Open Reduction and Internal Fixation of Scaphoid Fractures
Asheesh Bedi
Peter J.L. Jebson
Levi Hinkelman
DEFINITION
The scaphoid is the most commonly fractured carpal bone, accounting for 1 in every 100,000 emergency department visits.15
Scaphoid fractures typically result from a fall on an outstretched hand or less commonly following forced palmar flexion of the wrist20 or axial loading of the flexed wrist such as in punching.12
Scaphoid nonunion or proximal pole avascular necrosis (AVN) after a fracture has been associated with considerable morbidity and a predictable pattern of wrist arthritis.18,21,25
The complex anatomy and tenuous blood supply to the scaphoid make operative management of these fractures technically challenging.25
ANATOMY
The scaphoid has a complex three-dimensional geometry that has been likened to a “twisted peanut.” It can be divided into three regions: proximal pole, waist, and distal pole.
The scaphoid functions as the primary link between the forearm and the distal carpal row and therefore plays a critical role in maintaining normal carpal kinematics.
Articulating with the scaphoid fossa of the radius, the lunate, capitate, trapezium, and trapezoid, more than 70% of the scaphoid is covered with articular cartilage.
Gelberman and Menon8 have described the vascular supply of the scaphoid. The main arterial supply is from the radial artery; it enters the scaphoid via two main branches:
A dorsal branch, entering through the dorsal ridge, is the primary supply and provides 70% to 80% of the vascularity, including the entire proximal pole via retrograde endosteal branches.
A volar branch, entering through the tubercle, supplies the remaining 20% to 30%, predominantly the distal pole and tuberosity.
The proximal pole is at increased risk for AVN secondary to disruption of its tenuous retrograde blood supply after a fracture of the scaphoid waist or proximal pole.
Due to its tenuous vascular supply, the scaphoid heals almost entirely by primary bone healing, resulting in minimal callus formation.
The size and shape of the scaphoid, in combination with its precarious blood supply, demands attention to detail and accurate implantation of fixation devices during fracture fixation. Scaphoid dimensions vary between genders; the male scaphoid is usually longer and wider than the females. In addition, the diameter of most commercially available standard screws are larger than the proximal pole of the female scaphoid.11
PATHOGENESIS
Scaphoid fractures are most commonly seen in young, active males.15
With the wrist dorsiflexed greater than 95 degrees, in combination with 10 degrees or more of radial deviation, the distal radius abuts the scaphoid and precipitates a fracture.15
The scaphoid can also be fractured with forced palmar flexion of the wrist20 or axial loading of the flexed wrist.12
Most of these fractures occur at the waist region, although 10% to 20% occur in the proximal pole.
Proximal pole fractures are associated with an increased risk of nonunion, delayed union, and AVN.
In children, scaphoid fractures are less common and are most frequently seen in the distal pole.
NATURAL HISTORY
An untreated or inadequately treated scaphoid fracture has a higher likelihood of nonunion. The overall incidence of nonunion is estimated at 5% to 10%, but the risk is significantly increased with nonoperative treatment of a displaced waist or proximal pole fracture.
The natural history of scaphoid nonunions is controversial, but they are believed to result in a predictable pattern of progressive radiocarpal and midcarpal arthritis.8,9,14,17,18,21,25
In an established scaphoid nonunion, the distal portion of the scaphoid may flex, producing a “humpback” deformity of the scaphoid. The loss of scaphoid integrity can result in carpal instability and abnormal carpal kinematics, most frequently manifesting as a dorsal intercalated segment instability (DISI) pattern.
The pattern of carpal instability and secondary arthrosis due to an unstable scaphoid nonunion has been termed an SNAC wrist (scaphoid nonunion advanced collapse pattern of wrist arthritis).14,21
In the SNAC wrist, there is a loss of carpal height with proximal capitate migration, flexion and pronation of the scaphoid, and secondary midcarpal arthritis.21
Factors associated with the development of a scaphoid fracture nonunion include the following17:
PATIENT HISTORY AND PHYSICAL FINDINGS
Scaphoid fractures classically occur in the active, young adult population. Patients present with radial-sided wrist pain.
Classic physical examination findings include the following:
Swelling over the dorsoradial aspect of the wrist
Tenderness to palpation in the “anatomic snuffbox”
Tenderness with palpation volarly over the distal tubercle
Pain with axial compression of the wrist (scaphoid compression test)
Scaphoid fractures can be part of a greater arc injury.
The physician should examine the entire wrist carefully for areas of tenderness and swelling.
Plain radiographs are scrutinized for an associated ligamentous injury or disruption of the midcarpal joint as seen in the transscaphoid perilunate fracture-dislocation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The following plain radiographs should routinely be ordered in the patient with a suspected scaphoid fracture: posteroanterior (PA), oblique, lateral, and dedicated scaphoid views.
The PA view allows visualization of the proximal pole of the scaphoid.
The semipronated oblique view provides the best visualization of the waist and distal pole regions.
The semisupinated oblique view provides the best visualization of the dorsal ridge.
The lateral view permits an assessment of fracture angulation, carpal alignment, and carpal instability.
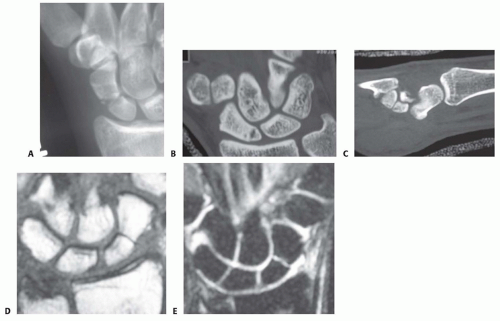
The dedicated scaphoid view is a PA view with the wrist in ulnar deviation. This results in scaphoid extension, allowing visualization of the scaphoid in profile (FIG 1A).
At least 1 mm of displacement
More than 10 degrees of angular displacement
Fracture comminution
Radiolunate angle of more than 15 degrees
Scapholunate angle of more than 60 degrees
Intrascaphoid angle of more than 35 degrees
Computed tomography (CT) with reconstruction images in multiple planes is used to identify an acute fracture not detected on plain radiographs and to determine the amount of displacement and comminution (FIG 1B,C).
CT is most useful in evaluating an established scaphoid nonunion or malunion.6
Because plain radiographs are often unreliable, CT is preferred for confirming union after a scaphoid fracture particularly before permitting a return to contact sports.
Magnetic resonance imaging (MRI) may be indicated in the evaluation of a suspected scaphoid fracture not detected on plain radiographs (FIG 1D,E). MRI is highly sensitive, with
a specificity approaching 100% when performed within 48 hours of injury.16
Bone bruising without a fracture detected on MRI can lead to an occult fracture in 2% of cases.23
MRI with intravenous gadolinium contrast is helpful in assessing the vascularity of the proximal pole, particularly in the patient with an established nonunion.
A technetium bone scan has been shown to be up to 100% sensitive in identifying an occult fracture.27 Unfortunately, it is also associated with a low specificity and often will not be positive immediately after the fracture.
DIFFERENTIAL DIAGNOSIS
Scapholunate injury
Wrist sprain
Wrist contusion
Fracture of other carpal bone
Greater arc injury
Distal radius fracture
NONOPERATIVE MANAGEMENT
Nonoperative management is indicated for a nondisplaced, stable scaphoid waist or distal pole fracture.
The appropriate type and duration of cast immobilization remain controversial and none has proven to be superior. Our preference is a short-arm thumb spica cast until the clinical examination and radiologic studies (usually a CT scan) confirm fracture union. If there are concerns for patient compliance, we prefer an initial period (4 to 6 weeks) of long-arm thumb spica cast immobilization.
Clinical studies have failed to demonstrate any benefit from including the thumb or fingers in the cast.2,4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree