 involves the dorsal aspect of the joint.
The trapezium has several important adjacent articulations. These include the first metacarpal base, the radial aspect of the second metacarpal base, the scaphoid, and the trapezoid (along with the trapezium, these last two make up the scaphotrapeziotrapezoid [STT] joint) (FIG 4).
PATHOGENESIS
Bennett fractures occur when the partially flexed thumb metacarpal is axially loaded, resulting in a Bennett articular fragment (the volar ulnar portion of the metacarpal base) and the remainder of the metacarpal that displaces dorsally, proximally, and radially.
Rolando fractures result from a similar injury mechanism and may have a variable degree of comminution at the base of the thumb metacarpal.
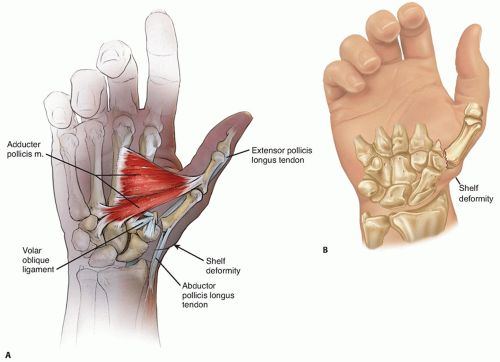
In Bennett-type fractures, the thumb metacarpal shaft is displaced dorsally and proximally by the pull of the APL at the metacarpal base, the extensor pollicis longus (EPL) which inserts more distally, and angulated ulnarly by the APL (FIG 5A).15
Rolando-type fractures are subject to the same deforming forces, except that the APL can sometimes displace both the shaft and the dorsoradial basilar articular fragment.
Due to the deforming forces that act on the fracture fragments, both injury patterns are usually unstable and difficult to reduce and stabilize by closed means.
NATURAL HISTORY
Nonoperative treatment is generally reserved for nondisplaced fractures. There is a low likelihood of maintaining reduction using closed means in displaced fractures.
Residual subluxation of the metacarpal shaft leads to basal joint incongruity and the potential for developing
posttraumatic arthrosis.3 In addition, residual intra-articular step-off greater than 1 mm may predispose the patient to the development of arthrosis.6,18
PATIENT HISTORY AND PHYSICAL FINDINGS
Most of these fractures occur with direct trauma to the thumb tip, often from a fall or sports-related injury.
The history should reveal whether the patient had preexisting basal joint arthritis, which is common and will affect treatment options and expected results.
Common physical examination findings include tenderness and ecchymosis surrounding the thumb CMC joint, crepitus with attempted motion, instability, and a “shelf” deformity resulting from displacement of the metacarpal shaft dorsally (FIG 5B).16
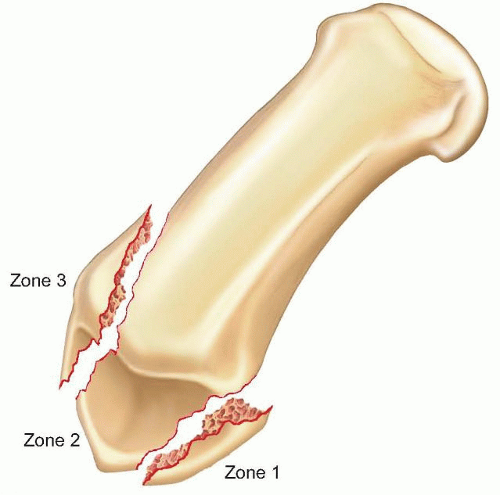
FIG 3 • The three zones found in fractures of the first metacarpal base. The central zone 2 is critical for joint stability and if involved usually requires open reduction and internal fixation.
Metacarpal subluxation or dislocation represents an unstable fracture.
Range of motion is decreased and may be associated with crepitus. Adjacent joints may also have arthrosis and decreased range of motion.
It is important to perform a complete neurovascular examination and to search for associated pathology such as wrist ligamentous injuries.
Neurovascular injuries are uncommon, but compartment syndrome should be suspected in higher energy injuries. A recent case study described the first documented case of
thenar compartment syndrome from a thumb metacarpal base fracture.20
Function of the EPL, flexor pollicis longus (FPL), and extensor pollicis brevis (EPB) should be confirmed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and oblique images of the hand should be obtained, although the oblique plane of the thumb in relation to the hand may make these images difficult to interpret.
A true lateral view, advocated by Billing and Gedda,1 is obtained with the hand pronated 20 degrees and the thumb positioned flat on the cassette. The x-ray beam is tilted 10 degrees from vertical in a distal to proximal direction (FIG 6B).
Radiographs of the contralateral, uninjured basal joint are helpful in certain cases as a template for reconstruction.
Computed tomography may be indicated if a significant amount of articular comminution is present or when plain films inadequately demonstrate the pathology.
A traction view may be helpful in Rolando-type fractures (FIG 6C).
Fluoroscopy alone should be used with caution in ensuring anatomic reduction, as this has recently been shown to be less accurate than plain x-rays or direct visualization.4
DIFFERENTIAL DIAGNOSIS
Bennett-type fracture
Rolando-type fracture
Basal joint degenerative joint disease
STT joint arthrosis
Thumb CMC joint ligamentous injury
Trapezial body fracture
De Quervain tenosynovitis
NONOPERATIVE MANAGEMENT
Nondisplaced, minimally comminuted fractures may be treated with closed reduction and thumb spica casting, but precise molding of the cast and close observation for fracture displacement are necessary.
In a Bennett fracture, closed treatment may be indicated if there is minimal displacement between the volar ulnar fragment and the metacarpal shaft. Most importantly, a concentric reduction of the metacarpal base and the CMC joint in Bennett fractures must be maintained.6
Several factors make closed treatment of these intra-articular fractures problematic and worsen results:
Difficulty in providing accurate three-point molding of the thumb metacarpal
Treatment of patients 4 or more days after the initial injury
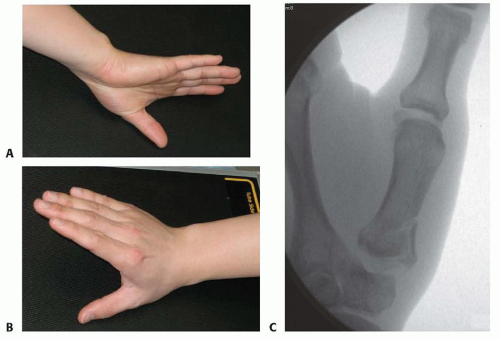
FIG 6 • A. An ideal AP view of the thumb and CMC joint is taken with the forearm hyperpronated and the dorsum of the thumb on the cassette. B. A true lateral view of the CMC joint is obtained with the radial aspect of the thumb on the cassette and the other fingers clear of the x-ray beam. C. A fluoroscopic view of a Rolando fracture with traction applied. Distraction at the CMC joint helps to delineate the fragments at the base of the metacarpal. (Copyright John Capo, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access