Open Reduction and Internal Fixation of Ulnar Styloid, Head, and Metadiaphyseal Fractures
Eon K. Shin
Peter Goljan
DEFINITION
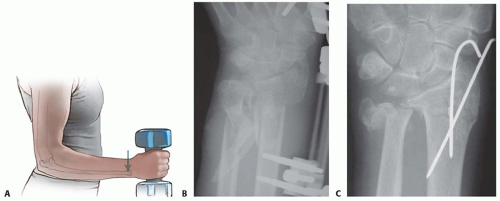
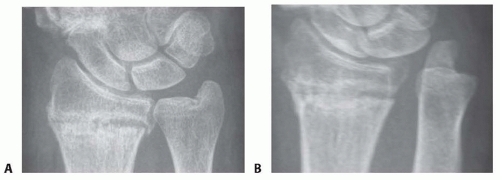
Fractures of the distal ulna are often inadequately treated in comparison to its larger counterpart, the radius (FIG 1B,C).
ANATOMY
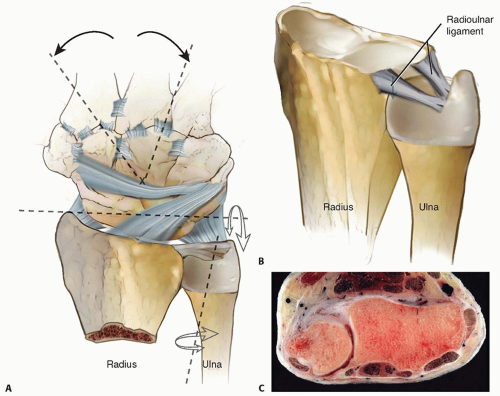
The radius rotates around the ulnar head through the distal radioulnar joint (DRUJ) during forearm pronation and supination.6,7
This joint is connected to the carpus by a complicated ligament apparatus, the triangular fibrocartilage complex (TFCC).
The stability of the DRUJ is achieved through bony congruity between the sigmoid notch of the radius and the ulnar head supported by the radioulnar ligaments1,6 (FIG 2B).
The spheres of the two articular surfaces differ (FIG 2C).
Sixty percent of the joint surfaces are in contact in neutral forearm position.1
In full pronation and supination, there is only 10% bony contact.1
PATHOGENESIS
Isolated ulnar fractures most commonly occur when the forearm is struck by an object, explaining the eponym “nightstick fracture.”
Distal ulnar fractures are most often due to a fall on an outstretched hand.
It is a common understanding that ulnar-sided injuries are more often caused by falls backward in which the forearm is in supination, loading the ulnar side of the distal forearm and wrist and causing distal ulnar fractures, triquetral chip fractures, TFCC injuries, and so forth.
In contrast, radial-sided injuries are more often caused by falls forward, loading the radial side of the forearm and wrist and causing scaphoid fractures, distal radius fractures, and so forth.
NATURAL HISTORY
Many distal ulnar fractures leave only marginal long-term problems.
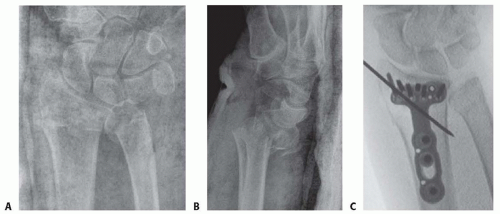
Some distal ulnar malunions cause DRUJ incongruency with subsequent instability or blocked forearm rotation (FIG 3).
This is why management of these deceptive fractures is important.
DRUJ stability is an important treatment goal.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Posteroanterior, lateral, and oblique radiographs typically reveal the pathology.
Computed tomography (CT) is useful in examining articular fractures of the ulnar head.
Magnetic resonance imaging (MRI) can be used to evaluate the integrity of the TFCC.
Arthroscopy should be considered if a radiograph leads the physician to suspect DRUJ dissociation without radiographic explanations, such as a displaced ulnar styloid base fracture.
Diagnostic arthroscopy prior to excision of an ulnar styloid nonunion can be useful to evaluate TFCC integrity.16
SURGICAL MANAGEMENT
Findings and Indications
Distal Radioulnar Joint Dissociation
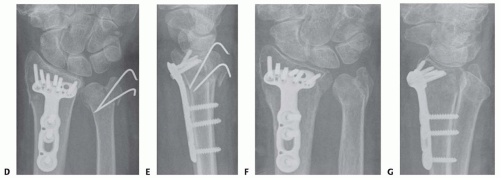
Radiographs occasionally reveal DRUJ dissociation in the absence of an ulnar-sided fracture (FIG 4). This results from detachment of the radioulnar ligament12 (FIG 5A).
Such radioulnar ligament injuries have been found to cause DRUJ laxity and a worse outcome after distal radius fractures in patients without osteoporosis11 (FIG 5B).
Arthroscopically assisted repair or open repair and reattachment of the radioulnar ligament to the fovea of the ulnar head are required to restore stability in the DRUJ (FIG 5C) (see Chap. 63).
Ulnar Styloid Fractures
The importance of ulnar styloid fractures and the need for operative intervention depends on the involvement of the radioulnar ligament insertion site around the fovea of the ulnar head at the base of the styloid (FIG 6A).
Recent literature has demonstrated satisfactory outcomes of distal radius and ulna fractures in which the ulna was left unaddressed following radius fixation.3,10,20
An ulnar styloid nonunion was not demonstrated to cause postoperative ulnar-sided wrist pain.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree