Operative Treatment of Metacarpal Fractures
José M. Nolla
DEFINITION
Hand metacarpals can fracture at their base, shaft, neck, or head. Such fractures can lead to shortening, rotation, or angulation.
Metacarpals provide a base for each finger and injury to a metacarpal can severely compromise independent digital function.
Treatment strategy for metacarpal injuries must consider the ability of the human hand to compensate for such injuries.
ANATOMY
The thumb metacarpal (first) is highly independent and is stabilized by its carpometacarpal (CMC) joint and supporting muscles.
The other four metacarpals (second to fifth) are tightly connected through the CMC joints proximally and the deep transverse metacarpal ligaments distally. These ligaments connect the volar plate and head of each metacarpal to the adjacent metacarpal. The ligaments also have a significant role in preventing shortening and rotation of fractures of the central (third to fourth) metacarpals (FIG 1).
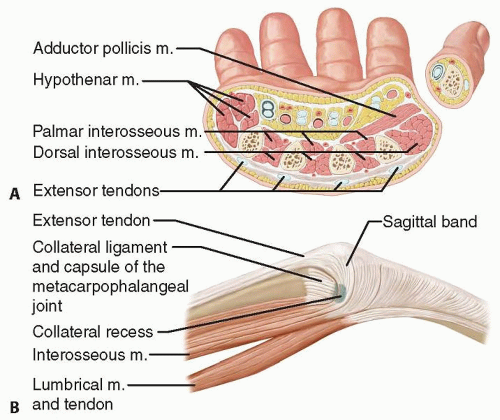
The thumb metacarpal has a round cross-sectional shape, whereas the other metacarpals tend to have a triangular shape with a dorsal, anterolateral, and anteromedial facets (FIG 2A).
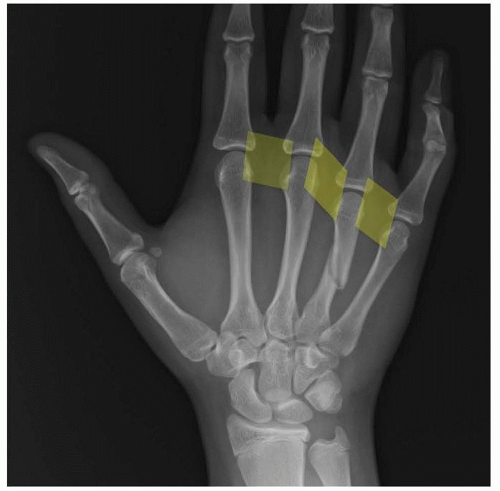
FIG 1 • The deep transverse metacarpal ligaments (shaded yellow) protect the fractured metacarpal from excessive shortening and rotation.
The dorsal and volar interosseous muscles cover the ulnar and radial surfaces of each metacarpal (see FIG 2A). These muscles provide blood supply to the metacarpals but are also at risk of contracture in cases of injury leading to severe hand edema and compartment syndrome.
The deep palmar arch and the deep branch of the ulnar nerve lie just volar to the metacarpals and are at risk during fracture and surgery.
On either side of the metacarpal head, there are fossae and tubercles that create a recess from which the collateral ligaments of the metacarpophalangeal (MP) joint arise (FIG 2B).
The extensor tendons lie just superficial to the base and shaft of each metacarpal. At the level of the metacarpal head, they contribute to the dorsal extensor apparatus of each finger (see FIG 2B).
PATHOGENESIS
Axial load is the most common injury mechanism for a metacarpal fracture. Due to the normal curvature of the fifth metacarpal, such an axial load will include a bending
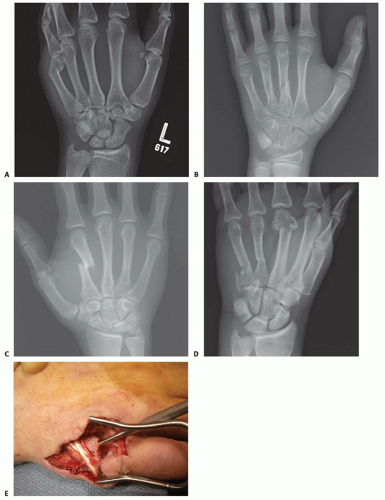
component and lead to an apex dorsal fracture at the neck, also known as a boxer’s fracture (FIG 3A).
Axial loads may also be transmitted proximally on the metacarpal and lead to a CMC fracture-dislocation.
Torsional injuries will lead to spiral oblique fractures (FIG 3B).
Bending injuries from direct impact may lead to short oblique or transverse metacarpal fractures (FIG 3C). The addition of butterfly fragments and comminution is dependent on a combination of additional loads.
Crush injuries can lead to comminuted fractures with significant soft tissue injuries and a heightened risk of compartment syndrome (FIG 3D).
NATURAL HISTORY
Metacarpal fractures are mainly affected by shortening and rotation. The effect of these two components is minimized in the central metacarpals due to the stabilizing effect of
the deep transverse metacarpal ligaments and the bordering intact metacarpals. This stabilizing effect is lost in cases of multiple metacarpal fractures and more severe injuries (see FIG 3D).
Shaft fractures of the third and fourth metacarpals tend to do well with minimal intervention. Border metacarpals are more prone to shortening and rotation.
Every 2 mm of shortening of the metacarpal can lead to a 7-degree lag at the MP joint.12
Fractures of the metacarpal neck typically result in apex dorsal angulation, which may lead to significant shortening. The increased mobility afforded by the ulnar CMC joints allows more tolerance of angulation in the ulnar metacarpals (fourth and fifth). Whereas some have accepted up to 70 degrees, most authors have recommended intervention if the angulation exceeds 30 to 40 degrees.4,6,9 The radial metacarpals (second to third) have stiffer CMC joints, and correspondingly, the tolerance for angulation is reduced to only 10 to 15 degrees.7
Thumb metacarpal extra-articular base and shaft fractures can easily tolerate 30 degrees of angulation due to its highly mobile CMC joint.1
Fractures of the metacarpal head with a significant gap or step-off, or fractures that involve a significant portion of the articular surface, should be considered for open reduction and stabilization.2
PATIENT HISTORY AND PHYSICAL FINDINGS
History: Note the mechanism of injury, time since injury, and any treatment received so far. Also, note the age, vocation, and hobbies of the patient. Comorbidities should also be recorded.
Inspection: The skin needs to be checked for any signs of an open fracture. A small laceration near the MP joint may be the only sign of a “fight bite” injury which requires urgent débridement to prevent joint and bone infection (FIG 3E). Also, note digit malrotation and extension lag at the MP and proximal interphalangeal (PIP) joints. A severely edematous hand may signal compartment syndrome or an internal degloving injury.
Palpation: The neurovascular examination should include checking activation of the first dorsal interosseous muscle to confirm activity of the motor branch of the ulnar nerve. Tense compartments and pain with passive motion may signal a developing compartment syndrome.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The posteroanterior (PA) view can show shortening, especially relative to the adjacent metacarpals. Fracture angulation can be seen on the lateral view but is often best seen on the oblique view. Fractures of the base of the fifth metacarpal are best seen on the pronated oblique view.
Specialized views of the metacarpal head can show the volar aspect (Brewerton) or the dorsal aspect (skyline).
Traction views in the anesthetized patient may help elucidate pattern and extent of injury.
Computed tomography (CT) scan can help in extensively comminuted fractures or articular injuries.
DIFFERENTIAL DIAGNOSIS
Open fractures
Fight bite with bacterial inoculation of the MP joint
Pathologic fractures
NONOPERATIVE MANAGEMENT
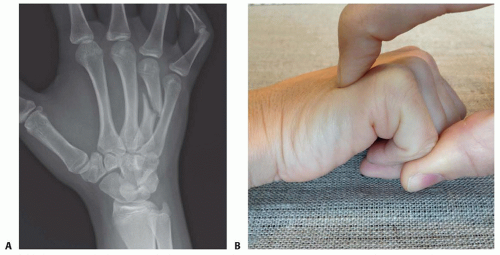
Shaft fractures that are not displaced and not angulated can be treated with a brief period of immobilization followed by protected activities. Those with angulation of greater than 20 degrees (30 on the small finger) deserve an attempt at closed reduction (FIG 4A).
Acute (<7 to 10 days), isolated fourth or fifth metacarpal neck fractures angled more than 30 to 40 degrees benefit from reduction and immobilization. Only 15 degrees should be accepted for the second or third metacarpals. A dorsally directed force can be applied to the head of the metacarpal through the Jahss maneuver (FIG 4B) or directly on the metacarpal head (FIG 4C).
The position of the MP joint during immobilization for treatment of fifth metacarpal neck fractures has not been
shown to affect the final mobility of the MP joint.14 It is often easier to immobilize the MP joint in extension while applying direct pressure on the metacarpal head (FIG 4D,E).5
Be aware that prolonged immobilization of MP joints in extension may lead to collateral ligament contracture and result in difficulty regaining MP flexion.
SURGICAL MANAGEMENT
Indications for surgery include open fractures, open joint injuries (such as fight bites), malrotated fractures, unstable fractures, and those associated with other injuries that need surgery such as tendon or nerve lacerations.
Relative indications for surgery include extensor tendon lag, metacarpal shortening, prominence of the metacarpal head in the palm, multiple metacarpal fractures, and intraarticular fractures.
Contraindications for internal fixation include grossly contaminated fractures and infirmed patients.
Contaminated fractures should be débrided and temporarily stabilized until definitive fixation can be performed.
Percutaneous pins have the advantage of minimizing soft tissue injury. However, the fracture must be reducible through closed means.
Percutaneous pins can be placed in a retrograde direction from distal to proximal entering the metacarpal through the collateral recesses. This technique allows stabilization of proximal neck or shaft fractures. Flexion of the MP joint facilitates access to the collateral ligament recesses.
Antegrade pin fixation (bouquet pinning) from proximal to distal can provide stability to shaft and neck fractures. This technique has the advantage of avoiding the MP joints altogether, which, if enough stability is present, may even permit early motion. In the treatment of neck fractures, it may lead to less MP stiffness compared to retrograde (collateral recess) pinning.10 However, placement of the antegrade wires can be more challenging technically.
There are many occasions when the fracture cannot be easily reduced through closed techniques and open approach is required. Such an approach allows for an anatomic reduction and placement of stable fixation. However, it also introduces a degree of soft tissue insult.
Screws provide rigid fixation while at the same time minimizing implant bulk. However, they are appropriate only for long oblique or spiral fractures whose lengths are at least twice the diameter of the bone at the level of the fracture.
Plates provide rigid fixation in short oblique and transverse fractures but require significant soft tissue dissection. Rarely, the hardware will have to be removed once the fracture is healed.
External fixators allow treatment of more complex fractures while minimizing soft tissue injury but do not allow precise control of the fracture fragments. External fixation may be desirable in the treatment of injuries with massive soft tissue disruption.
Preoperative Planning
The fracture itself and its character will dictate much of the approach to the fracture. However, respect of the soft tissue is of utmost importance.
Crush injuries with significant degloving of the soft tissues may be best managed with limited or percutaneous approaches to limit further embarrassment of the tissue envelope.
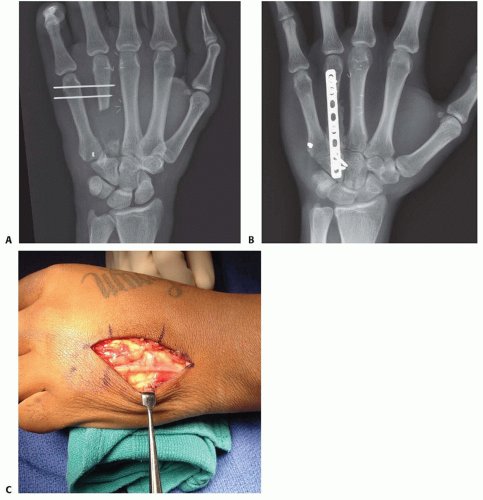
Grossly contaminated wounds, or those with tenuous soft tissues, may be best managed initially with limited fixation until more definitive fixation can be performed (FIG 5A).
Bone grafting may also need to wait until the soft tissues have stabilized (FIG 5B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree