Operative Strategies for Basilar Thumb Fractures: Rolando’s and Bennett’s Fractures
Michael D. Wigton
Joelle Tighe
Mark E. Baratz
INDICATIONS/CONTRAINDICATIONS
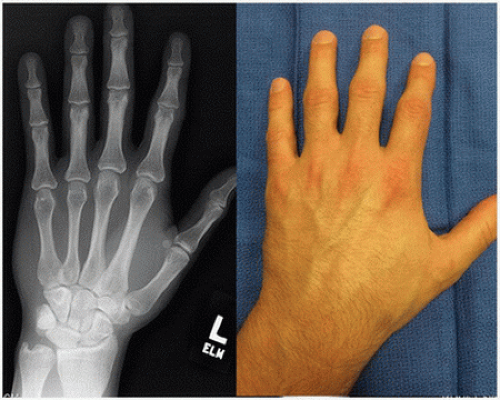
Injuries to the base of the thumb metacarpal typically present with two patterns: Bennett’s fracture or Rolando’s fracture. Both fractures are characterized by inherent instability due to the ligamentous and tendinous insertions crossing the thumb carpometacarpal (CMC) joint. Additionally, these fractures involve the surface of the base of the thumb metacarpal (Fig. 7-1). Bennett’s fracture was first described in 1885 by Dr. E.H.
Bennett, in an address to the British Medical Association (1). This pattern involves a volar (palmar)-ulnar fracture fragment that remains attached to the tubercle of the trapezium by virtue of the anterior oblique ligament (AOL) (Fig. 7-2). The base of the metacarpal is subluxated in a proximal, radial, and supinated position due to the pull of the abductor pollicis longus. The radial subluxation of the metacarpal base leads to an adducted posture of the thumb metacarpal. Rolando’s fracture involves an additional radial fragment with or without comminution of the base of the first metacarpal (2).
Historically, nonoperative management was the treatment of choice in fractures of the base of the thumb metacarpal. In 1990, Livesley published a 26-year follow-up of nonoperatively treated Bennett’s fractures in which 100% had decreased range of motion and grip strength (3). Since then, operative treatment has been favored.
Surgical indications include displaced and/or unstable fractures or articular displacement greater than 2 mm. (Articular displacement alone is a debatable topic in the literature as there are conflicting reports of the long-term functional significance of joint degeneration.) The current standard of care in most cases is operative as few fractures of the base of the first metacarpal are neither stable nor nondisplaced. The CMC joint is a saddle articulation with concavity in the volar-dorsal plane and convexity in the radial-ulnar plane. This joint has an inherently wide range of motion in all planes allowing opposition, pinch, and grip functions of the thumb; this results in fracture instability. The AOL or beak ligament (Fig. 7-2) prevents volar subluxation of the metacarpal and accounts for the relative stability of the constant fragment in a Bennett’s fracture. The abductor pollicis longus (APL) (Fig. 7-1) crosses the CMC joint and inserts on the proximal and radial aspect of the first metacarpal creating a deforming force in both a Bennett’s and Rolando’s fracture pattern. The APL accounts for the radial and dorsal translation of the metacarpal in Bennett’s fracture and the displacement of the radial fracture fragment(s) in Rolando’s fracture. The extensor pollicis
longus (EPL) contributes to the dorsal and proximal migration of the metacarpal. Adduction of the metacarpal is seen most significantly with Bennett’s fracture and is caused by the adductor pollicis (AdP) insertion at the proximal, ulnar base of the proximal phalanx. Together, these forces create the classic deformities seen.
longus (EPL) contributes to the dorsal and proximal migration of the metacarpal. Adduction of the metacarpal is seen most significantly with Bennett’s fracture and is caused by the adductor pollicis (AdP) insertion at the proximal, ulnar base of the proximal phalanx. Together, these forces create the classic deformities seen.
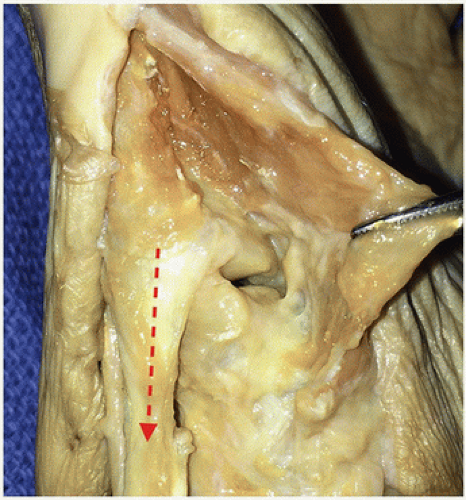 FIGURE 7-1 Anatomical dissection of left thumb showing the first CMC joint with the APL insertion with the direction of pull indicated. |
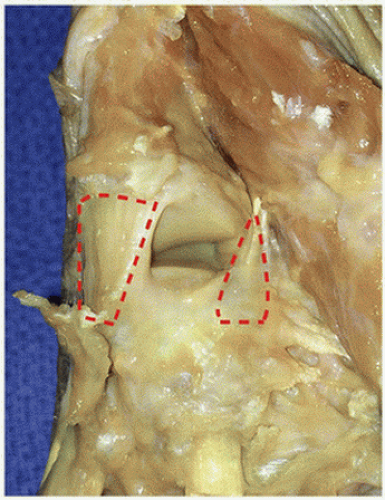 FIGURE 7-2 The left CMC joint is demonstrated with the palmar/volar (right) and dorsal (left) ligaments outlined. |
Nonoperative treatment is an option for stable, nondisplaced fractures. Cast immobilization with weekly close radiographic follow-up over the first 4 weeks postinjury is recommended as these fractures may have tendency for displacement even if initially nondisplaced.
PREOPERATIVE PLANNING
The mechanism of injury typically involves an axial load to the thumb, often occurring during a sporting event, fall, or higher-energy trauma such as a motor vehicle collision. Physical examination will reveal pain, swelling, and ecchymosis about the base of the thumb metacarpal. Swelling can be significant, resulting in distortion of usually palpable landmarks.
Radiographic evaluation includes posteroanterior and lateral views of the thumb (Figs. 7-3 and 7-4). Views specific for the thumb CMC joint may also be useful such as Robert’s view (4) and Bett’s or Gedda’s view (5,6). These views may be difficult to obtain in the acutely traumatized hand. Preoperative computed tomography scan is reserved for chronic injuries to assess deformity, union, and the presence of arthritic changes.
If closed reduction and pinning is contemplated, we prefer to attempt this in the first week following the injury to facilitate exposure and reduction. Initially, the fracture is immobilized in a thumb spica splint and the limb is elevated.
The primary operative goal is a stable CMC joint with the articular surface of the metacarpal that is aligned with the trapezium. The base of the radial cortex of the metacarpal typically forms a “V” with the radial cortex of the trapezium. A “broken V” is seen with fracture-subluxation of the metacarpal. Restoration of the “V” indicates correction of the subluxation (Figs. 7-5 and 7-6). A perfect articular surface is not always possible, nor does it seem to alter the short- or long-term outcome. A number of techniques have been described for both Rolando’s and Bennett’s fractures.
Closed reduction and percutaneous pinning, open reduction and internal fixation, traction pinning, and external fixation may be viable options in either fracture pattern.
Closed reduction and percutaneous pinning, open reduction and internal fixation, traction pinning, and external fixation may be viable options in either fracture pattern.
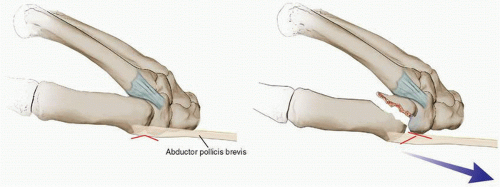 FIGURE 7-5 Line drawing representing the radial “v” as seen in the anatomically normal CMC articulation (left). In Bennett’s fracture, the “v” is broken with CMC subluxation (right). |
We prefer closed reduction and pinning for both injury patterns. Open reduction and internal fixation is reserved for fracture-dislocations where we cannot get reasonable alignment of the metacarpal base with respect to the trapezium or in Bennett’s fractures or where there are two large fracture fragments.
SURGICAL TECHNIQUE
The patient is placed in a supine position. We prefer regional anesthesia with a proximal block (axillary). The arm is positioned at 90 degrees from the body on an operating hand table. Intraoperative fluoroscopy is used for assessment of fracture reduction and fixation.
Closed Reduction With Percutaneous Pinning
Bennett’s Fracture Closed reduction and percutaneous pinning are preferred in the majority of the Bennett’s fracture during the acute phase provided the articular reduction is less than 1 to 2 mm of articular step-off (7,8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree