Operative Treatment of Finger Carpometacarpal Joint Fracture-Dislocations
John J. Walsh IV
DEFINITION
Fractures and dislocations of the carpometacarpal (CMC) joints of the index through small fingers involve intraarticular fractures at the base of the metacarpals or pure dislocations between the metacarpals and carpus. The fracture can involve the base of the metacarpal or the trapezoid, capitate, or hamate articular surface.
These fractures and dislocations can result in instability and articular incongruity (FIG 1).
ANATOMY
The CMC joints connect the metacarpals and the distal carpal row.
The shape and degree of constraint present in the joints differ from finger to finger.
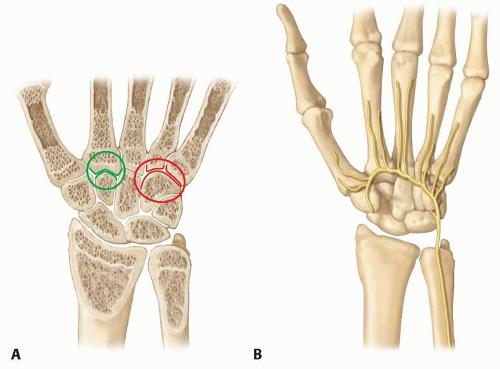
The index and middle fingers have highly constrained articulations due to the shape of the index CMC articulation and supporting soft tissues.4 These include the flexor carpi radialis tendon, extensor carpi radialis longus and brevis tendons, and very strong capsular insertions. This provides for a strong radial column for the hand and efficient force transfer to the radius (FIG 2A).
The ring and small fingers have a gliding articulation on the hamate, which allows for the closure of the hand around objects and is very important in power grip. This mobility makes them more susceptible to injury. The extensor carpi ulnaris tendon attaches to the dorsal base of the small finger metacarpal.4
The deep motor branch of the ulnar nerve crosses around the base of the hamate hook from ulnar to radial and runs along the volar surface of the CMC joints (FIG 2B). It is vulnerable at the time of injury or during fixation.
PATHOGENESIS
Injuries of the CMC joints may be divided into two broad categories.
The first, involving a load applied to a flexed metacarpal, is by far the most common mechanism. This injury usually involves the ring and small fingers displacing dorsally as a unit relative to the hamate. This may occur as a dislocation only or include a marginal fracture of the hamate.8
NATURAL HISTORY
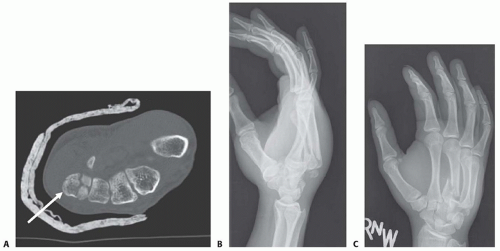
The natural result of an untreated fracture-dislocation is progressive arthritis of the involved joints. This occurs due to progressive subluxation of the joint(s) and articular incongruity (FIG 4A-D).
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient’s history is important to assess the mechanism of injury, which provides further clues regarding concomitant injuries in the extremity.
Examine the hand for tenderness and local swelling.
Assess neurovascular integrity, especially function of the deep motor branch of the ulnar nerve (first dorsal interosseous contraction).
Examine the limb for other injuries.
Associated injuries should be detected by examination and verified by radiographs.
Preoperative notation of nerve function is important when comparing function following reduction and fixation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs of the CMC joints require careful positioning to assess each joint.
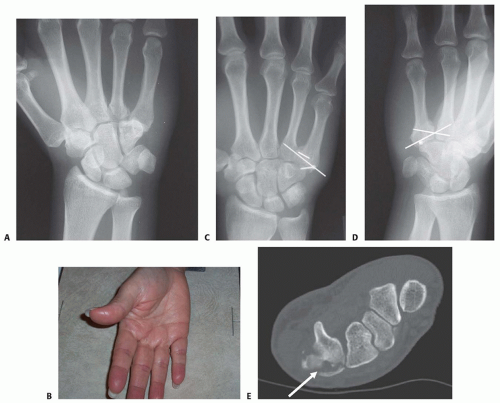
The transverse metacarpal arch causes the CMC joints of the index and middle fingers to appear in an oblique projection when a standard posteroanterior (PA) radiograph is obtained of the ring and small finger CMC joints and vice versa (FIG 5A).
A true frontal radiograph is most easily obtained by positioning the hand in an anteroposterior (AP) projection with the dorsum of the hand placed flat on the cassette (or image intensifier, if using fluoroscopy). The base of the affected metacarpal should lie on the cassette (FIG 5B). This will result in a far more accurate portrayal of the joint, essential for assessing the fracture as well as checking hardware position after fixation.
Visualization of the joint surfaces at the base of the ring and small fingers differs in a typical PA projection (FIG 5C) and a properly positioned film of the same patient (FIG 5D).
A computed tomography (CT) scan should be obtained in most cases to assess for articular injury. CT also is especially helpful for visualizing impacted articular surface fragments. The best visualization and determination of fracture patterns will be possible if the scan is obtained after preliminary reduction of any displaced fractures or dislocations associated with a fracture (FIG 5E).10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree