Open Reduction and Internal Fixation of the Talus
David E. Karges
DEFINITION
Fractures of the talus are severe injuries affecting ankle and hindfoot joint function.
Displaced fractures of the talus are a surgical challenge to orthopaedic surgeons. The injuries are infrequent and the fracture anatomy is partially concealed by adjacent osseous structures.
Open reduction and internal fixation is generally mandatory to restore talar anatomy, precisely.
Outcomes of talus fractures correlate with injury severity. These results include ankle and subtalar joint stiffness, posttraumatic arthrosis, and osteonecrosis of the talus.
ANATOMY
Two anatomic factors play significant roles in the outcome of talus fractures.
Sixty percent of the bone is covered by articular cartilage, significantly limiting extraosseous perfusion to the bone.
Disruption of circulation to the talus correlates with open or comminuted talus fractures, leading to an increased risk of avascular necrosis. The blood supply to the talar body enters through the inferior talar neck via the artery of the tarsal canal. This key vessel originates from the posterior tibial artery. Secondary blood supply to the body is derived from the deltoid branch of the posterior tibial artery, entering the talar body along its medial surface. Circulation to the neck, head, and lateral body is supplied via the dorsalis pedis, tarsal sinus, and lateral tarsal sinus arteries. This last artery is an anastomosis between the peroneal and dorsalis pedis arteries.3
Recent latex injection cadaveric study evaluated talar vascularity using gadolinium-enhanced magnetic resonance imaging (MRI) followed by gross dissection.6 Results showed the following:
Peroneal artery contributed 17% talar perfusion.
Anterior tibial artery contributed 36% talar perfusion.
Posterior tibial artery contributed 47% of talar perfusion.
Substantial vascular contribution to the posterior talus support reasons why talar neck fractures may not result in avascular necrosis.
The talus has seven articulations.
Three main surfaces articulate with the plafond and lateral malleolus, whereas three surfaces articulate with the calcaneus.
The final articulation of the talar head with the tarsal navicular represents an important articulation for midfoot motion.
Predictable stiffness with range of motion and posttraumatic arthritic changes is experienced with severe fractures of the talus.
PATHOGENESIS
Fractures of the talus present in varying patterns depending on the mechanism of injury.
Fractures of the talar head are intra-articular and the result of axial load to the talonavicular joint with the foot positioned in plantarflexion.
These fractures constitute up to 10% of all fractures of the talus.
They are uncommon but must be looked for in the event of an isolated subtalar dislocation.
Talar neck fractures occur in the frontal plane and result from dorsiflexion of the foot against the anterior lip of the distal tibia. The fracture begins transversely along the medial talar neck due to an associated supination force to the hindfoot. The fracture line extends laterally. The fracture may be extra-articular, intra-articular, or a combination of both. With increased energy, the hindfoot supination force generates a fracture of the medial malleolus of the ankle.
After completion of the neck fracture, continued hyper-dorsiflexion and axial load to the body of the talus may force dislocation of the talar body posteriorly, disrupting significant extraosseous circulation.
Fractures of the body of the talus involve up to 23% of talus fractures. The mechanism of injury is the same for body fractures as for fractures of the talar neck.
Fracture patterns of the body of the talus include coronal, sagittal, horizontal shear, and crush fractures of the weight-bearing surface.
Process fractures of the talar body are described by anatomic location.
Lateral and posterior process fractures are sustained by inversion and eversion mechanisms of the ankle, respectively. These fractures are often missed on plain film radiographs of the ankle and diagnosed as ankle sprains.
Hawkins classified lateral process fractures into avulsion, isolated, and comminuted types.
Posteromedial and posterolateral process fractures lie to each side of the flexor hallucis longus (FHL) tendon. These are commonly intra-articular fractures of the inferior surface of the posterior talus.
NATURAL HISTORY
The postoperative prognosis for any displaced talus fracture should be guarded because of significant postinjury potential for complication.
Fractures of the head of the talus are commonly nondisplaced because of powerful capsular and talonavicular ligamentous attachments.
Displaced fractures of the talar head have a 10% incidence of osteonecrosis and can lead to secondary posttraumatic arthrosis.
Fractures of the neck of the talus are defined as fractures anterior to the lateral process of the talus. Hawkins’4 work on vertical fractures of the neck of the talus helped clarify injury of vascular perfusion to the bone by delineating three types of fractures of the neck of the talus.
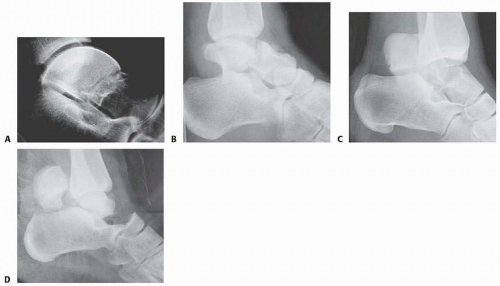
The type I fracture is nondisplaced. Disruption of blood flow is limited to the anterolateral region of the bone. I recommend a computed tomography (CT) scan to confirm no displacement of the fracture before diagnosing a type I fracture. Historically, Hawkins reported a 13% incidence of osteonecrosis in type I injuries (FIG 1A).
In the type II talar neck fracture, there is displacement of the talar dome fragment, which is routinely posterior, often depicting clear subluxation of the talar body. Blood flow to the medial body and head is preserved. The type II talar neck fracture has a 20% to 50% risk of avascular necrosis (FIG 1B).
In the type III injury, the transverse fracture of the talar neck is associated with dislocation of the talar body. The incidence of osteonecrosis of the talar body is 50% to 100%. All major perfusion to the body of the talus is damaged (FIG 1C).
A type IV injury of the talar neck has been documented; it is a type III fracture-dislocation with associated talonavicular dislocation.2 All extraosseous blood flow to the talus is considered disrupted. The value of the Hawkins classification is that it allows the orthopaedic surgeon to predict what to expect with a specific talar neck injury. Open reduction and rigid internal fixation is the recommended treatment (FIG 1D).2
Talar body fractures are defined as fractures extending into or posterior to the lateral process.
PATIENT HISTORY AND PHYSICAL FINDINGS
Fractures of the talus are commonly associated with vehicular trauma and falls.
The relationship of severe lower extremity trauma and airbags is well known. After airbag deployment, the torso and lower extremities are directed toward the floor panel of the car.
I believe that the incidence of high-energy hindfoot trauma will increase over time. Globally, transport-related injuries remain the leading cause of disability from injury. By 2020, traffic injuries will increase from a current ninth position to third disability-adjusted life-years lost.1
The history and the clinical status of the talar injury must be carefully recorded because the injury severity is likely to correlate with the long-term patient outcome.
On the initial examination, the physician should note pain, motion, crepitus, deformity, soft tissue swelling, open fractures, and associated fractures of adjacent bones to the foot and ankle and should perform a complete neurovascular evaluation of the extremity.
Detailed documentation of the talus fracture pattern and local soft tissue injury is paramount.
Soft tissue local pressure phenomenon, commonly found anterolaterally in closed type III fractures of the talar neck, may precipitate full-thickness pressure necrosis of the skin if not decompressed early.
Severe swelling of the ankle is common in the acute fracture of the talus and may progress to fracture blister formation, precluding safe execution of operative incisions.
The physician should examine the skin for swelling, ecchymosis, fracture blisters, and deformity; these are signs of a closed fracture.
A closed injury with mild or moderate swelling (bony landmarks palpable) indicates talar neck type I and II fractures and process fractures.
A closed injury with severe swelling indicates talar neck type III and IV fractures and body fractures.
Open fractures will be apparent by the transverse, medial, or supramalleolar traumatic laceration of the ankle. Lateral, posterior, and plantar wounds are uncommon.
The physician should perform vascular, neurosensory, and myotendinous examinations of the foot and ankle.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Three plain radiographic views are necessary to radiographically evaluate talus fractures: anteroposterior (AP), mortise (15-degree internal rotation view), and lateral images of the ankle.
The AP and mortise views of the ankle demonstrate alignment of the talar body in the ankle mortise. The lateral view depicts the sagittal outline of the talus.
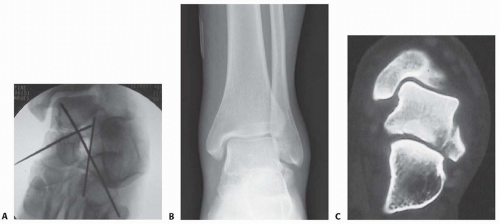
The Canale view is used to assess varus or valgus malalignment of the talar neck, particularly with Hawkins type I and II injuries. The knee must be flexed and the foot in equinus and everted, with the x-ray tube directed 15 degrees caudally (FIG 2A).
Because of the high-energy nature of fractures of the talus, AP and oblique views of the foot should be a standard addition to the three-view plain film ankle protocol so as not to miss associated midfoot and forefoot injuries (FIG 2B).
CT provides important additional information to the threeview plain film series of the ankle. Thirty-degree coronal and paraxial CT imaging is important to confirm Hawkins type I fractures of the talar neck and plan treatment of talar body fractures with extension posterior to the lateral process. Reconstructions of both sagittal and coronal CT studies provide valuable information about incremental pathoanatomy of the entire talus, medial to lateral and anterior to posterior, respectively. In addition, confirmation of a process fracture that is not clearly viewed by plain film is easily diagnosed by CT (FIG 2C).
DIFFERENTIAL DIAGNOSIS
Process fracture of the talus
Lateral process fracture
Medial process fracture
Head of talus fracture
Neck of talus fracture
Body of talus fracture
Neck and body of talus fracture
Fracture-dislocation of talus
Involving body
Involving neck and body
Extruded talus
(Any of these injuries to the talus may be open fractures, affecting management.)
NONOPERATIVE MANAGEMENT
Fractures of the talus include a spectrum of injury patterns ranging from isolated regions of the talus (eg, lateral process) to severely comminuted talus fractures involving all parts of bone, making nonoperative management inappropriate.
High-energy injury mechanisms that cause talus fractures precipitate fracture displacement and joint surface incongruity.
Medial and lateral process fractures, minimally displaced (<2 mm) and involving less than 1 cm of bone, are commonly managed nonoperatively.
These injuries are treated acutely in well-padded, compressive dressings with posterior splints and non-weight bearing. Swelling and immediate pain in the ankle improve significantly by 7 to 10 days. The patient is subsequently converted to a short-leg, non-weight-bearing cast for 6 weeks followed by progressive range of ankle and subtalar motion and return to weight bearing in a removable fracture boot.
If the process fracture is severely comminuted, precluding surgical reconstruction, the same initial and definitive nonoperative management is employed.
Isolated fractures of the head of the talus without dislocation and without displacement are largely stable fractures. These injuries require plain radiographic evaluation of both the ipsilateral foot and ankle to confirm the isolated nature of the injury. I recommend CT scanning (axial and transverse views of foot and ankle) of this injury to rule out associated midfoot pathology.
Acutely, an isolated, nondisplaced talar head fracture is splinted for 7 to 10 days with subsequent short-leg casting
in neutral plantarflexion with non-weight bearing for 4 weeks. Intermittent daily ankle and subtalar motion with Achilles tendon stretching should follow with application of a removable fracture boot. The patient remains non-weight bearing until 6 to 8 weeks after injury. Next, progressive weight bearing, range of motion, stretching, and strengthening of the entire lower extremity are recommended.
The Hawkins type I fracture of the neck of the talus is a nondisplaced talar neck fracture. The talus remains anatomically positioned in the ankle and subtalar joint with minimal potential for disruption of perfusion to the bone.
A subgroup of these injuries may present with displacement of the talar neck on initial injury plain radiographs. After closed manipulation of the fracture in plantarflexion, the talar neck fracture may reduce. A true Hawkins type I talar neck fracture will not displace even with gentle dorsiflexion. The type I fracture strongly warrants a CT scan with sagittal reconstruction to confirm anatomic alignment of the talar neck.
If there is displacement of the neck fracture, the injury must be reclassified as a type II, which requires surgical treatment to obtain, and maintain, the reduction.
Truly nondisplaced fractures of neck of the talus can be treated nonoperatively in a short-leg, non-weight-bearing cast for 6 to 8 weeks. Close follow-up is recommended to watch for any displacement of the neck fracture. At 6 to 8 weeks after the injury, progressive weight bearing, range of motion, stretching, and strengthening are initiated.
Injury forces precipitating fractures of the dome of the talus are universally severe, causing articular displacement, and are an indication for surgery. Open fractures of the talus, even with no displacement, are best managed with rigid surgical stabilization to allow for wound care and early motion.
SURGICAL MANAGEMENT
The timing of operative management of talus fractures has been an area of controversy, specifically whether the displaced talus fracture is an orthopaedic emergency.
One recent study indicates that orthopaedic trauma surgeons do not believe that a displaced fracture of the neck of the talus is an orthopaedic emergency.
However, it is important to differentiate the potential of vascular injury to the talar body from soft tissue and neurovascular compromise of the foot because of injury to the talus. In particular, fracture-dislocation of the body of the talus is associated with compromised blood flow to the bone, the threat of pressure phenomenon to the skin, and possible tibial nerve dysfunction.
The acute severity of soft tissue swelling or the impact of an open hindfoot wound may preclude safe, immediate reconstruction of the talus fracture after reduction of the dislocation.
Foot and ankle external fixation is a suitable treatment option, with staged definitive fixation applied accordingly.
Any open talus fracture must be treated as an orthopaedic emergency.
Preoperative antibiotics may be selected on the basis of wound contamination. These include a cephalosporin and possibly gentamicin. Penicillin is added if gross or farm contamination is present. All patients should receive a tetanus toxoid booster.
The patient is taken to the operating room, and after soft tissue débridement, the wound receives at least 3 to 9 L of normal saline using pulsed lavage.
At this time, in addition to partial or complete fixation of the talus fracture, provisional foot and ankle external fixation may be used to provide soft tissue and osseous stabilization before delayed closure.
Regarding general guidelines for fractures of the body, neck, and head of talus fractures, surgical management is indicated with fracture displacement, malalignment, subluxation, dislocation, or instability.
Recent studies indicate that displacement or malalignment will have a negative impact on foot function. Two millimeters of fracture displacement has been shown to affect subtalar joint mechanics.
There is less agreement regarding surgical indications for process fractures of the talus. Acute, displaced fractures with large fragments showing extension into the subtalar joint by CT imaging are best treated with open reduction and internal fixation.
A displaced fracture of the neck of the talus is one of the most common indications for surgery on the talus. The fracture is known to start in the coronal plane, along the medial neck, and extend laterally until completion.
There are two common types of neck fractures: an extraarticular pattern and an intra-articular type that extends into the subtalar joint.
The displaced extra-articular vertical neck fracture is routinely amenable to closed reduction by applying dorsal to plantar pressure on the head of the talus associated with longitudinal traction and plantarflexion of the forefoot. Immediate reduction of this fracture diminishes concerns for soft tissue, neurovascular, and osseous compromise.
The intra-articular pattern is less likely to cooperate with closed manipulation owing to the obliquity of the fracture as it extends posterior into the subtalar joint. This fracture pattern is more deserving of immediate or early surgery.
For patients with severe open fractures of the talus or closed injuries in which soft tissue compromise precludes immediate open management, temporizing external fixation may be effective.
The goals of temporary external fixation are to maintain the length of the talus for reconstruction, facilitate soft tissue management, and restore general alignment. External fixation is a temporary form of management for talus fractures until internal fixation can be safely performed.
Displaced, open or closed, fractures benefit most from rigid internal fixation for bone healing and early motion. However, a recent report evaluating results of the extruded talus identified definitive external fixation as an option to manage the purely dislocated talus. This is an excellent treatment option to stabilize the ankle and subtalar and talonavicular articulations of the talus.
Preoperative Planning
Operative planning for talus fractures requires evaluation of imaging studies to clearly understand the relationships of all major fracture fragments.
A preoperative CT scan of the fracture is standard when confronted with a comminuted talar neck or body fracture. The surgeon must become familiar with the morphology of the bone and its many contours to facilitate reconstruction.
Intraoperative visibility and access to talar fragments are routinely challenging, but these variables can be largely facilitated by correct patient positioning, surgical approaches, adequate operating room lighting (headlamp), attention to reduction techniques, and implants selected. All play a key role in preoperative planning.
The principles of open treatment are restoring articular congruity, maximizing the revascularization potential of the bone, and allowing early motion of the ankle and subtalar joints.
The use of a radiolucent table and a headlamp promotes optimal visualization.
A tray of fine-tipped, sharp and strong bone elevators; dental probes; Freer elevators; small bone clamps; mini/small lamina spreaders; and small distractors or external fixation equipment is routinely needed not only for talus fracture fixation but also for all fine articular fracture reconstructions.
Small interfragmentary (3.5 mm) cortical screw fixation and minifragment (2.7 or 2.0 mm) screw/plate instrumentation is commonly needed for talus fracture fixation.
An extra-long mini-screw (2.7 or 2.0 mm) inventory is recommended, with screws up to 60 mm long.
The use of mini-implants is particularly helpful when reconstructing comminuted fractures.
Contemporary minifragment systems are predominantly stainless steel.
Some authors have suggested using titanium implants to allow use of MRI to assess osteonecrosis.
Caution to tap long mini-screws (>30 mm) directed through dense talar body bone before insertion to avoid difficulty with insertion or shearing of mini-screw head.

FIG 3 • A. Supine position for medial and anterolateral approaches. B. Supine position for direct lateral approach. C. Prone position for posterior approach.
Osteochondral fragments too small for minifragment fixation can be fixed with bioabsorbable pegs or headless articular screws.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree