Operative Treatment of Distal Interphalangeal Joint Fracture-Dislocations
Leo T. Kroonen
Eric P. Hofmeister
The views expressed in this chapter are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
DEFINITION
Injuries about the distal interphalangeal joint (DIP) consist of avulsion injuries of the terminal extensor tendon or the flexor digitorum profundus (FDP) tendon, isolated dislocations of the DIP joint, and complex tuft fractures.
A “bony” mallet finger (ie, mallet fracture) is an intraarticular bony avulsion at the insertion site of the terminal extensor tendon on the dorsal base of the distal phalanx that results in inability to actively extend the DIP joint.
A “non-bony” mallet finger is an injury to the extensor mechanism at or near the insertion onto the distal phalanx that typically results in inability to actively extend the DIP joint.
“Jersey finger” is an avulsion of the FDP tendon, with or without its bony attachment, from the volar base of the distal phalanx. It typically results in inability to actively flex the DIP joint.
Isolated dislocations of the DIP joint are rare injuries in which the distal phalanx is dislocated either dorsal or volar relative to the middle phalanx.
An intra-articular or tuft fracture can have a component of a mallet or FDP avulsion, and should be treated accordingly, while also taking into consideration the additional instability associated with the fracture.
ANATOMY
The DIP joint is stabilized by the radial and ulnar collateral ligaments, the volar plate, and the firm insertions of the FDP and terminal tendons of the extensor mechanism.
The extensor mechanism terminates with the confluence of the lateral bands into a single terminal tendon, which inserts on the dorsal base of the distal phalanx. The terminal tendon is a strong, flat, thin segment that averages 10.1 mm in length and 5.6 mm in width.15
The terminal tendon insertion, on average, is 1.4 mm proximal to the germinal matrix of the fingernail.15
The volar surface of the terminal tendon usually is adherent to the dorsal capsule of the DIP joint.15
The FDP tendon inserts on the volar surface of the base of the distal phalanx. It is surrounded by the flexor tendon sheath. The A4, A5, and C3 pulleys secure the FDP tendon around the level of the DIP joint.
The vinculum longus profundus and vinculum brevis profundus are thin mesenteries providing vascular supply to the distal portion of the FDP tendon. They also provide a weak attachment of the FDP tendon to the flexor tendon sheath.8
PATHOGENESIS
Mallet finger injuries are the result of a disruption to the extensor mechanism at or near the insertion to the base of the distal phalanx. Such disruptions can occur as a result of a laceration or a sudden flexion force to an extended DIP joint. The disruption of the extensor mechanism allows unopposed pull of the FDP tendon, leaving the DIP joint in a flexed posture and sometimes volar subluxation of the joint.
Jersey finger injuries occur as a result of disruption to the FDP, from either a laceration or a sudden extension force applied to a flexed DIP joint during an eccentric contraction. The disruption of the FDP tendon leaves the pull of the extensor mechanism unopposed, resulting in a flaccid and often extended posture of the DIP joint.
Dislocations of the DIP joint are rare due to the inherent stability provided by the collateral ligaments, the volar plate, and the flexor and extensor tendon insertions. However, when a dislocation does occur, the distal end of the middle phalanx usually “buttonholes” through these structures, making reduction more difficult.
Complex intra-articular distal phalanx fractures and tuft fractures can occur as a result of crushing injuries or axial loading injuries. Careful attention should be given to these injuries to determine whether or not they demonstrate accompanying characteristics of a mallet injury or FDP avulsion. Characteristics such as a transverse shaft fracture impart further instability to the injury pattern and should be treated with stabilization first in order to have a firm foundation on which to base further fixation.
NATURAL HISTORY
Mallet finger injuries can occur in any digit but most commonly are seen in the three most ulnar digits.
Left untreated, a mallet finger injury can progress to a secondary “swan neck” deformity.
With the disruption of the extensor mechanism at the DIP joint, the pull of the lateral bands adds to the extension force of the central slip at the PIP joint, thereby creating an imbalance in forces at the PIP joint and a hyperextension deformity at that joint.17
Despite treatment, residual deformity, usually in the form of a dorsal prominence, can be seen in up to 80% of cases.17 Additionally, lack of terminal extension or a mild flexion contraction may persist.
Approximately, 75% of cases of FDP avulsions involve the ring finger. Some authors theorize that this is because the ring finger protrudes the farthest distally when the hand is held in a flexed position; however, no literature has proven this theory.
Leddy6 proposed the classification system that is still widely used today for FDP avulsion injuries, based on the level of retraction of the tendon. Other authors since have made additions to this injury.
Type I FDP avulsions retract into the palm, thereby disrupting the vincular system and leading to poor blood supply. Surgery should be performed within 7 to 10 days.
Type II injuries retract to the level of the PIP joint or distal A2 pulley. An associated small bony fleck often is seen on the lateral radiograph. Because the proximal blood supply is preserved through the long vincula, these injuries can be successfully treated as late as 6 weeks from the time of injury.
Type III injuries usually are associated with a bony avulsion and as a result do not retract proximal to the A4 pulley. These injuries are treated as bony injuries with open reduction and internal fixation and can be treated late if required.
Type IV injuries are bony avulsion injuries in which the tendon also has separated from the avulsed bony fragment. Time to treatment depends on the level of tendon retraction.16
Type V injuries are bony FDP avulsion injuries coupled with a distal phalanx fracture.
Type Va subtype is with an associated extra-articular fracture.
PATIENT HISTORY AND PHYSICAL FINDINGS
As with all hand injuries, patients should be questioned about their hand dominance and occupational requirements to aid the surgeon in better understanding individual needs and goals.
The following examinations should be performed to determine possible injuries:
FDP function
Inability to flex at the DIP joint implies disruption of the FDP tendon.
Limited, weak, or painful flexion may indicate a partial injury or a complete disruption with intact vinculae or pseudotendon.
DIP joint extensor mechanism function
Inability to extend at the DIP joint implies disruption of the terminal extensor tendon. Weak extension implies a partial or less severe injury. Loss of passive extension indicates a possible fracture or dislocation.
Axial injuries to an extended DIP joint often are the culprit in mallet finger injuries.
The history often reveals an axial blow to the fingertip, such as when an incoming ball strikes an extended fingertip.
The patient will be unable to actively extend at the DIP joint.
Jersey finger injuries often are the result of a sudden extension force on a flexed DIP joint, such as when grabbing for another player’s shirt while playing football.
Patients will be unable to actively flex through the DIP joint.
Active PIP flexion will be present but may be moderately diminished due to pain or stiffness.
Most dislocations of the DIP joint are the result of sporting injuries.12,13 In addition to a deformity, there will be lack of active and passive motion of the joint.
The tenodesis effect can also be used to test the continuity of the terminal flexor or extensor tendons.
Passively flexing the wrist should result in extension of the DIP joint by tensioning the extensor tendons at the level of the wrist. If a flexed position is maintained at the DIP joint despite full wrist extension, then an extensor tendon injury should be suspected.
Passively extending the wrist should cause flexion of the DIP joint. If the injured finger does not flex with the neighboring digits, FDP injury should be suspected.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs of the affected hand (posteroanterior [PA], lateral, and oblique) and dedicated views of the affected finger (PA, lateral, and oblique) should be obtained and usually are sufficient for making the diagnosis in association with a thorough clinical examination.
Mallet finger injuries can be associated with a bony avulsion. Any joint subluxation should be noted, and the size of the avulsed fragment should be estimated (FIG 1).
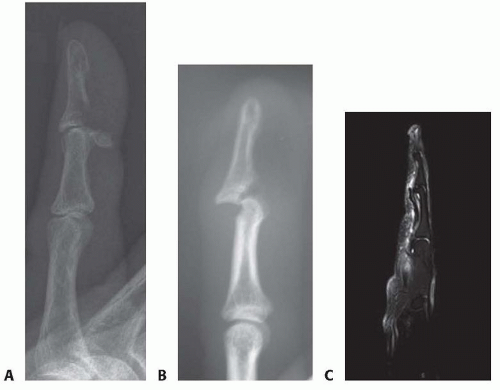
In FDP avulsion injuries, the location of the retracted flexor tendon often can be appreciated by finding a bony fragment on the lateral radiograph of the affected digit (FIG 2A,B).
Ultrasound sometimes can be helpful in determining continuity of the flexor tendon or identifying the location of the retracted proximal flexor tendon stump.3,7,14
Magnetic resonance imaging (MRI) can be useful in determining flexor tendon continuity and level of tendon retraction (FIG 2C).
DIFFERENTIAL DIAGNOSIS
Osteoarthritis
Inflammatory arthropathy (such as gout, rheumatoid arthritis [RA], etc.)
FDP rupture
FDP laceration
Terminal extensor tendon rupture (mallet finger)
Mallet fracture
NONOPERATIVE MANAGEMENT
For tendinous mallet fingers and mallet fractures involving less than one-third of the articular surface and without joint subluxation, a variety of splints are available.
We prefer immobilizing the DIP joint with a prefabricated polyethylene extension splint.
For hygiene assistance, the patient is given two splints that can be alternated to assist in keeping the skin dry. They should be carefully instructed to always keep the digit in full extension when changing splints. This can be accomplished by keeping the entire digit flat against a countertop while sliding the splints on and off.
Casting of the DIP joint also has been described.
Full-time splinting in extension is recommended for 6 weeks, followed by 6 weeks of part-time splinting. During this second 6 weeks, patients are advised to wear the splint for any heavy activity and at night.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree