Open Reduction and Internal Fixation of the Posterior Wall of the Acetabulum
Jodi Siegel
David C. Templeman
DEFINITION
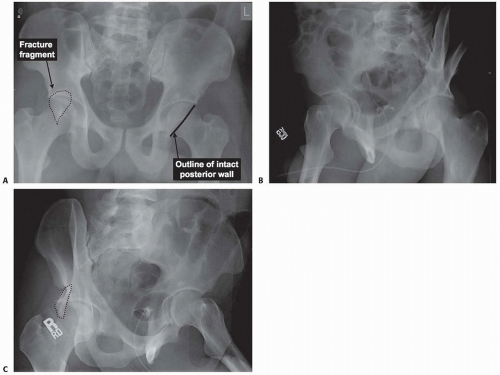
A posterior wall fracture is one of the elementary fracture types as described by Letournel and Judet.6 It is a fracture of the posterior rim of the socket portion of the ball-and-socket joint of the hip (FIG 1).
The disruption separates a segment of articular surface that involves varying amounts of the bony posterior wall of the acetabulum. It can exist as one single fragment or as several comminuted pieces.
The wall fracture can exist alone or as part of an associated acetabular fracture.
By definition, the posterior column, and therefore the ilioischial line, remains intact despite varying amounts of retroacetabular surface disruption.
ANATOMY
The hip is a constrained ball-and-socket joint composed of the femoral head as the ball and the acetabulum as the socket.
The capsule surrounding the joint extends from the bony acetabular rim to the intertrochanteric line anteriorly and to the femoral neck posteriorly. It is thickened in specific areas, creating ligaments.
Anteriorly, the iliofemoral Y ligament exists as two bands. The inferior capsule is supported by the pubofemoral ligament and the posterior capsule is strengthened by the ischiofemoral ligament.
The acetabular labrum is a fibrocartilaginous structure attached to the bony rim, deepening the socket and making
the joint more stable. It adds an additional 10% of coverage to the femoral head.
The acetabulum is composed of two columns, two walls, and the roof within the pelvis. The anterior and posterior columns form an inverted Y and are attached to the sacrum via the sacral buttress. The articular surface of the joint sits on the anterior and posterior walls and the roof, which is located within the arms of the Y.
The anatomic roof is located between the anterior inferior iliac spine and the ilioischial notch of the acetabular margin.6
The weight-bearing dome, as determined by 45-degree roof arc measurements on anteroposterior (AP) and Judet radiographs, is the most important articular portion of the acetabulum. This functional aspect of the acetabulum includes the excursions of all resultant force vectors during normal daily activities.9
Two additional segments should also be considered separately.
The posterosuperior segment is the bridge between the roof and the posterior wall.
The posteroinferior segment is the lower part of the posterior wall and the posterior horn of the cartilage.6
Due to the large area of muscular attachments, the blood supply to the acetabulum is vast.6 Small arteries start peripherally and flow centrally, parallel to each other.
The largest nutrient foramina on the internal aspect of the ilium is reliably located 1 cm lateral to the sacroiliac joint and 1 cm above the iliopectineal line. It is fed by a branch of the iliolumbar artery.
A branch of the superior gluteal artery feeds the largest nutrient foramina on the external surface in the center of the iliac wing, just anterior to the anterior gluteal line.
The obturator artery supplies foramina in front of the sciatic notch just below the iliopectineal line and in the roof of the obturator canal. The body of the pubis is also supplied by the obturator artery. A branch of this artery, the acetabular branch, feeds the cotyloid fossa via a number of small perforators.
A complete vascular circle supplies multiple nutrient vessels around the periphery of the acetabulum. The artery of the roof of the acetabulum (from the superior gluteal artery), the obturator artery, and the inferior gluteal artery are main contributors.
The iliac crest, from the anterior inferior iliac spine posteriorly to the auricular articular surface of the sacroiliac joint, is supplied by branches of the external anterior iliac artery, branches of the fourth lumbar artery, and branches of the iliolumbar artery.
The sciatic buttress receives its blood supply from multiple branches of the superior gluteal artery.
PATHOGENESIS
Acetabular fractures occur when a force is transmitted from the femur, through the femoral head, to the acetabulum. The specific pattern of the fracture is determined by the position of the hip at the time of injury and the magnitude of the force of the trauma.
A common mechanism of injury of posterior wall fractures and fracture-dislocations is a motor vehicle crash in which the unrestrained patient is sitting with a flexed knee and the knee strikes the dashboard, creating an axial load along the length of the femur, loading the posterior aspect of the acetabulum.
Posterior wall fractures of the acetabulum occur when the hip is flexed to 90 degrees and is in neutral coronal and axial plane orientation. In this position, when an axial load is applied to the femur, the posterior articular surface of the joint is stressed. The amount of comminution, displacement, and articular impaction will depend on the quality of the bone and the magnitude of the force.
A typical posterior wall fracture is completely below the roof of the acetabulum.
With less hip flexion and a force applied along the axis of the femoral shaft, a superior posterior wall variant will result, which includes part of the adjacent roof.
A posterior inferior fracture includes the inferior horn of the articular surface, the subcotyloid groove, and often the superior ischium.
Extended fractures, massive posterior wall fractures, and transitional forms are mentioned for completeness but are outside the scope of this chapter.
A variation of a posterior wall fracture is a fracturedislocation, which involves single or multifragmented pieces of the posterior wall separated by the dislocating femoral head. This pattern is often associated with impaction of the articular surface of either the head or the wall (FIG 2).
With a posterior wall fracture or fracture-dislocation, one of two possibilities exists for the capsule.
The capsule can rupture and allow the head to dislocate.
In this scenario, varying sizes of wall fragments and labral injury can exist.
Alternatively, the capsule can remain intact to the wall fragment and to the femur, with all of the displacement (or even the dislocation) occurring through the fracture site.
The size of the posterior wall fragment and the integrity of the capsule and the labrum play a role in hip stability.
Despite attempts to quantitate fragment size to define operative indications,2, 5, 7, 16 stress examination remains the only method to predict instability.14
When the capsule remains intact and the head dislocates, the fracture edges often fragment. This creates osteochondral fragments, which can lead to impaction or incarceration of the pieces upon reduction of the femoral head.
NATURAL HISTORY
The goal of the treatment of acetabular fractures is to achieve a stable, congruent hip joint with an anatomically reduced articular surface. Anatomic reduction and stabilization will decrease the incidence of posttraumatic arthritis.8
Although fractures of the posterior wall are common, representing 24% of Letournel and Judet’s initial series, they are frequently reported as having poor results, with 10% to 30% of patients developing posttraumatic arthritis within 1 year.
Nonoperative treatment is unsuccessful, and Epstein3 has documented that 88% of patients treated with closed reduction alone had unsatisfactory long-term results.
Roof arc and subchondral arc measurements do not apply to typical posterior wall fractures; however, the size of the posterior wall fragment may play a role.
Multiple authors have attempted to define the size of the fragment that will predict instability.
Dynamic stress examination that uses fluoroscopy to assist with the detection of subtle subluxation can define a stable or unstable joint without depending on fragment size measurements.14
PATIENT HISTORY AND PHYSICAL FINDINGS
Acetabular fractures are often the result of high-energy trauma, therefore other associated injuries must be sought.
Hemorrhage and hemodynamic instability are rarely associated with isolated fractures of the posterior wall; however, the superior gluteal artery and vein may be lacerated when fractures extend to the greater sciatic notch.
Patients will frequently present with hip or groin pain and a shortened lower extremity due to the posterior, superior dislocation of the femoral head.
Soft tissue injuries around the pelvis are uncommon because the mechanism of injury is indirect. Nonetheless, the skin overlying the hip and pelvis of any pelvic or acetabular fracture should be carefully evaluated for any subcutaneous fluctuance, ecchymosis, or cutaneous anesthesia.
The Morel-Lavallée lesion, a subcutaneous degloving injury, although a closed injury, is culture positive in up to 40% of cases.4 Initial débridement of these lesions as well as a delay in internal fixation is recommended by some authors.
Soft tissue injuries at the knee are more common and often missed. Ligamentous or chondral injuries are often discovered on secondary survey, but only if they are considered and a careful and thorough examination is performed.
The incidence of damage to the femoral head is unknown as the head is not routinely dislocated during fixation of the acetabular fracture for complete evaluation. However, it is not surprising when associated femoral head fractures or chondral lesions are noted as the large amount of force needed to cause the acetabular fracture is transmitted via the femoral head.
Careful neurologic examination at the time of injury reveals deficits in up to 30% of cases. The peroneal division of the sciatic nerve is the most commonly seen nerve injury, especially when the femoral head is dislocated posteriorly.
Other ipsilateral extremity injuries often discovered include fractures of the femur, tibia, and foot.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The diagnosis and classification of an acetabular fracture is made from the initial trauma AP radiograph.
Two 45-degree oblique radiographs (Judet views) must be obtained also to aid in classification and treatment planning.
Completing the five views of the pelvis series with pelvic inlet and outlet views allows potential injuries to the pelvic ring to be evaluated.
A computed tomography (CT) scan of the pelvis will assist in defining displacement, intra-articular fragments, marginal articular impaction, and associated femoral head injuries.
The size of the posterior wall fragment can also be determined more accurately using a CT scan, which is optimally obtained after the initial reduction.
The size and number of incarcerated fragments can be more precisely determined with a CT scan. Preoperative planning allows determination of the size and number of free fragments that must be removed from the joint as well as the location of any impaction that must be elevated.
DIFFERENTIAL DIAGNOSIS
Posterior hip dislocation
Associated acetabular fracture
Associated transverse and posterior wall fracture
Associated posterior column and posterior wall fracture
Associated T-shaped fracture
Associated both-column fracture
Pelvic fracture
Femoral head fracture
Proximal femur fracture
NONOPERATIVE MANAGEMENT
Nondisplaced, stable fractures with a congruent joint can be treated with protected, foot-flat weight-bearing restrictions if no instability is evident on fluoroscopic-assisted stress examination.14
Posterior wall fractures that present dislocated should be considered a surgical emergency.
A prompt closed reduction with satisfactory general anesthesia is recommended.
The surgeon should check the femoral neck before reduction.
Once reduced, the joint should be evaluated fluoroscopically in both the AP and obturator oblique views for stability: The joint should be axially loaded with the hip in flexion and in flexion plus adduction.14 Only if the joint is stable (nonsubluxated) is nonoperative management sufficient.
SURGICAL MANAGEMENT
Surgical management of acetabular fractures is technically demanding. The goal of surgery is to obtain an anatomic reduction of the joint surface and to create a congruent and stable hip joint while avoiding complications.
Other factors that play a role in surgical management include surgeon experience and the timing of operative intervention.
Letournel and Judet described their learning curve in 4-year intervals.
They also reported reduced ability to achieve anatomic reduction when fractures are operated on more than 21 days after injury.
Unlike most conditions in orthopaedic surgery, all displaced fractures of the acetabulum, which include marginal impaction, are indicated for surgery unless specific criteria for nonoperative management are met.15 These include the following:
A congruent hip joint on AP and Judet radiographs and on CT scan
An intact weight-bearing surface, as defined by roof arc measurements and subchondral arc measurements on CT scan
At least 50% of the posterior wall intact on CT scan
A stable joint, including on a dynamic stress examination
Patient factors must also be considered.
Age, bone quality, comorbidities, preinjury functional status, type of employment, and personal expectations all must factor into the decision-making process.
Preoperative Planning
Open reduction and internal fixation of a posterior wall fracture is based on evaluation of the AP pelvic and Judet view radiographs and the CT scan.
The surgeon should closely evaluate the films for a transverse component, which may be overlooked on initial viewing.
The identification of marginal impaction necessitates elevating the articular cartilage and packing behind it with some form of bone graft or bone void filler to reconstruct the joint surface successfully (see FIG 2).
Careful review of the CT scan will allow identification and quantification of the number of intra-articular fragments that exist to ensure that all foreign bodies are removed from the joint upon exploration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree