Operative Treatment of Metacarpal Fractures
Lance A. Rettig
Thomas J. Graham
INDICATIONS/CONTRAINDICATIONS
The majority of isolated metacarpal fractures are effectively managed with closed reduction and splint immobilization. However, a subset of metacarpal shaft or neck fractures cannot be reduced by closed means or are unstable after reduction. For these fractures, operative treatment is a consideration or a requirement. Simple extra-articular diaphyseal metacarpal fractures may be amenable to transcutaneous pin fixation or intramedullary stabilization. If the fracture is not reducible by closed reduction, or if pin stabilization fails to maintain adequate stability, open treatment is required. Indications for open reduction and internal fixation include open fractures, injury to multiple metacarpals, intra-articular displacement, and fractures associated with significant soft-tissue injury or segmental bone loss. The decision to consider operative stabilization may be influenced by age and hand dominance along with vocational and avocational demands. Few true contraindications exist to operative fixation of metacarpal fractures. Age is a consideration in young patients with open physis or elderly with severe osteopenia.
PREOPERATIVE PLANNING
Physical examination should focus on assessing rotation, shortening, and angulation of the digit resulting from the metacarpal fracture. The majority of metacarpal fractures can be adequately evaluated with plain film radiographs. Anteroposterior, lateral, and oblique hand x-rays are important to help characterize the fracture and define the metacarpal anatomy. A Brewerton view may be helpful in the evaluation of the fractures of the metacarpal head. Semipronated or semisupinated oblique
projections are of value when assessing injuries of the border rays, especially possible carpometacarpal (CMC) fracture-dislocations. CT imaging of the hand may be beneficial in these instances to evaluate for concomitant hamate injury or subluxation of the CMC joint.
projections are of value when assessing injuries of the border rays, especially possible carpometacarpal (CMC) fracture-dislocations. CT imaging of the hand may be beneficial in these instances to evaluate for concomitant hamate injury or subluxation of the CMC joint.
SURGICAL TECHNIQUE
The operating room setup is standard for surgery of the hand. The patient is supine with the affected extremity on a hand table. A padded pneumatic tourniquet encircles the proximal brachium. The anesthesia choices range from local (wrist block) and regional (including axillary and Bier block) to general endotracheal anesthesia regardless of closed versus open treatment. Prior to prepping and draping, it may be helpful to perform a fluoroscopic examination of the metacarpal injury. Traction and manipulation of the involved ray under the fluoroscan can provide information about fracture reduction and detail about the pathoanatomy. This step is important in determining whether the fracture can be managed with closed reduction and pinning or by open methods. Further defining the fracture in this manner may also assist in placement of the skin incision when open treatment is indicated.
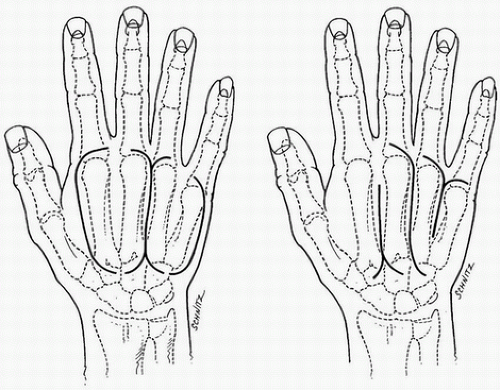
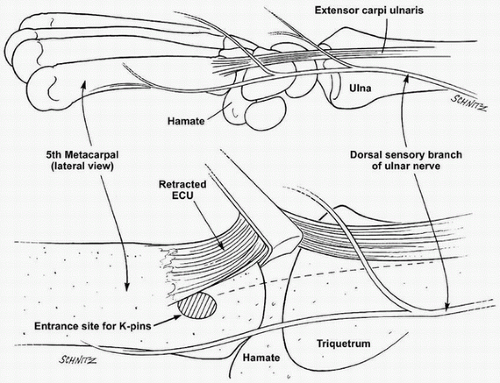
When an open approach is required, skin incisions are positioned slightly offset from the metacarpal to reduce the risk of scarring of the extensor mechanism (Fig. 5-1). Following the skin incision, blunt dissection is undertaken to identify branches of the superficial radial and ulnar nerves. Extreme caution should be undertaken when approaching the most ulnar ray, particularly the more proximal aspect of the metacarpal. Careful handling of the dorsal ulnar sensory nerve is critical in the approach to the small finger metacarpal. This is especially important when performing intramedullary pinning (Fig. 5-2).
Exposure of the fracture is undertaken by incising the periosteum longitudinally. Subperiosteal dissection will help define the plane of the injury. In cases of long oblique diaphyseal or comminuted segments, extreme care should be undertaken to avoid additional compromise of the bone integrity. The fracture site is inspected and irrigated to ensure that no intervening soft-tissue structures are blocking reduction. This step is particularly important in cases of delayed treatment when scar or granulation tissue may impede anatomic restoration. Maintenance of exposure is achieved with the use of self-retaining retractors and Hohmann- or Bennett-type instruments.
Fracture reduction is undertaken by a combination of longitudinal traction and derotation. In certain cases, realignment of the metacarpal may be facilitated by performing a Jahss maneuver. By positioning the MCP joint in a flexed posture, the proximal phalanx can be used as a lever to assist with addressing rotational deformity. A sharp tenaculum will assist with reduction and provisionally stabilize the fracture. Once anatomic reduction has been achieved, Kirschner wires may also be utilized to temporarily stabilize the metacarpal. Clinical assessment of digital alignment is assessed by passively positioning the digits into flexion to ensure there is no digital overlap.
Implant selection is largely based on the plane and configuration of the fracture. Although each fracture has a unique personality, there are some basic tenets to fixation of these injuries that exist.
Implant choices include lag screw fixation alone or combined with plate stabilization. Plate fixation may be used in compression or as a neutralization device. Other options not discussed in this chapter include wiring techniques or external fixation.
Implant choices include lag screw fixation alone or combined with plate stabilization. Plate fixation may be used in compression or as a neutralization device. Other options not discussed in this chapter include wiring techniques or external fixation.
With indications established, the choice of operative fixation becomes the next consideration. For the purposes of this chapter, fracture treatment will be divided into closed treatment with pin stabilization and open reduction internal fixation.
CLOSED TREATMENT WITH PIN STABILIZATION
A myriad of configurations and techniques have been described for closed reduction and pinning of metacarpal fractures. These have included cross-pinning, transverse pinning to an adjacent intact metacarpal, intramedullary pinning, or combination of these patterns. Collateral recess pinning and bouquet pinning are described because of the technical challenge inherent in these fixation methods and their unique utility.
Collateral Recess Pinning
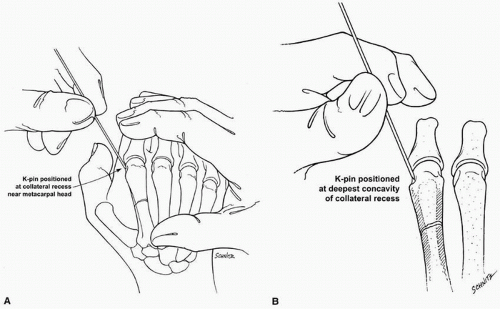
This method is often utilized for reducible transverse diaphyseal fractures and metacarpal neck injuries. Fracture extension into the collateral recess and degree of comminution may preclude the use of this technique in certain cases. Provisional closed reduction of the fracture is performed. The metacarpophalangeal (MCP) joint of the fractured metacarpal is flexed to 90 degrees. A 0.045-inch or 0.062-inch Kirschner pin is manually positioned percutaneously onto the radial or ulnar collateral recess while maintaining the flexed posture of the MCP joint. The initial pin placement is completed by feel or stereognosis (Fig. 5-3). Fluoroscopy is used to confirm appropriate placement at the deepest concavity of the collateral recess. A lateral view is also completed to evaluate the position of the wire in the sagittal plane.
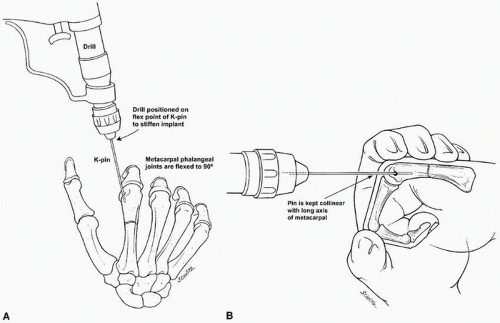
Assessing initial pin position is critical to minimize the number of additional passes of the wire required to achieve fixation. Once the pin has been manually positioned in the collateral recess, the driver is positioned over the wire. The pin is captured at its flex point nearest the leading end of the Kirschner wire (Fig. 5-4A). The pin is then advanced into the shoulder of the metacarpal
while the appropriate angle is established. One must consider the relationship of the pin to the metacarpal in both the sagittal and frontal planes prior to intramedullary placement of the wire. The Kirschner pin needs be positioned collinear with the long axis of the metacarpal within the sagittal plane (Fig. 5-4B). Alignment in the coronal plane requires that the pin be placed at an angle so that the leading edge of the wire crosses the fracture site within the confines of the intramedullary canal.
while the appropriate angle is established. One must consider the relationship of the pin to the metacarpal in both the sagittal and frontal planes prior to intramedullary placement of the wire. The Kirschner pin needs be positioned collinear with the long axis of the metacarpal within the sagittal plane (Fig. 5-4B). Alignment in the coronal plane requires that the pin be placed at an angle so that the leading edge of the wire crosses the fracture site within the confines of the intramedullary canal.
Fluoroscopy is repeated to check the overall alignment of the pin and its insertion site. The fracture site is visualized to check reduction. Once anatomic alignment has been confirmed, the wire is advanced across the fracture, down the medullary canal, and into the proximal cortex. Ideally, proximal fixation is obtained with cortical purchase in the metacarpal base or metaphysis (opposite cortex from initiation point) (Fig. 5-5). Crossing the CMC joint to allow the pin to reside in the distal carpus is typically not problematic.
Maintenance of fracture reduction and pin placement is confirmed with intraoperative imaging. A second pin of the same caliber is placed in the opposite collateral recess using the previously discussed technique. Often, the two pins obtain a crossed configuration proximal to the fracture site. With the pins in place, the stability of the fracture fixation and the rotational alignment are assessed. The pins are bent at 90 degrees and cut (Fig. 5-6). A bulky dressing and protective splint are applied.
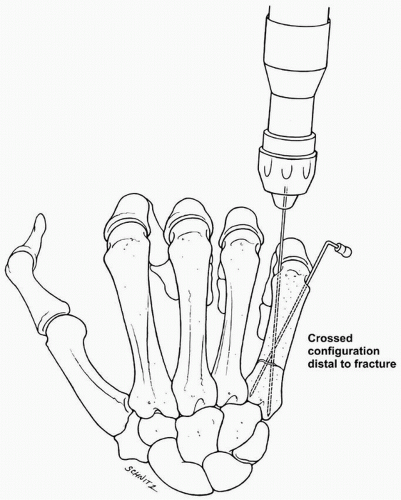 FIGURE 5-5 Ideally, the collateral recess pins occupy a crossed configuration within the medullary canal with purchase in the proximal metacarpal metaphysis. |
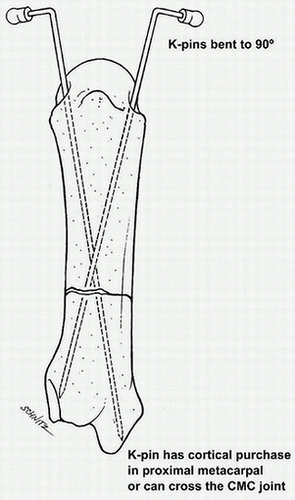 FIGURE 5-6 Kirschner wires are bent and cut after fluoroscopic confirmation of the collateral recess pins. |
Bouquet Pinning
An alternative method of pin fixation may be considered when treating distal third metacarpal fractures involving the border digits. In metacarpal neck fractures that are reducible but unstable, “bouquet pinning” or intramedullary stabilization can be utilized.
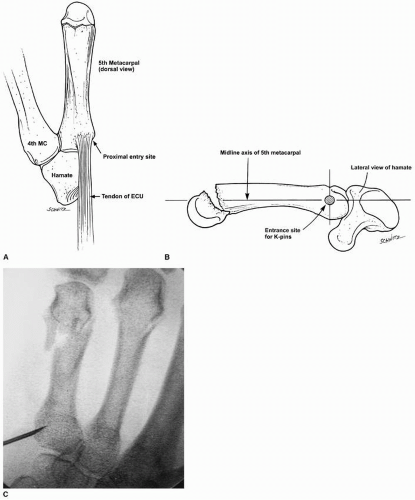
The incision is distant from the distal metacarpal fracture site. It is made at the glabrous border over the tubercle of insertion of the extensor carpi ulnaris (ECU) tendon (Fig. 5-7). The length of the incision may vary with patient size, but 2.0 cm to 3.0 cm is standard. Care must be exercised to avoid damage to smaller arborizations of the dorsal sensory branch of the ulnar nerve. Typically, the main sensory branch crosses the midaxis, an imaginary line drawn between the ulnar styloid and the ECU tubercle, about halfway between these structures. Thus, it is conceivable that handling of the nerve will be necessary, even through such a limited incision (see Fig. 5-2).
Because a relatively volar starting point is desired, the ECU tendon should be reflected dorsally, but splitting the insertion as it fans to a broader area is acceptable. There is a small area of prominence, a “shoulder,” at the ulnar metacarpal base that presents a convexity relative to the juxtaarticular margin at the CMC joint and the remainder of the metaphysis; it is at this area, or just proximal to it, that the intramedullary canal should be entered (Fig. 5-8A, B). Use of fluoroscopy to
locate the entry site is recommended to avoid potential pitfalls (Fig. 5-8C). If the cortical window is made too proximal, intra-articular fracture into the CMC joint could result. More commonly, the entry is too distal, which makes introduction of the pin arduous as it has difficulty by passing the narrow isthmus.
locate the entry site is recommended to avoid potential pitfalls (Fig. 5-8C). If the cortical window is made too proximal, intra-articular fracture into the CMC joint could result. More commonly, the entry is too distal, which makes introduction of the pin arduous as it has difficulty by passing the narrow isthmus.
Cortical perforation can be accomplished with hand tools or power drills. After initial opening of the canal, the entry site is best enlarged with curettes. Because the direction of the tools entering the canal influences the tract taken by the fixation pins, the introitus should be machined with the most acute angle possible (Fig. 5-9). Although the integrity of the metacarpal base must be maintained, the portal of entry must be large enough to accommodate the desired number of pins (usually three). The size of the hole is approximately 4 to 6 mm in diameter. The portal is made ovoid to minimize the chance for fracture propagation due to this stress riser.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree