Fig. 10.1
a Lateral position using beanbag body positioner. b Lateral position with surgical leg externally rotated for anterior surgical access
Supine Figure-4 Position
The patient is positioned in supine, and then rolled 15–20° with a wedge placed under the opposite hip. In order for this position to be used, the patient must have adequate external rotation of the hip; therefore, the figure-4 position is not suitable for a patient with increased femoral anteversion. For all of the anterior and arthroscopic work, the hip is slightly internally rotated and flexed to 90°. The surgical leg may be supported with a lateral post and a foot stop, or it may be flexed over the side of the bed. To access the posterior knee, the knee and hip are externally rotated and flexed to approximately 60°. The foot can then be placed on the opposite thigh, making the “4” position. In addition, tilting the table can aid in the visualization of the posterior knee. Laupattarakasem et al. [22] have also described a novel approach, with the surgeon positioned between the patient’s legs to access the posterior knee (Fig. 10.2).


Fig. 10.2
a Modified figure-4 position using a surgical foot stirrup. b Modified figure-4 position with surgeon placement
A significant advantage of this position is that it allows the surgeon to complete the entire inlay PCL reconstruction with the patient in the supine position. This supine figure-4 position also allows the surgeon to use either a posteromedial or a posterior approach. However, there are some disadvantages to this patient position. One of the biggest disadvantages is that the degree and angle of knee flexion makes it difficult to obtain adequate lighting of the operative area from the overhead fixtures and therefore the surgical area is often shadowed. Visualization can be aided with the use of a headlamp to correct this concern. Another disadvantage of this position is the increased difficulty of completing an adequate arthrotomy and debridement of the PCL insertion, because the knee is flexed.
Prone Position
Parker and Bergfeld describe their duo-table technique to achieve the prone position for an open tibial inlay technique [13]. The patient starts in the supine position until the femoral tunnels are drilled and any necessary meniscal work is completed [13]. A separate operating room table is used to roll the patient into the prone position and the patient is redraped [13]. The open tibial inlay technique is then completed through a posterior approach. Once the bone block is secured to the tibia, the patient is rolled back into the supine position and redraped [13]. Alternately, after the patient is anesthetized, it is possible to drape, prepare, and perform the posterior work with the patient in the prone position, and while keeping the patient draped and the field sterile, perform a single turn to the supine position for the remainder of the case.
Once the patient is lying face down with his/her arms comfortably out to the side, place a pillow underneath the patient’s feet to achieve 20–30° of knee flexion . This slight flexion reduces the tension in both the gastrocnemius and hamstrings muscles, which will facilitate posterior exposure of the knee. Pillows may also be placed under the patient’s hips and chest for comfort, and to protect bony prominences. The prone position can be used for either the posterior medial or posterior approaches. The major advantage of the prone position is improved visualization of the posterior knee for the surgical dissection and placement of the tibial inlay graft. The major disadvantage of this position is the time and manpower required to move the patient, along with the risk of contaminating the surgical field during this process.
Surgical Approaches
Posterior Medial Approach
The posterior medial approach was first described by Berg [4]. This method uses the interval between the distal aspect of the medial hamstrings, and the medial head of gastrocnemius. In the original description, the medial head of the gastrocnemius is detached; however, other surgeons have since described leaving this origin intact and flexing the knee to access the PCL insertion site [4, 8, 23, 24]. The skin incision initiates proximally along the medial border of the semitendinosus, then moves laterally and distally close to the midline at the popliteal skin crease, and ends approximately 10 cm distal to the popliteal skin crease. The proximal interval lies between the medial hamstrings and the neurovascular bundle. More distally, the interval is medial to the medial head of the gastrocnemius, which can be reflected laterally by either detaching the medial head proximally, or flexing the knee to relax the muscle (Fig. 10.3). The popliteus muscle is then reflected laterally and distally, and the medial genicular vessels are exposed and ligated or cauterized. This exposes the PCL footprint and the posterior capsule.
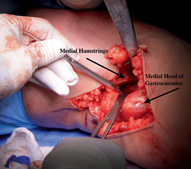
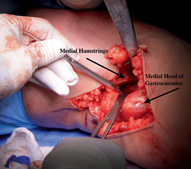
Fig. 10.3
Posterior medial approach
The posterior medial approach can be performed in the lateral, supine figure-4, or prone position. The most positive aspect of this approach is that it provides for protection of the neurovascular bundle with the medial head of gastrocnemius. One of the main challenges for surgeons using this approach is the difficulty in visualizing the posterior capsule and PCL footprint without detaching the medial head of gastrocnemius. This can compromise an adequate arthrotomy, as well as correct positioning of the tibial inlay graft. Additionally, this approach makes it difficult for screw insertion to be perpendicular to the graft bone block, which could potentially compromise the fixation.
Posterior Approach
The posterior approach accesses the posterior capsule and PCL insertion on the tibia directly via the popliteal fossa. Proximally, the interval is located between the medial hamstrings and the neurovascular bundle, and distally between the medial head of gastrocnemius and the neurovascular bundle. This approach is the author’s preferred technique and is described in detail later in this chapter.
This approach can be performed with the patient in the lateral, figure-4 or prone position. The advantage of this approach is direct visualization of all the midline posterior structures, specifically the PCL tibial footprint and the posterior capsule (Fig. 10.4). This approach allows for a well-visualized arthrotomy and debridement of remnant PCL fibers. It also enables insertion and solid fixation of a well-docked graft, and facilitates smooth graft passage. The major disadvantages of the posterior approach are the large posterior incision, the amount of dissection, the time-consuming patient position changes, and the proximity to the neurovascular structures.
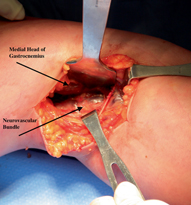
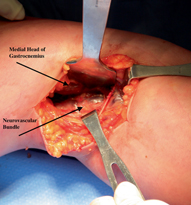
Fig. 10.4
Midline posterior image with neurovascular bundle
Graft Choice
The open tibial inlay technique is amenable to numerous graft options including autografts, allografts, and synthetic grafts. This PCL reconstruction approach was developed during an era when autograft tissue was primarily used for ligament reconstructions [4, 13, 19]. Use of patellar tendon autograft was reported in the early literature [4, 13, 19]. The patellar tendon autograft has many benefits beside the inherent benefit of being autologous. This graft facilitates a bony union at both the tibial and femoral insertions by 4–6 weeks postoperatively, which provides early central stabilization, and may prevent laxity during the more vigorous phases of rehabilitation. The patellar tendon autograft has some disadvantages including the limited amount of soft tissue tendon that can be harvested, (approximately 10–12 mm width and 2–3 mm depth). This amount of tissue is much less than a native PCL. Secondly, the graft length may not allow for the graft to be docked below the crest of the tibial plateau, thus risking proximal migration and/or tilt, if screw fixation loosens during cyclic loading. Lastly, the patellar tendon is not conducive to a double-bundle surgical technique on the femur, limiting this graft type to a single bundle technique.
The quadriceps tendon is another frequently used autograft. It is possible to harvest a large graft, (up to 80 mm length and approximately 6–8 mm depth). Due to the layered structure of this tendon, it can be used in a double-bundle technique on the femoral side. The disadvantages of the quadriceps graft are harvest-site morbidity, including pain, decreased knee function, and reduced quadriceps power [25]. Laupattarakasem et al. described a unique approach using a doubled semitendinosus autograft [22]. The graft is looped over a partially threaded screw, whereby the cortical bone window that was excised for the inlay becomes a washer [22]. The graft is augmented with any remnant posterior PCL fibers and placed under this bony washer [22]. This novel technique is useful for surgeons performing multiligament reconstruction surgery, particularly when allograft tendon is not available, or in a patient with a ruptured patellar tendon. Another advantage of this technique is the biologic bone–tendon–bone healing that it provides. The biggest drawback to using a hamstring autograft is that the size is limited to 6–8 mm width.
PCL reconstructive surgery frequently requires multiple ligament reconstructions and repairs, and therefore more than one graft often needs to be harvested. Considering the substantial degree of trauma that causes PCL injuries, along with the added trauma of harvesting autograft, it is not surprising that allograft tissue has become very popular for these procedures. Preparation and sterilization procedures of allograft tissue have evolved, and the majority of surgeons now prefer to use fresh, frozen, unirradiated allografts. Unirradiated allografts have been reported to produce superior outcomes and a lower failure rate compared with irradiated grafts [26]. For the open tibial inlay technique, the Achilles tendon is often the allograft of choice, but some surgeons use 12–15 mm patellar or quadriceps tendon allografts. The major advantages of allograft tissue are the large graft size as well as reduced harvest site and patient morbidity [27]. In addition, often more than one allograft can be harvested from a single Achilles tendon. The disadvantages of allograft tissue are reduced bone and soft tissue quality, prolonged graft healing, incorporation and remodeling, and the risk of infectious disease transmission [27].
Lastly, there is an option of using synthetic grafts for PCL reconstruction . These are typically completed using a transtibial technique, but some have eyelets that could be secured to the posterior tibia in an inlay fashion. Synthetic grafts may be used to augment native PCL tissue, but are less frequently used in North America than in Europe [28]. These grafts can be useful in the acute multiligament knee injury by enabling the creation of a central joint stabilizer, when other soft tissue damage prohibits multiple ligament repairs.
Author’s Preferred Surgical Approach
Surgical Preparation
The patient is anesthetized in the supine position, the surgical leg is shaved, and a tourniquet is applied to the proximal thigh as a safety measure if any vascular injury occurs. The arthroscopic portals, planned incisions, and the knee joint are all injected with 20 cc of 0.25 % Marcaine with 1/400,000 epinephrine to decrease intraoperative bleeding and postoperative pain. Additionally, 2 g of prophylactic, intravenous cefazolin is administered prior to starting the procedure. This surgery can be performed using either a spinal anesthetic or a general anesthetic. The spinal anesthetic offers the advantage of the patient being able to assist with the position changes. If using a general anesthetic, the anesthesiologist should intubate the patient for maximal airway protection.
Before placing the patient into the prone position, the surgeon performs an examination under anesthesia to confirm the diagnosis. The contralateral extremity should also be examined to assess normal knee ligament function. Prior to the skin preparation, the patient is rolled into the prone position. Perform this patient transfer with the surgical leg uppermost, as this transfer will be repeated in the opposite direction later in the procedure. This will ensure that anesthesia lines and monitoring equipment will not become tangled during position changes. Once in the prone position, place a pillow under patient’s ankles to achieve 20–30° of knee flexion , which will facilitate relaxation of the hamstrings and gastrocnemius muscles. Pillows may also be placed under the patient’s hips and chest for comfort and to protect bony prominences. The patient is prepared for surgery in the prone position. An easy way to assist with the preparation of the entire surgical area is to place one hand under the anterior knee, and to pull the leg up toward the ceiling and away from the body, to ensure the leg stays straight (Fig. 10.5). Once the limb is prepared, drape the patient using a split drape, in addition to a disposable single-hole leg drape, the latter of which will be used during the entire procedure.


Fig. 10.5
Positioning for preparation of the surgical limb
Surgical Technique
With the tourniquet deflated and the use of cautery for hemostasis, perform a classic posterior approach to the knee. Make a 10–15-cm lazy “S” shape incision through the popliteal crease, with a slightly longer distal limb (Fig. 10.6). This nonlinear incision prevents a painful scar or flexion contracture. Incise the fascia with a scalpel and extend the fascial incision using scissors. Identify the superficial sural cutaneous nerve and remain medial to this structure. Using blunt finger dissection, dissect through the fat that is lateral to semimembranosus and the medial head of gastrocnemius until the neurovascular bundle is exposed (Fig. 10.7). The popliteal artery can be palpated during this dissection to confirm you are in the correct interval. Frequently, there is a small neurovascular bundle that innervates the medial head of gastrocnemius, which crosses the field obliquely, and can be preserved (Fig. 10.8). Most often, surgeons will be able to complete the procedure proximal to this bundle. However, in some patients, it is necessary to expose distally from this bundle to properly visualize the tibia for placement and fixation of the tibial inlay graft.
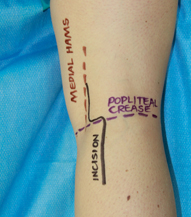

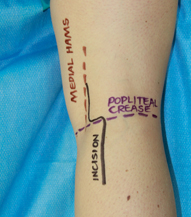
Fig. 10.6
Posterior approach lazy “S” incision

Fig. 10.7
Finger dissection
Fig. 10.8
Neurovascular branch to medial head of gastrocnemius
A Hohmann, or similarly spiked retractor, can be placed medially to retract the medial head of gastrocnemius along with the medial hamstring tendons. Deep dissection on the tibia begins on the medial side, away from the neurovascular structures. The medial genicular artery is cauterized, after which the popliteus muscle is elevated using a soft tissue elevator and reflected laterally and distally. A second Hohmann is added on the posterior lateral tibial plateau where it is hammered into cancellous bone, 3–4 cm below the joint line. This second retractor serves to protect the neurovascular bundle throughout the remaining dissection. The surgeon should now be able to fully visualize the footprint and insertion of the native PCL , along with the posterior capsule (Fig. 10.9).
Fig. 10.9
Footprint and insertion point of the native PCL. PCL posterior cruciate ligament
A formal “L”-shaped arthrotomy is performed on the medial and distal side of the posterior knee joint, away from the neurovascular structures. Often the posterior horn of the medial meniscus can be visualized as a landmark. A medially based arthrotomy also prevents damaging the meniscofemoral ligaments of Wrisberg and Humphrey. The native insertion of the PCL is resected down to its footprint and any remaining bulk of the PCL is excised. If the posteromedial bundle of the PCL is intact, these fibers can be preserved and the tibial inlay graft can be used solely as an anterolateral bundle. These steps allow for easy graft passage, and also prevent graft loosening from delayed necrosis of the injured PCL fibers. The exposure from this dissection facilitates anatomic placement of the tibial inlay graft.
An Achilles tendon allograft is the optimal graft choice due to its size, strength, and the elimination of graft site morbidity. However, either a quadriceps or patellar tendon autograft can be used for patients who are opposed to allografts. Single- and double-bundle grafts can be developed using the Achilles tendon allograft, with current research supporting the use of a large single bundle that mimics the anterolateral bundle on the femoral side [26]. The double-bundle technique is challenging due to the difficult process of precisely mapping two tunnels. This surgical approach often results in two smaller bundles, which are exposed to higher forces, thereby increasing the risk for subsequent graft failure.
An osteotome is used to create an open tibial inlay socket, approximately 1.5 cm in diameter and 3.5 cm in length (Fig. 10.10). Once cancellous bone is exposed, blood will obscure the field, so it is best to start with the technically most difficult distal cut first. Following the distal cut, move laterally next to the neurovascular bundle, finishing with the more straightforward proximal and medial cuts. This sequence minimizes the risk of damaging neurovascular structures after the field becomes bloodied. The placement of the superior aspect of this socket is critical for docking the graft. Ensure that 2–3 mm of solid posterior tibial plateau bone is preserved for this docking process. Proximally, the socket should be 1 cm deep to ensure that the bone block cannot migrate proximally. Distally, it is less important for the socket to be deep, and often the graft is somewhat proud against the tibia. It is important to note that the socket size can vary depending on the size of the patient and the graft being used (Fig. 10.11).