Operative Fixation of Juxta-Articular, Intracapsular, and Diaphyseal Fractures of the Phalanges and Interphalangeal Joints
David E. Ruchelsman
Matthew I. Leibman
Mark R. Belsky
Thomas J. Graham
The phalanges are short tubular bones, but tend to exhibit similar fracture patterns to the long tubular bones of the skeleton. Phalangeal fractures are subject to displacement, angulation, and malrotation due to forces exhibited by the traversing flexor and extensor tendons and collateral ligaments at juxta-articular locations. The metaphyseal and articular fractures are subject to compressive forces and joint impaction, and diastasis can be challenging to reconstruct. The etiology of digital stiffness following operative fixation of unstable phalangeal diaphyseal, juxta-articular, and intra-articular fractures may be multifactorial. Malreduction with resultant soft-tissue imbalances, extensor/flexor tendon adhesions, and capsular contractures may be minimized with meticulous operative technique and initiation of early functional rehabilitation.
Conceptually, we divide phalangeal fractures into articular and nonarticular injuries involving the proximal, middle, and distal phalanges. Extra-articular fractures include fractures of the neck, shaft, or base. Articular fractures include unicondylar fractures; comminuted intra-articular fractures (i.e., bicondylar fractures); dorsal, volar, or lateral base fractures; pilon fractures and fracture-dislocations; and diaphyseal fractures with articular extension.
EXTRA-ARTICULAR PHALANGEAL FRACTURES
Diaphyseal Phalangeal Fractures
Phalangeal fractures may be transverse, oblique, spiral, or comminuted/multifragmentary. The latter are usually associated with significant soft-tissue injury even if the overlying skin envelope is intact. Spiral and oblique fractures are more common in the proximal phalanx diaphysis, and transverse fractures tend to be more common in the middle phalanx and proximal third of the proximal phalanx.
Transverse proximal phalangeal fractures tend to collapse into an apex volar angulation, with the proximal metaphysis flexed by the interosseous insertion. The remainder of the phalanx then collapses into extension due to the longitudinal pull of the extrinsic extensor. Angulation of middle phalangeal fractures is generally apex dorsal as the sublimis insertion along the distal fragment draws the distal fragment into flexion.
Transverse proximal phalangeal fractures tend to collapse into an apex volar angulation, with the proximal metaphysis flexed by the interosseous insertion. The remainder of the phalanx then collapses into extension due to the longitudinal pull of the extrinsic extensor. Angulation of middle phalangeal fractures is generally apex dorsal as the sublimis insertion along the distal fragment draws the distal fragment into flexion.
Management of phalangeal fractures depends on the following factors: displacement, fracture geometry, soft-tissue injury, and patient characteristics and requirements. Treatment should be tailored to the individual taking into consideration fracture characteristics.
Oblique and spiral fractures are prone to shortening and malrotation when treated nonoperatively. Periarticular oblique fractures may involve the collateral recess or subcondylar fossa and effect function. Comminuted fractures are prone to shortening, soft-tissue adhesions, delayed healing, and stiffness.
Indications/Contraindications
Greater than 10 degrees of malangulation in the coronal or sagittal plane
Malrotation
Shortening
Open fractures
Combined injuries
Preoperative Preparation
Regional versus local anesthesia
Mini-C arm
Kirschner wires (0.045 inch, 0.035 inch)
Modular plate/screws (1.5 mm, 1.3 mm, 1.1 mm)
Techniques
Closed Reduction and Percutaneous Pinning Percutaneous K-wire fixation is the most common method of operative stabilization of unstable proximal and middle phalangeal shaft fractures once satisfactory reduction has been achieved. Care is taken to try and avoid violation of the extensor hood, central extensor tendon, and neurovascular bundles. Early range of motion following percutaneous K-wire fixation is often limited as skin motion at the pin sites may lead to superficial and/or deep pin site infections.
K-wire placement depends on the fracture pattern, configuration, and bone quality. Proximal metaphyseal fractures at the base of the proximal phalanx usually demonstrate dorsal cortical comminution with apex volar angulation. Multiple adjacent fingers can fracture in this fashion in the elderly osteoporotic individual after a fall. Imaging of the phalangeal base is difficult especially after an acute injury. While these fractures are reducible with digital flexion, they are inherently unstable. These fractures may also extend proximally and involve the articular surface.
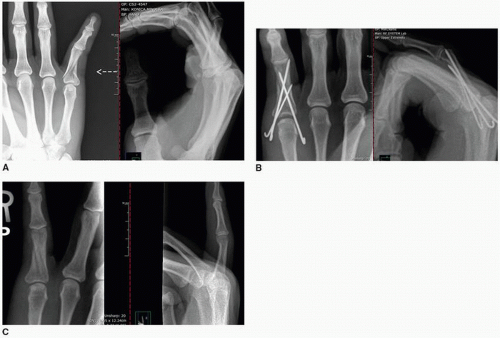
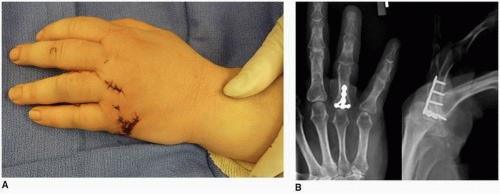
Antegrade crossed K-wires beginning at the periphery of the articular margin are often used to stabilize these fractures (Figs. 6-1 and 6-2). The metacarpophalangeal (MCP) joint is flexed maximally and the distal fracture fragment of the proximal phalanx reduced to the metaphyseal segment.
Alternatively, these fractures can be stabilized with a longitudinal wire passed antegrade through the metacarpal head into the medullary canal of the proximal phalanx (1). Additional pins may be inserted to provide rotational stability especially in more distal fractures. Each technique has inherent advantages and disadvantages. Patients are counseled regarding the potential for extensor and/or flexor tendon adhesions at the level of the metaphyseal fracture corresponding to the A2 pulley. At times, tenolysis of the flexor system and/or MCP/proximal interphalangeal joint (PIP) contracture releases are needed following osseous union.
Oblique and spiral fractures may be stabilized with two or more K-wires passed percutaneously perpendicular to the fracture plane. If one elects percutaneous fixation of these rotationally unstable fractures, it is imperative to use fluoroscopy to ensure that the wires truly engage in a bicortical fashion and in the plane perpendicular to the plane of the fracture (Fig. 6-3). Transverse or short oblique wires can be fixed with crossed K-wires. As crossing K-wires tend to distract the fracture, manual compression must be applied to the digit at the time of insertion of the second wire. The fracture is usually immobilized for approximately 3 weeks, and the wires are then removed followed by protected motion with buddy taping.
Pearls and Pitfalls
Avoidance of an intra-articular starting point with antegrade crossed K-wire fixation of proximal phalangeal metaphyseal/diaphyseal fractures.
Use of intrinsic plus casts/splints to minimize MCP joint stiffness and contracture.
Avoidance of K-wires placed through the collateral recess of the interphalangeal joints to minimize collateral ligament contracture.
Newer fixation systems with self-tapping mini-screws allow for percutaneous screw fixation through small incisions after reduction. Percutaneous screw fixation achieves interfragmentary compression and may allow for earlier motion.
Use of local anesthetic and active motion in the early postoperative period (i.e., 4 to 6 weeks) may facilitate “closed tenolysis” and yield increases active composite flexion.
Postoperative Management Initiation of mobilization is based on clinical tenderness as early clinical union precedes radiographic union. Following clinical union (typically 4 to 6 weeks postoperatively), a digital block may be performed in the office if there is early postoperative digital stiffness followed by active digital motion to attempt “closed tenolysis” of early adhesions and facilitate recovery of digital motion. Sagittal plane malunion may result in clinical pseudo-claw deformity and extensor imbalance with resultant extensor lag.
Open Reduction and Internal Fixation Open reduction is indicated for irreducible phalangeal fractures, open fractures, and combined injuries. Stable internal fixation facilitates early postoperative functional rehabilitation.
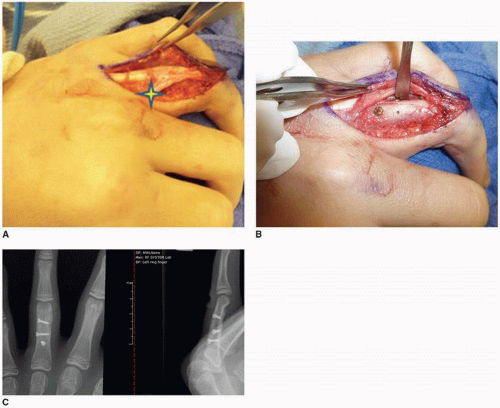
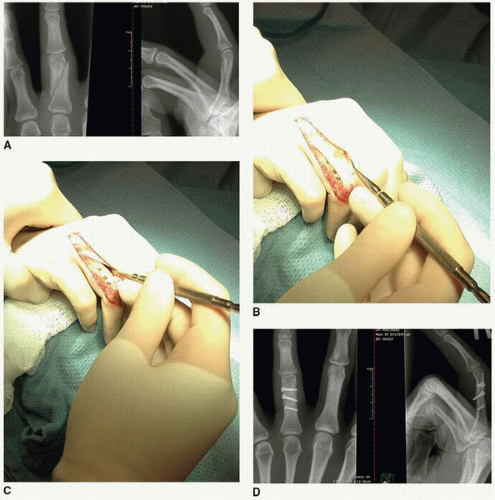
A dorsal curvilinear or lateral/midaxial incision is most frequently utilized for proximal phalangeal exposure. Several deep surgical intervals exist. For diaphyseal fractures of the proximal phalanx, the interval between the central extensor tendon and lateral band may be incised, or the extensor may be mobilized together with the ipsilateral conjoined lateral band (Fig. 6-4). For metadiaphyseal fractures, a unilateral intrinsic resection of the lateral band and oblique fibers of the
MCP joint facilitates mobilization and reflection of the central extensor tendon in a supraperiosteal fashion (2) (Fig. 6-5). The periosteum is incised along the obliquity of the fracture to allow for anatomic reduction and internal fixation. This exposure is especially useful for lateral plate fixation of unstable proximal phalanx fractures. Lateral plate application minimizes interference with extensor tendon excursion. Furthermore, biomechanical analyses (3,4) have suggested that mid-lateral plate positioning may have superior biomechanical properties. Alternatively, the extensor may be split in its midline for wide exposure of the fracture.
MCP joint facilitates mobilization and reflection of the central extensor tendon in a supraperiosteal fashion (2) (Fig. 6-5). The periosteum is incised along the obliquity of the fracture to allow for anatomic reduction and internal fixation. This exposure is especially useful for lateral plate fixation of unstable proximal phalanx fractures. Lateral plate application minimizes interference with extensor tendon excursion. Furthermore, biomechanical analyses (3,4) have suggested that mid-lateral plate positioning may have superior biomechanical properties. Alternatively, the extensor may be split in its midline for wide exposure of the fracture.
Fractures of the distal third of the proximal phalanx can be exposed in a limited fashion for screw placement without incising the extensor mechanism. The lateral band can be retracted dorsally following division of the transverse retinacular ligament as is performed for fixation of unicondylar fractures (as outlined below).
Independent of deep exposure selected, the entire length of the fracture must be exposed, especially with spiral fractures, prior to reduction. The apices must be visualized to confirm anatomic reduction and restoration of length and rotation. Once the fracture is provisionally reduced with bone reduction forceps or K-wires, tenodesis maneuver is performed to confirm restoration of the digital cascade. The fracture-specific fixation construct is then selected.
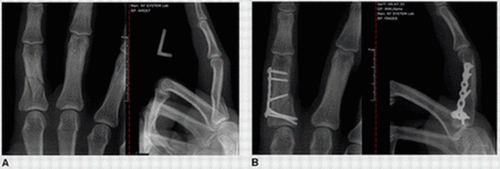
Interfragmentary screws enhance stability compared to K-wires and wire loop fixation constructs. Screws alone are best indicated for the stabilization of oblique and spiral fractures when the length of the fracture is more than twice the diameter of the bone to allow placement
of at least two screws (Figs. 6-6 and 6-7). Obtaining bicortical fixation is more imperative than is true lag compression (5). When planning screw placement, care should be taken to stay a minimum of 2 screw diameters away from the fracture margin to prevent cortical failure. Generally, 1.3-mm and 1.5-mm screws are used depending on fragment size and comminution (Fig. 6-8).
of at least two screws (Figs. 6-6 and 6-7). Obtaining bicortical fixation is more imperative than is true lag compression (5). When planning screw placement, care should be taken to stay a minimum of 2 screw diameters away from the fracture margin to prevent cortical failure. Generally, 1.3-mm and 1.5-mm screws are used depending on fragment size and comminution (Fig. 6-8).
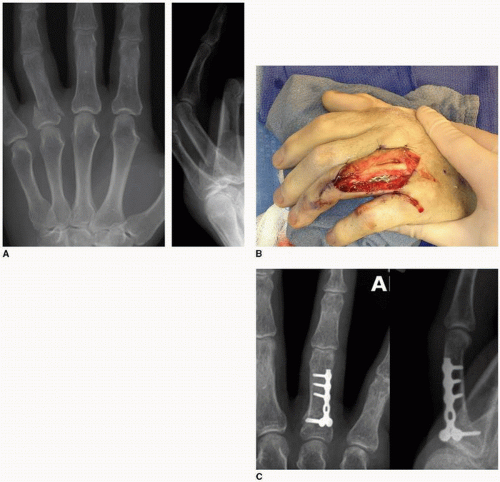
Plate fixation is indicated when K-wire or lag screw fixation is inadequate as in fractures with comminution, articular fractures with extension into the shaft, and for reconstruction of nonunions and malunions. Additionally, there are some fractures such as transverse fractures of the midshaft that are amenable to compression plating.
Plate stabilization is used in multifragmentary and comminuted phalangeal fractures. Complications of plate fixation are related to their use in more complex cases and open fractures
rather than the technique itself (6). Plates can be placed dorsally (Fig. 6-9) or laterally (Fig. 6-10) based on fracture pattern and direction of displacement. While extensor irritation is less likely with lateral plate placement, the latter is also more technically demanding due to the limited area of bone surface available. Generally a minimum of four cortices should be fixed on either side of the fracture.
rather than the technique itself (6). Plates can be placed dorsally (Fig. 6-9) or laterally (Fig. 6-10) based on fracture pattern and direction of displacement. While extensor irritation is less likely with lateral plate placement, the latter is also more technically demanding due to the limited area of bone surface available. Generally a minimum of four cortices should be fixed on either side of the fracture.
Several recent technical advances in plate and screw design have facilitated the application of plates to the phalanges and may reduce complications. New plates are lower profile with varying shapes, thicknesses, and recessed screw heads (Fig. 6-11). A particularly important advance is locking screw technology that allows the screw to thread into the plate hole for added stability. Locking plates are particularly useful for osteopenic bone, for comminuted fractures, and for periarticular fractures where the locking screws buttress the articular surface (7).
External fixators are used for highly comminuted diaphyseal fractures precluding stable internal fixation, combined injuries with bone and soft-tissue loss, and management of infected nonunions necessitating staged reconstruction. External fixation avoids additional soft-tissue dissection and fragment devascularization. Various unilateral fixators are available and multidirectional clamps allow fine tuning of fracture reduction following pin placement.
Reduction of displaced/malangulated distal phalangeal diaphyseal and tuft fractures is considered in the setting of significant sagittal plane deformity in order to repair the lacerated overlying nail matrix. The nail plate is removed and the nail matrix is repaired followed reduction and K-wire fixation of the distal phalanx fracture. Transarticular fixation is often performed to avoid early loosening of the K-wire(s).
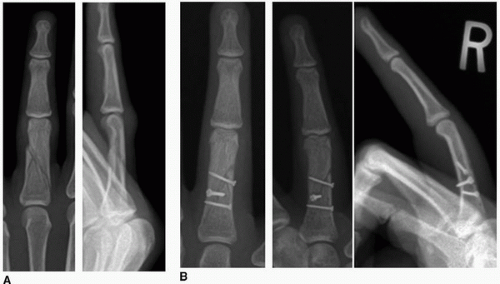 FIGURE 6-8 A: Multifragmentary ring finger proximal phalangeal fracture. B: Appropriately sized interfragmentary screws were used to secure fixation of this multiplanar fracture. |
Pearls and Pitfalls
Unilateral intrinsic resection of the lateral band and oblique fibers of the MCP joint allows for lateral plating of proximal phalangeal fractures and minimizes postoperative extensor tendon adhesions.
Division of the ipsilateral transverse retinacular ligament facilitates lateral band mobilization for distal diaphyseal fractures of the proximal phalanx and unicondylar fractures.
Repair of the periosteum over implants may minimize postoperative adhesions.
Interfragmentary screws are used when the length of the fracture is more than twice the diameter of the bone to allow placement of at least two screws.
Visualize occult nondisplaced fracture lines that may preclude screw fixation.
Use of locking plate designs for comminuted and periarticular fractures.
Postoperative Management
Hand-based intrinsic plus splints are utilized.
Early functional rehabilitation following stable internal fixation is initiated within the first postoperative week. Extensor adhesions are minimized by encouraging early active motion, functional splinting, and edema control.
Reverse blocking splints and exercises are utilized to minimize extensor lag at the PIP joint.
LMB splinting is used to address PIP flexion contractures.
Static and dynamic splints may be needed to address adhesions and joint contractures following clinical union.
Phalangeal Neck Fractures
Isolated subcondylar fractures of the neck of the phalanx are almost exclusively seen in children with the majority occurring in toddlers. The mechanism of injury is usually from crush injury. Al-Qattan (8) classified pediatric phalangeal neck fractures into nondisplaced, minimally displaced with partial contact of the bony fragments, and completely displaced. The distal condylar segment can be displaced dorsally or volarly, and there may also axial plane deformity (i.e., malrotation).
Indications/Contraindications Closed reduction and percutaneous wire fixation is recommended for all displaced fracture of the phalangeal neck. Nondisplaced neck fractures are followed with serial radiographs to confirm maintenance of reduction.
Preoperative Preparation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree