Proximal interphalangeal (PIP) joint fracture-dislocations are intra-articular injuries that include a concomitant soft tissue injury to the surrounding capsular and ligamentous structures.
The injury can result from axial, bending, and torsional loads, or a combined mechanism.
These injuries are relatively common and potentially disabling and may result in the following:
Joint stiffness/swelling
Persistent subluxation
Posttraumatic arthritis
Chronic pain
Stability, a concentric joint reduction and alignment are more important goals than articular congruency in determining a successful outcome.
Evaluation and treatment may be delayed, with the injury dismissed as a “jammed finger.”32
The PIP joint acts as a bicondylar sloppy hinge joint, consisting of radial and ulnar condyles on the proximal phalanx with matching concavities on the middle phalangeal base. This allows for a wide range of motion (ROM) in flexion and extension but relative rigidity in abduction and adduction.19
The PIP joint has an arc of motion of approximately 120 degrees and accounts for 85% of the motion required to grasp an object.2
The heads of the proximal phalanx are trapezoidal in shape tapering toward the ring finger; this allows for a normal finger flexion cascade toward the distal pole of the scaphoid.19
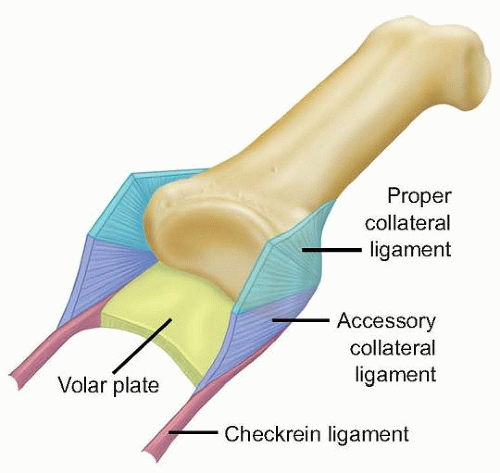
The joint derives its stability from its bony articular congruence and its soft tissue restraints and allows for lateral as well as rotational stability with loading (FIG 1).
The volar plate resists dorsal (hyperextension) stresses, is taut in extension, and most often fails distally.
Checkrein ligaments are slender proximal extensions of the volar plate under which transverse branches of the digital arteries pass supplying the joint, vincula, and the flexor tendons.
Collateral ligaments, the primary soft tissue restraints, have two components:
The proper collateral ligaments (radial and ulnar), which insert on the middle phalanx, provide the principal resistance to abduction/adduction stress. These ligaments are commonly injured in dorsal dislocations. Injury to the radial collateral ligament is more common than injury to the ulnar collateral ligament.
The accessory collateral ligaments arise from a conjoined origin just volar to the proper collateral ligament and insert onto the volar plate.
The extensor complex limits volarly directed stress.
The central slip attaches to the dorsal tubercle on the base of the middle phalanx.
The conjoint lateral tendons run obliquely on each side of the joint.
The transverse retinacular ligament connects the central slip and the conjoint lateral bands and extends laterally.
For a dislocation to occur, at least one, often two, and sometimes all three of these structures must be significantly disrupted.
The PIP joint is uniquely susceptible to injury.
The pattern of joint injury depends on the direction, degree, and rate of force application as well as the position of the joint at the time of injury.
The three main groups of PIP fracture-dislocations are defined by the mechanism of injury force and the direction of deformity (FIG 2).
Dorsal subluxation or dislocation of the middle phalanx, the most common type, is caused by hyperextension and axial loading of the middle phalanx against the head of the proximal phalanx. The result is a fracture involving the volar base of the middle phalanx and dorsal positioning of the middle phalanx.
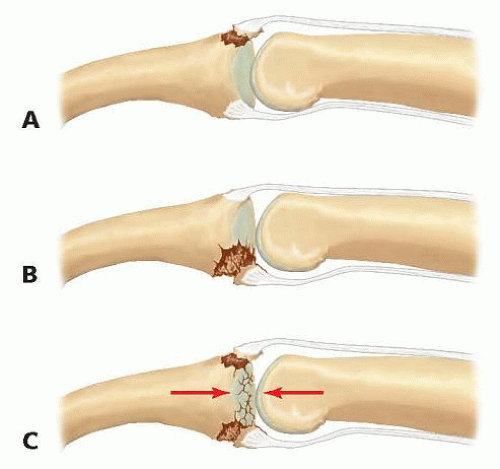
FIG 2 • PIP fracture-dislocation classifications. The three main groups of PIP fracture-dislocations are volar (A), dorsal (B), and pilon (C).
This injury can be subclassified into three types based on the amount of volar middle phalanx articular surface involved, as determined on a lateral radiograph.8,15 The degree of instability is directly proportional to volar lip fragment size due to the loss of collateral ligament support and the articular buttress (see Fig 3B in Chap. 52).17,29,32
Stable: less than 30% of the articular surface, reduced even in extension
Tenuous: 30% to 50% of the articular surface, reduction is maintained with less than 30 degrees of flexion
Unstable: either more than 50% of the articular surface or 30% to 50% of the articular surface but requiring more than 30 degrees of flexion to maintain reduction
Volar subluxation, or dislocation of the middle phalanx, is less common and is thought to be caused by forced flexion of an extended joint.
Stable: joint reduction in extension
Unstable: palmar subluxation of middle phalanx with the joint extended
Pilon injuries are almost always unstable. They are caused by an axial force on a partially flexed PIP joint, resulting in comminution of the articular surface of the middle phalanx (most commonly, volar and dorsal articular fragments surrounding a central depressed fragment).
Unicondylar fractures of the head of the proximal phalanx are included in a classification system proposed by Weiss and Hastings31 (see Chap. 50).
These injuries can also be accompanied by a dislocation of the PIP joint and are nearly always unstable. They often are amenable to the same approaches and fixation methods presented here.
Following injury, the PIP joint quickly stiffens. Pain and instability limit motion initially, followed by fibrosis of the joint capsule and ligaments.
Over time, the unreduced PIP joint will become arthritic and painful.
Patients present following a traumatic event to the digit, frequently one that occurred some time ago.
In the acute setting, the primary complaints are pain and swelling of the joint and digit.
Patients with subacute and chronic injuries are focused primarily on stiffness, loss of function, and persistent swelling, and secondarily on pain.
The history must include a detailed description of the mechanism of injury and any previous treatment.
Inspection
Evaluate the skin and soft tissues for swelling and for any open or healed wounds that could indicate an open fracture-dislocation.
Deformity in extension or flexion indicates whether the dislocation is volar or dorsal, respectively.
Axial or rotational malalignment may result from articular depression of a condyle. This can be recognized clinically as subtle angulation when full digital extension and flexion is attempted.
Tenderness
The location of greatest tenderness on palpation may indicate which soft tissue structures are injured.
ROM
Adequate evaluation may be difficult in the acute setting due to pain. After neurologic examination, a digital block may be necessary.
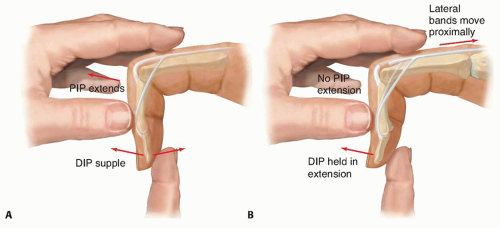
Elson test (FIG 3)
From a 90-degree flexed position over the edge of a table, ask the patient to actively extend the PIP joint of the involved finger against resistance. If the central slip is intact, the examiner will feel an extension force from the middle phalanx. In addition, the distal interphalangeal (DIP) joint remains flail during this effort because the competent central slip prevents the lateral bands from acting distally.
An absence of extension force at the PIP joint and fixed/rigid extension at the DIP joint (due to the extensor action of the lateral bands alone) is diagnostic of a complete rupture of the central slip. In the acute setting, the patient may be reluctant to perform this test due to pain, but this can be relieved by proximal infiltration with local anesthetic around the dorsal sensory nerves of the digit.9
Note the ROM through which the joint remains reduced. In the case of a dorsal dislocation, the degree of extension that results in instability or redislocation determines the angle for the extension block splint.
An irreducible joint is consistent with entrapment of a soft tissue structure (eg, volar plate, collateral ligament, flexor or extensor tendon) in the joint, which usually necessitates surgery.
The neurovascular examination is usually normal.
Subjective complaints of paresthesias and objective measure of capillary refill should be noted, both pre- and postreduction.
Posteroanterior (PA) and lateral radiographs of the involved digit(s) are required.
Partially supinated and pronated oblique views may help to identify fracture planes, determine the extent of comminution, and may be valuable for surgical planning.
It is critical to determine the amount of articular involvement on a true lateral film in full PIP joint extension to evaluate stability of the joint.
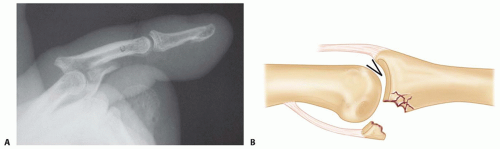
Radiographs can be misleading, suggesting that a very simple fracture involving only a small fragment of the bone has occurred. This fragment is potentially the major attachment of a collateral ligament, the volar plate, or a tendon. The resultant incompetence of these structures can render the joint grossly or potentially unstable (FIG 4A).
On a postreduction true lateral radiograph of the digit, divergence of the dorsal articular surfaces from the central portion of the joint creates a V-shaped gap between the articular surfaces of the head of the proximal phalanx and the undamaged portion of the middle phalanx base.
The presence of this sign indicates an incompletely reduced joint.
Dynamic fluoroscopy is extremely valuable in evaluating the reduction and its stability.
Hinged flexion is a variant of the V sign in which congruent rotation of the joint is replaced by abnormal translation, as the joint is actively flexed and extended across the flattened fracture segments.
The joint position that results in instability or redislocation is best determined fluoroscopically.
Prompt recognition of the complexity of injury and an understanding of the appropriate treatment options are essential for optimal management of these fractures.22
Although fractures and dislocations of the PIP joint have the potential to be disabling, most can be treated with closed reduction, splinting, early motion, and close follow-up.
Closed reduction is almost always successful for acute dorsal PIP dislocations. Volar dislocations are more problematic, especially if the deformity has a rotary component.
Reductions performed immediately after the injury, such as coming to the sideline, often can be accomplished without
anesthesia. If reduction is delayed, a digital block with 1% lidocaine (without epinephrine) is helpful.
Always make sure to complete a careful neurologic examination of the digit before performing an anesthetic block. Confirm adequate anesthesia before manipulation.
Be gentle and limit the number of attempts. Irreducible dislocations usually are caused by soft tissue interposition.
Dorsal dislocations can be reduced with gentle traction on the finger with the wrist in the neutral position, followed by pressing the base of the middle phalanx in a volar direction while holding the proximal phalanx steady.
Volar dislocations without a rotatory component are usually reducible with gentle traction.
Place the wrist in the neutral position, and, with longitudinal traction, apply a dorsally directed force to the middle phalanx and a volarly directed force on the proximal phalanx.
These dislocations, which usually can be treated with closed reduction, commonly involve an avulsion of the central slip.
Volar dislocations with a rotatory component often are difficult to reduce by closed means. The head of the proximal phalanx becomes entrapped between the central slip and one of the lateral bands of the extensor mechanism.
These injuries occasionally can be reduced closed by placing the metacarpophalangeal (MCP) and PIP joints in 90 degrees of flexion with the wrist extended, applying light traction, and rotating the middle phalanx in the direction opposite to the deformity.
Surgical management can be difficult:
The fracture fragments can be small and comminuted, making anatomic reduction and stabilization with implants difficult.
The need for early mobilization of the joint to prevent stiffness requires rigid fixation of these fragments.
These fractures have a high risk of redisplacement, and patients must be warned of the possibility that repeat surgical treatment of the fracture may be necessary.
Table 1 Advantages and Disadvantages of Techniques for Repair of Proximal Interphalangeal Joint Fracture-Dislocation
Technique
Indications
Advantages
Disadvantages
Pearls
ORIF
Minimal comminution
Intact dorsal cortex
Anatomic reduction
Can use bone graft
Early ROM
Technically difficult if multiple fragments
Increased risk of infection
Consider other options in older patients (older than 60 yo), for example, dorsal block pinning.
Volar plate arthroplasty
<50% articular surface involved
Comminution base of P2
Proven track record
Restores volar buttress
Redislocation (especially if >50% P2 base fractured)
Stiffness
Arthritis
Careful patient selection
Osteochondral autograft (ie, hemi-hamate, radial styloid, toes)
Highly unstable dislocations:
>60% of articular surface involvement
Acute or chronic dislocation
Biologic replacement of articular surface
Donor morbidity
Technically demanding
Consider osteochondral autograft if >50% is involved.
Short-term results are promising.
ORIF, open reduction with internal fixation; ROM, range of motion; P2, middle phalanx.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree