In orthopaedic surgery, the terms pilon and plafond have been loosely translated and interchangeably used to describe the weight-bearing portion of the distal tibial articular surface.
These injuries account for approximately 1% of all lower extremity fractures and 5% to 10% of tibial fractures.
Most orthopaedic surgeons will encounter these injuries during the course of their practice, thus a basic understanding of their characteristics and their management possibilities is important for any practicing orthopaedist exposed to trauma.
Open reduction with internal fixation (ORIF) remains the basis by which most pilon fractures are operatively stabilized.
As established by Rüedi and Allgower,15 the goals of any surgery for pilon fractures should include precise articular reconstruction, restoration of extremity length and alignment, stable fracture fixation, and early joint motion.
ORIF presents some difficulties during the management of pilon fractures as it may further compromise the thin soft tissue envelope surrounding the distal tibia, that is, wound complications and infection.
Modern techniques (eg, staged management using temporizing external fixation) in fracture care are useful in minimizing potential complications associated with open treatment in this unique location.
Pilon fractures involve the weight-bearing articular surface of the distal tibia. In approximately 90% of cases, there is an associated distal fibular fracture.
The talus is predominantly cartilage-covered and sits in the ankle mortise beneath the tibial pilon and is restrained medially and laterally by the malleoli.
The mechanism of injury for articular fractures of the distal tibia usually involves some degree of axial compression as the dense talus impacts into the tibia’s distal articular surface.
The distinction between fracture patterns is thus attributed to a number of other associated variables, such as the amount of rotational forced involved, foot (talus) position during loading, bone quality, and energy of impact.
Highly comminuted articular injuries usually occur due to high-energy axial loading forces, whereas spiral fractures with minimal articular injury are presumed to result from lower energy rotational forces. True bending injuries are seen less commonly and may be caused by low- or high-energy causes.
Despite the absence of a clear spectrum of injury severity, an estimation of the energy involved in a pilon fracture can be assumed from aspects other than the tibial fracture pattern itself (eg, history, soft tissue injury, associated injuries).
Open injuries occur in approximately 15% to 40% of pilon fractures, reflecting the severity of the injury and the necessity for aggressive soft tissue management.
Associated injuries should be carefully investigated as 5% to 10% of pilon fractures are bilateral, 30% have ipsilateral lower extremity injuries, and 15% have injuries to the spine, pelvis, or upper extremities.
Although a number of injury combinations is possible in the distal tibia, characteristic patterns can often be identified. Understanding the pattern of injury is critical to formulating an optimal treatment plan.
Lower energy metaphyseal or diaphyseal involvement of the tibia is typically spiral in nature with a cortical spike that can guide the reduction.
Metaphyseal comminution just above the articular pilon is resultant of high-energy axial loading, as the talus impacts into the corresponding weight-bearing surface of the tibia. In such injuries, the anterior pilon is often comminuted and impacted into the adjacent metaphysis.
The Orthopaedic Trauma Association’s (OTA) Committee for Coding and Classification has developed its alphanumeric system6 from the AO/ASIF (Arbeitsgemeinschaft für Osteosynthesefragen-Association for the Study of Internal Fixation). This alphanumeric system is popular among fracture surgeons and is used in most current reports of fracture treatment.
Distal tibial fractures are designated as types 43-A, B, and C, with further subgrouping based on specific fracture characteristics (FIG 1).
The three major types—A (extra-articular), B (partial articular), and C (intra-articular extension with complete separation between the articular fracture fragments and the tibial shaft)—are further divided into subgroups based on the amount of fracture comminution, articular depression, and overall displacement.
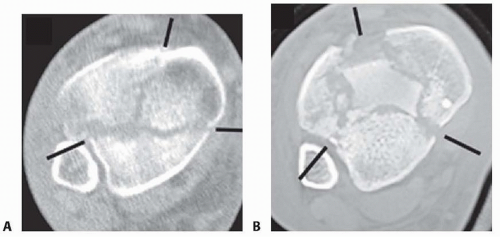
Cole and associates5 mapped 38 consecutive AO/OTA 43-C3 (complex articular) pilon fractures with computed tomography (CT) scans and found that all pilon fractures in this category exited the tibiofibular joint laterally and at two separate locations medially to create a coronally oriented “Y” pattern with three major fragments (FIG 2A,B). Additionally, there were varying amounts of articular comminution anterolaterally or anteromedially (FIG 2B).
The three “major” pilon fragments seen in comminuted complete articular (AO/OTA 43-C) injuries can be described as follows:
First, a posterior pilon fragment develops with a fracture line exiting 1 to 4 cm proximal to the articular surface (in partial articular injuries [AO/OTA 43-B], the posterior pilon often remains intact).
An anterolateral pilon fracture fragment of varying size separates with its anteroinferior tibiofibular ligament attachment. This anterolateral tubercle of Chaput requires fixation to restore the anatomy and function of the syndesmosis complex.
A medial malleolar fracture is identified as the third characteristic fragment.
Isolated osteochondral fragments of variable size are often encountered (typically central to anterolateral in location; see FIG 2B) and constitute the remaining portion of the articular surface.
High-energy injuries can extend into the tibial diaphysis with fibular fractures proximal to the articular level.
Finally, the syndesmosis will be functionally disrupted, secondary to the fibular fracture and anterolateral pilon separation. The syndesmosis anatomy and function can be restored by fixation of both the fibula and anterolateral pilon. As such, tibiofibular syndesmotic screw fixation is rarely required.
In contrast to high-energy patterns, rotational injuries (FIG 3) cause spiral fractures of the distal tibia and fibula. The fibular fracture commonly originates at the articular level. Intraarticular injury, if present, is typically simple and without comminution or impaction.
On one end of the spectrum, high-energy vertical compression injuries result in comminuted articular fractures with compromised surrounding soft tissues. On the other end, low-energy rotational injuries with minimal axial compression produce more straightforward spiral fractures with less soft tissue damage and a more favorable prognosis.
Where a particular fracture pattern falls within this spectrum can often predict the eventual outcome of the injury.
Unfortunately, determining the outcomes from these fractures is not straightforward as existing classification systems fail to clearly distinguish the spectrum of injury, making a fair comparison of published outcomes difficult to achieve.
The surgeon maintains an important role in affecting the final outcome of these injuries, principally by designing a treatment plan that accomplishes the surgical goals detailed previously while minimizing the risks of complications.
Established variables that clearly affect outcome include avoiding complications while restoring a congruent articular surface as well as the axial alignment of that articular surface relative to the shaft.
The injury history is usually clear and often involves a fall from heights, motor vehicle crash, motorcycle crash, or sports injury. Occasionally, a patient will simply misstep on stairs or a curb. A simple, low-energy mechanism should prompt consideration for osteoporosis evaluation.
These patients are usually injured by high-energy means and should be evaluated as trauma patients and according to advanced trauma life support (ATLS) protocols.
All associated injuries must be identified and formulated into the global treatment plan.
Table 1 Tscherne and Gotzen Grading System for Closed Fractures
Grade
Description
0
Little/no soft tissue injury
1
Superficial abrasion and mild to moderately severe fracture configuration
2
Deep, contaminated abrasion with local contusional damage to skin or muscle and moderately severe fracture configuration
3
Extensive skin contusion or crushing or muscle destruction and severe fracture
Comorbidities such as diabetes mellitus, vascular disease, tobacco usage, and chronic immune or inflammatory disease may affect treatment and risk stratification. The medication profile should be assessed for blood thinners, antiinflammatories, and others that may affect surgical risk or bone metabolism.
A meticulous examination with special attention to soft tissue and neurovascular status is important in the evaluation and classification of these fractures (Tables 1, 2, 3).
With wound complication rates having a historic potential of 50%,12, 20 recognition and appropriate management of the soft tissue injury cannot be overemphasized.
Table 2 Gustilo and Anderson System for Grading Open Fractures
Grade
Type of Trauma
Wound size
Soft Tissue Injury
I
Low energy
<1 cm
Minimal
II
Intermediate energy
>1 cm
Moderate
III
High energy
>10 cm
Severe, with crushing
Table 3 Methods for Examining the Distal Leg
Examination
Technique
Grading
Significance
General appearance
Observation for swelling, blisters, wounds, ecchymosis
Closed injury: (Tscherne and Gotzen)
0: Injury from indirect forces with negligible soft tissue injury
1: Superficial contusion/abrasion, simple fractures
2: Deep abrasions, muscle/skin contusion, direct trauma
3: Excessive skin contusion, crushed skin/muscle, subQ degloving, compartment syndrome
Open injury: (Gustilo and Anderson)
1: Low energy, <1 cm wound
2: Intermediate energy, 1-10 cm wound
3: High-energy, blast/crush, contaminated, > 10 cm
3a: Adequate soft tissues for coverage
3b: Inadequate soft tissues, requires soft tissue reconstruction
3c: Associated vascular injury requiring repair
Increased surgical risks until soft tissues have improved.
Vascular
Palpating pulses and Doppler tones. Compare to contralateral side.
“Allen test of the leg” to assess for a single vessel injury (eg, ant. tibial artery), compress posterior tibia artery while palpating dorsalis pedis (DP) artery. If the DP pulse disappears, there is likely injury to the anterior tibial artery and DP flow is occurring retrograde through the forefoot collateral arch.
Pulse grading:
0: Absent
1 +: Barely palpable
2 +: Normal
3 +: Enlarged
4 +: Aneurysmal
Increased surgical risks for wound problems, infection, failed treatment. Alternative approaches
Neurologic
Light touch and motor examination
Quantify light touch
Charcot problems Medicolegal
Associated injury (foot, talus, knee, hip, lumbar spine)
Observation, palpation, and ROM
N/A
Avoid missed injury.
SubQ, subcutaneous; ROM, range of motion.
Inspect and document wounds, swelling, ecchymosis, blisters, ischemic skin, and chronic skin/vascular changes.
Identify open fractures.
Establish “personality” of the injury.
A careful vascular examination is important in evaluating patients with high-energy pilon injuries, as arterial compromise appears to be more common than previously appreciated (which may help explain the relatively high complication rates seen with early ORIF).
Findings of vascular compromise may be subtle (such as a one vessel injury, eg, anterior tibial artery) due to collateral/retrograde flow patterns. Arterial compression testing (Allen test) about the ankle, ankle-brachial indices, or the addition of angiography to CT may be a useful tools to further evaluate the local vasculature.
Rarely, compartment syndrome may occur creating the need for urgent operative intervention.
The diagnosis of tibial pilon fracture is initially evaluated with three radiographic views of the ankle (anteroposterior [AP], mortise, and lateral) (FIG 4A).
These views should be repeated after all “reductions” including application of temporizing external fixation.
CT scans have been clearly shown to improve a surgeon’s understanding of the injury (see FIGS 2 and 4F) and are critical to preoperative planning for complex injuries.21
For displaced, comminuted pilon fractures, the best time to obtain a CT scan is after temporizing external fixation is performed (FIG 4C), when the fracture length is restored. This tends to grossly reduce many parts of the fracture, making the pathoanatomy of the injury more understandable (FIG 4B,D,E).
The addition of angiography to CT is considered for assessing the arterial tree of the distal leg before pilon reconstruction if vascular injury is suspected (FIG 4G). Occult vascular injuries, especially of the anterior tibial artery, do occur with some frequency in high-energy pilon fractures and may contribute to wound complications postoperatively if not recognized.
Tibial shaft fracture
Ankle fracture or dislocation
Talus fracture
Nonoperative treatment should be reserved for nondisplaced or minimally displaced fractures that are determined to be stable and have little comminution and soft tissue injury.

FIG 4 • (continued) F. Axial CT showing articular injury pattern. G. Three-dimensional reconstruction of CT angiogram demonstrating deficient flow through anterior tibial artery.
This scenario is uncommon, however, as the amount of energy necessary to fracture the tibial pilon usually results in significant fracture displacement and resultant instability.
Some consideration may be given to nonoperative treatment in the infirmed or neuropathic patient, although the risks of splinting or casting are often greater than for operative treatment.
Attempts at casting or splinting unstable pilon fractures in patients considered to be poor candidates for operative treatment (ie, elderly, diabetics, vasculopaths, etc.) are fraught with risks for progressive deformity, skin break down, and amputation.
The presence of other musculoskeletal injuries becomes a strong relative indication for surgical treatment of the pilon fracture as surgical stabilization may allow for easier mobilization and rehabilitation.
Reasonable conservative treatment options include non-weight bearing with casting or bracing until radiographic signs of healing are visualized.
Regular follow-up and radiographic vigilance is needed to ensure that articular congruity and axial alignment of the lower leg remain satisfactory.
Protected weight bearing (PWB) must be individualized in each case, but usually, greater than 10 to 12 weeks of PWB is necessary to safely maintain alignment.
Displaced tibial pilon fractures generally require surgery. ORIF is the preferred method of treatment for such displaced fractures to achieve the goals previously outlined by Ruedi and Allgower.15
ORIF is reserved for those fractures where the soft tissues allow such a surgery within a reasonable time frame (ie, 5 to 21 days from the injury) as determined by the surrounding soft tissue appearance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree