Operative Reconstruction of Digital Polydactyly, Including the Duplicated Thumb
Heather R. Harrison
Kevin J. Little
PREAXIAL POLYDACTYLY
Indications/Contraindications
The duplicate thumb was first described in 1645 by Digby, and its treatment has continued to evolve and be improved since. The presence of a duplicate thumb usually represents an indication for surgical reconstruction due to psychosocial, cosmetic, cultural, and functional concerns. The reported incidence varies greatly but is most commonly reported as 1 per 3,000 live births (1). It is found equally in blacks and whites but is slightly more common in Native Americans and Asians. It is categorized as a type of duplication as recommended by the International Federation of Societies for Surgery of the Hand (IFSSH) and the American Society for Surgery of the Hand (2,3,4).
The most commonly used classification for preaxial polydactyly was described by Wassel and has been used to accurately describe the presentation of the duplicate thumb. This system defines the anatomic location of duplication and is broken into seven categories, beginning distally with a bifid distal phalanx as type I. The odd numbers represent incomplete duplications and the even represent complete duplications of bones. The Wassel IV classification involves a single but widened metacarpal with duplication of the proximal and distal phalanges and represents 43% of all cases. Wassel II involves a duplicated distal phalanx only and is the second most common representing 15% of cases. Any triphalangeal thumb is classified as type VII (5) (Fig. 37-1).
A newer classification modification has been proposed by Zuidem and colleagues to better classify triphalangeal thumbs as well as triplications and deviation. They also further described the position of the duplications using m, u, and r to describe middle, ulnar, and radial locations, respectively (Fig. 37-2). None of the previously described classification systems addresses the fact that neither of the thumbs in preaxial polydactyly is normal; therefore, referring to it as a split thumb may be more accurate and better explain the treatment goals (6).
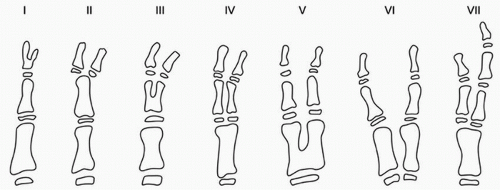 FIGURE 37-1 Wassel classification of preaxial polydactyly. (Reproduced with permission from Wassel HD: The results of surgery for polydactyly of the thumb. Clin Orthop 64: 179, 1969.) |
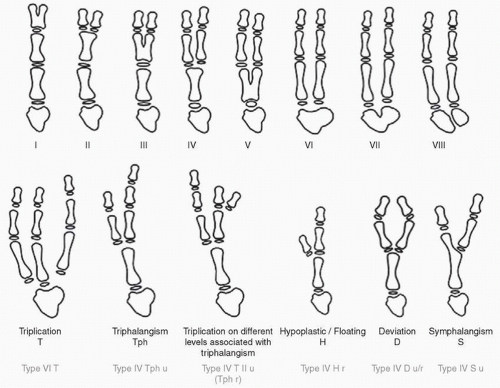 FIGURE 37-2 Zuidem classification of preaxial polydactyly. (Reproduced with permission from Zuidem JM, et al.: A classification system of radial polydactyly: inclusion of triphalangeal thumb and triplication. J Hand Surg Am 33(3): 374, 2008.) |
The overall surgical goals regardless of type are to ablate the hypoplastic component, combine structures from both thumbs to create a stable metacarpophalangeal (MP) joint, align bony units, and centralize tendinous structures to optimize motion while maintaining a healthy sensate pulp for pinch and prehensile activity (7,8,9).
The timing of surgical reconstruction is dictated by the progression of prehensile activity as well as safety. At 6 months of age, gross grasp and grip develop, while thumb and index finger pinch does not develop until 12 to 15 months of age. Established fine motor patterns develop between 2 and 3 years of age. Performing reconstruction when the patient is 9 to 12 months of age decreases the risks associated with anesthesia while preceding development of pinch, allowing this function to develop normally after the reconstruction. Allowing the hand to grow during the first 9 to 12 months also allows for easier dissection of neurovascular and tendinous structures.
Contraindications to surgery are typically related to other underlying conditions. Conditions such as Holt-Oram, Diamond-Blackfan, and Fanconi’s anemia are more commonly seen with hypoplastic thumbs; however, they may also be present with thumb duplication, especially if the duplicate thumb involves a triphalangeal component. Hematologic indices as well as pediatric genetic consultation should be sought prior to proceeding with any surgical intervention (3,7).
Preoperative Planning
Duplication of the thumb usually occurs as a sporadic mutation; however, rarely, an autosomal dominant inheritance pattern can be seen especially with type VII duplications, and genetic counseling should be offered to these patients’ parents. A complete blood count (CBC) and platelet count along with prothrombin time (PT) should be assessed to rule out thrombocytopenia and coagulopathies (3,7).
It is important to explain early on to the parents that the child with a duplicate thumb will never have a completely normal thumb after surgical reconstruction. This will help to avoid any misconceptions that may arise later. Removal of the hypoplastic component and reconstruction of the dominant thumb will still leave the child with a smaller and stiffer thumb. Long-term studies have shown that even after surgical reconstruction, interphalangeal motion will be limited, averaging 0 to 30 degrees. The possibility of postoperative sequelae, such as joint laxity, thumb size and appearance mismatch, and the zigzag deformity, should be discussed with the parents as well as the 25% need for revision later as the child grows. These risks increase when the thumbs are crooked or angulated preoperatively (10,11,12).
Preoperative physical and radiographic examinations both at presentation as a newborn and shortly prior to planned intervention allow for refinement of the surgical plan, as well as developing a relationship with the family and realistic expectations of outcomes. Examination of the digits will usually demonstrate that the more radial component is hypoplastic and better suited for ablation; however, occasionally, the radial component is more functional and will need to be salvaged (Fig. 37-3A,B). The flexor and extensor tendons are frequently displaced radially and will need centralization. This should be examined and identified during preoperative examination. Additionally, there are occasional connections between the extensor pollicis longus (EPL) and flexor pollicis longus (FPL) tendons, known as pollex abductus, which will need to be identified and released to prevent recurrent deformity (Fig. 37-4). The abductor pollicis brevis (APB) tendon often inserts on the radial thumb in type IV duplications, which potentiates the angular deformity if not addressed at the time of surgery. Radiographs most commonly in the Wassel IV presentation demonstrate a widened metacarpal head that requires intraoperative reduction. Bony angulation of the metacarpals and phalanges should be evaluated to determine the need for osteotomies. Collateral ligament stability should be assessed, as most commonly the radial collateral ligament of the MP joint is unstable and will require reconstruction. Simple ablation of one of the duplicate thumbs was previously attempted; however, this does not address the APB insertion, radial collateral ligament reconstruction, or appropriate skeletal alignment of the remaining thumb and thus has not provided satisfactory results (10,13,14).
Arteriography is not usually necessary for preoperative planning. The arterial pattern has been studied by Kitayama, who found that more than 75% of the time there is a digital vessel to each component and 5% of the time, there is only one single digital vessel to the ulnar component and none to the radial. In the rare case that the radial component is determined to be more appropriate for reconstruction, this should be taken into consideration (15).
In the patient with near-symmetrical type II or III duplication, we have a discussion with the family regarding the outcomes of ablation and reconstruction versus modified Bilhaut-Cloquet as proposed by Baek et al. The modified Bilhaut-Cloquet procedure has a higher rate of stiffness and decreased motion and frequently results in nail deformities; however, it provides a more cosmetic result with a thumb more similar in width and appearance to the contralateral side. Ablation and reconstruction should be selected if increased thumb motion and function is preferred to a better cosmetic result (16,17,18).
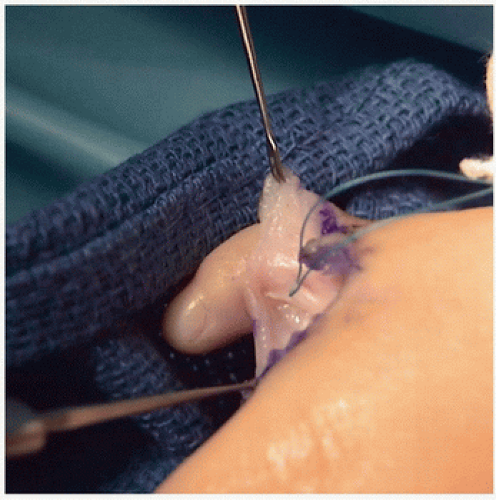 FIGURE 37-4 Clinical photograph of the tagged pollex abductus connection between the EPL and FPL tendons. (Photograph courtesy of Kevin J. Little, MD.) |
The Bilhaut-Cloquet procedure described as a longitudinal osteotomy taking a central wedge resection of bone and soft tissue and approximating the remaining components of the radial and ulnar digits is complicated by joint stiffness, growth arrest, asymmetric growth, and nail bed deformities
due to its intra-articular nature and physeal involvement (5,16,19) (Fig. 37-5). Naasan and Page (20) have reported secondary deformities in 71% of thumbs reconstructed utilizing this technique. Remaining extra-articular allowed Baek and colleagues to avoid growth arrest and nail bed deformities. The modified Bilhaut-Cloquet is advocated in Wassel type II and III thumbs. In a small sample size of 7 patients, Baek and colleagues demonstrated satisfactory functional and cosmetic results with preserved preoperative range of motion in type III, improved range of motion in type II thumbs, and no cases of nail deformities or growth arrest (17,18).
due to its intra-articular nature and physeal involvement (5,16,19) (Fig. 37-5). Naasan and Page (20) have reported secondary deformities in 71% of thumbs reconstructed utilizing this technique. Remaining extra-articular allowed Baek and colleagues to avoid growth arrest and nail bed deformities. The modified Bilhaut-Cloquet is advocated in Wassel type II and III thumbs. In a small sample size of 7 patients, Baek and colleagues demonstrated satisfactory functional and cosmetic results with preserved preoperative range of motion in type III, improved range of motion in type II thumbs, and no cases of nail deformities or growth arrest (17,18).
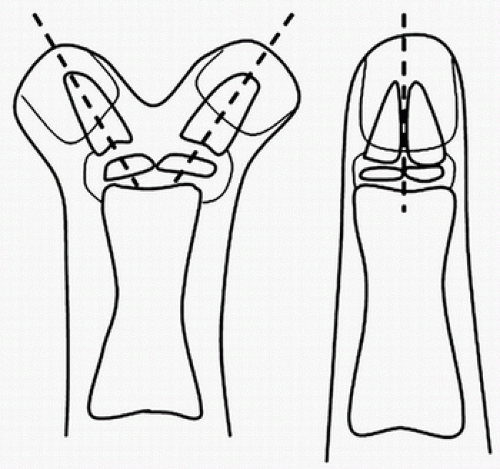 FIGURE 37-5 The Bilhaut-Cloquet sharing procedure. (Reproduced with permission from Malliet M, et al.: Results after surgical treatment of thumb duplication: a retrospective review of 33 thumbs. J Child Orthop 1(2): 136, 2007.) |
Surgical Technique
Wassel Type IV Reconstruction with Excision of Hypoplastic Digit The surgery is performed under general anesthesia in the supine position, with the upper extremity on a hand table. A tourniquet is placed high on the arm and, after exsanguination, inflated to approximately 100 mm Hg above systolic pressure.
A zigzag incision is made beginning just distal to the carpometacarpal joint and continued to the base of the radial hypoplastic thumb, around this in a racquet fashion and continued in a zigzag fashion along the radial border to the level of the IP joint of the ulnar thumb. This incision should be constructed in a zigzag fashion as a longitudinal scar will contract and can contribute to a postoperative angular deformity and thus should be avoided (Fig. 37-6). The flaps are developed and can be
tagged with suture to help in exposure. The initial dissection should identify and retain all structures to both thumbs. Aberrant tendons along with neurovascular structures should be identified prior to any vascular structures being ligated. EPL and FPL tendons are dissected proximal and commonly bifid at the level of the bony duplication, ensuring that the pollex abductus is released. These are released at their insertions on the radial thumb and tagged for later use.
tagged with suture to help in exposure. The initial dissection should identify and retain all structures to both thumbs. Aberrant tendons along with neurovascular structures should be identified prior to any vascular structures being ligated. EPL and FPL tendons are dissected proximal and commonly bifid at the level of the bony duplication, ensuring that the pollex abductus is released. These are released at their insertions on the radial thumb and tagged for later use.
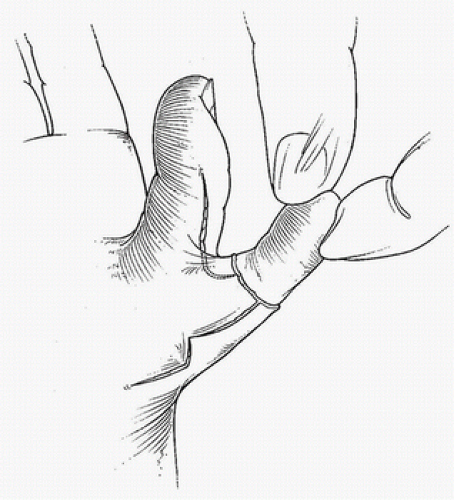
Next, the APB muscle and tendon are identified from the thenar aspect to its insertion on the proximal phalanx of the radial thumb taking care to not violate the underlying radial collateral ligament. The insertion is released and tagged for later transfer to the ulnar thumb. The proximal phalanges may be completely duplicated and separate, or there may be a cartilaginous connection, which should be transected longitudinally to the level of the MCP joint (Fig. 37-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree