Open Reduction and Internal Fixation of Supracondylar and Intercondylar Fractures
Joaquin Sanchez-Sotelo
PATIENT HISTORY AND PHYSICAL FINDINGS
Distal humerus fractures occur in two age groups:
Younger patients who sustain high-energy trauma
Older patients with underlying osteopenia
Comminution is the dominant feature of supracondylar and intercondylar fractures and complicates internal fixation. The complicated skeletal geometry of the distal humerus also contributes.
The goals of the initial evaluation are to
Understand the fracture pattern
Determine the existence of previous symptomatic elbow pathology
Determine the extent of associated soft tissue (open fractures)
Identify associated musculoskeletal or neurovascular injuries
IMAGING AND OTHER DIAGNOSTIC STUDIES
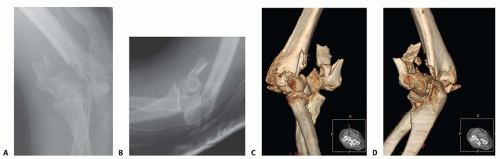
Elbow radiographs in the anteroposterior and lateral planes are the first imaging studies obtained and should be carefully scrutinized to identify the fracture lines and fragments as well as the extent of comminution. It is also important to look for associated injuries in the proximal radius and ulna.
A complete understanding of the fracture pattern is difficult to obtain based only on simple radiographs because of the complex geometry of the distal humerus and fragment overlapping (FIG 1A,B).
Computed tomography (CT) with three-dimensional reconstruction is extremely helpful, especially in the more complex cases. It allows the surgeon to look for specific fractured fragments at the time of fixation, facilitating accurate fracture reduction (FIG 1C,D).
Traction radiographs obtained in the operating room with the patient under anesthesia just before surgery also can be helpful, especially if a CT scan is not available.
SURGICAL MANAGEMENT
Internal fixation is the treatment of choice for most fractures of the distal humerus.
Modern fixation techniques seem to benefit from the following:
Fixation strategies designed to improve the mechanical stability of the construct
Use of precontoured periarticular plates
Use of screws locked to the plates
Elbow arthroplasty should be considered in elderly patients with previous elbow pathology or in very low comminuted fractures in patients with osteopenia.12,14 However, internal fixation can be successful even in low transcondylar fractures.18
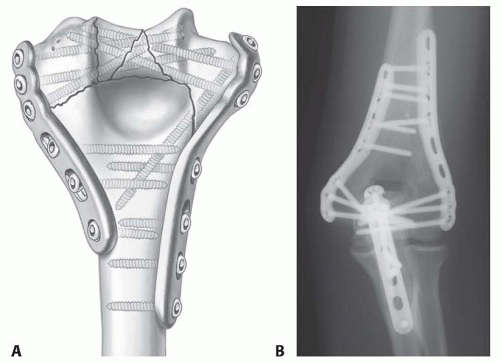
The goal of the internal fixation technique is to achieve a construct stable enough to allow immediate unprotected motion without fear of redisplacement.15,16 This can be attained in most distal humerus fractures—even the most complex—provided the following principles are adhered to the following (FIG 2):
Plates used for internal fixation are applied so that fixation in the distal fragments is maximized.
Distal screw fixation contributes to stability at the supracondylar level, where true interfragmentary compression is achieved.
Approaches
Adequate exposure is necessary to achieve satisfactory reduction and fixation.
The management of the ulnar nerve is controversial; some surgeons favor routine subcutaneous transposition, whereas others prefer to leave the nerve in its anatomic location at the end of the procedure. A number of patients will develop a transitory or permanent ulnar neuropathy, mostly sensitive, regardless of nerve management; preoperative counseling is important in this regard.
Most fractures require mobilization of the extensor mechanism of the elbow through an olecranon osteotomy, triceps reflection, or triceps split.
Simple fractures occasionally may be addressed working on both sides of the triceps without mobilization of the extensor mechanism.
Olecranon osteotomy is the preferred surgical approach for internal fixation for most distal humerus fractures.13
Advantages
Provides excellent exposure
Offers the potential of bone-to-bone healing, thereby limiting the risk of triceps dysfunction
Disadvantages
Complications: nonunion, intra-articular adhesions
Hardware removal may be needed.
Limits the ability for intraoperative conversion to elbow arthroplasty
May devitalize the anconeus muscle
The proximal ulna cannot be used as a template to judge reduction and motion.
Triceps reflection and triceps split9 allow preservation of the intact ulna.
Avoid complications related to olecranon osteotomy.
Facilitate intraoperative conversion to total elbow arthroplasty.
Allow use of the proximal ulna as a template for reduction of the distal humerus articular surface.
Allow assessment of extension deficit after fracture fixation, which is especially useful in fractures requiring metaphyseal shortening.
Bilaterotricipital approach1
Goals and indications
The goal is to provide adequate exposure for fracture fixation without violating the extensor mechanism.
This approach is used only for the more simple fracture patterns (eg, extra-articular or simple intra-articular distal humerus fractures [AO/OTA A, C1, C2]) or when elbow arthroplasty is being considered.
Advantages
This approach avoids complications related to the extensor mechanism.
No postoperative protection is needed.
Surgical time is decreased.
Disadvantage
The procedure provides limited exposure of the articular surface.
TECHNIQUES
▪ Surgical Approach
Olecranon Osteotomy
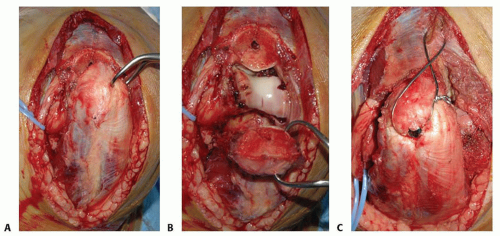
Chevron osteotomy provides increased stability (TECH FIG 1A).
The distal apex of the chevron osteotomy is centered with the bare area of the olecranon articular surface.
The anconeus is divided with electrocautery in line with the lateral limb of the osteotomy.
Alternatively, the anconeus may be preserved by dissecting it free on its distal aspect and reflecting it proximally attached to the proximal ulnar fragment.2
Start the osteotomy with a thin oscillating saw; use of a thick saw blade removes bone excessively, which may make it more difficult to obtain interfragmentary compression at the time of olecranon osteotomy fixation and thus increase the risk of olecranon osteotomy nonunion.
Complete the osteotomy with an osteotome.
Decreases risk of damage to the articular cartilage on ulna and humerus
Creates irregularities at the opposing cut surfaces, which may increase interdigitation
Mobilize the fragment to facilitate exposure (TECH FIG 1B).
Fixation (TECH FIG 1C)
Some biomechanical studies support the combination of a 7.3-mm cancellous screw and tension band over either a screw alone or K-wires plus tension band; others have found no differences.
The author’s preferred method uses K-wires plus a tension band in patients with good bone quality and plate fixation in patients with osteopenia.
If screw fixation is planned, drill and tap the ulna before performing the osteotomy.
Plate fixation provides improved fixation, but the risk of wound complications is increased.
There is substantial interest in the development of intramedullary fixation devices locked proximally and distally; they would combine the benefits of stability and intramedullary location, which could lead to a decreased rate of wound complications and painful hardware requiring removal.
Triceps Reflection and Triceps Split
Bryan-Morrey triceps-sparing approach (TECH FIG 2)
The triceps is elevated from the medial intermuscular septum and the posterior aspect of the humeral shaft.
The forearm fascia and periosteum are incised just lateral to the flexor carpi ulnaris.
The triceps, forearm fascia, and anconeus are elevated in continuity from medial to lateral.
When this approach is used for fracture fixation, the anterior bundle of the medial collateral ligament and the lateral ulnar collateral ligament must be preserved to avoid postoperative instability.
Mayo-modified extensile Kocher approach
The triceps is elevated from the lateral intermuscular septum and the posterior aspect of the humeral shaft.
The triceps and anconeus are elevated in continuity from lateral to medial.
As noted earlier, the anterior bundle of the medial collateral ligament and the lateral ulnar collateral ligament must be preserved to avoid postoperative instability.
Bilaterotricipital Approach
The triceps is elevated from the medial and lateral intermuscular septae.
Lateral dissection can be extended anterior to the anconeus muscle (TECH FIG 3).
The arthrotomy is performed posterior to the medial collateral ligament and lateral collateral ligament complex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree