Open Reduction and Internal Fixation of Fractures of the Medial Epicondyle
Brian G. Smith
Kristan A. Pierz
DEFINITION
Trauma to the medial aspect of the elbow may cause a medial epicondyle fracture, which is an injury to the apophysis of the medial epicondyle.
ANATOMY
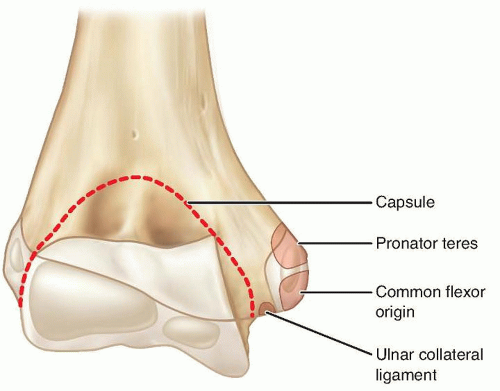
Medial epicondylar fractures involve the medial epicondylar apophysis on the posteromedial aspect of the elbow.
PATHOGENESIS
A direct blow to the medial aspect of the elbow may cause a fracture to the medial epicondyle, but this is rare.
More commonly, a fall on an outstretched arm causes an avulsion of the medical epicondyle via tension generated by stretch of the muscles attaching to it. Elbow dislocation is frequently associated with a medial epicondyle fracture and may occur with spontaneous reduction at the time of the injury (FIG 2).
Considerable force applied to the arm may cause elbow dislocation and associated disruption of the ulnar collateral ligament. This ligament, the principal stabilizing ligament of the elbow, can avulse the medial epicondyle, and the apophyseal fragment may sometimes become lodged in the elbow joint.3
Overuse may cause a chronic stress-type injury or an apophysitis, an example of which would be Little League elbow.
NATURAL HISTORY
The outcome of medial epicondyle fractures is related to the amount of fracture displacement and also the demands placed on the elbow by the patient.
Minimally displaced fractures treated nonoperatively generally do well, especially if the patient is not an athlete or if the fracture involves the patient’s nondominant arm.
Untreated displaced fractures may lead to chronic medial elbow instability and even recurrent elbow dislocations.
Throwing athletes may have significant impairment in their sports activities.9
PATIENT HISTORY AND PHYSICAL FINDINGS
For any elbow injury, the mechanism of injury should be sought, with particular attention to the details of a fall. In children, this may be difficult to elicit, but often, a witness may be available. Medial epicondyle fractures frequently arise from a fall.
The two most important issues in the physical examination are to document neurovascular status and to assess for elbow stability. Determination of stability includes determination of whether the elbow is dislocated, which can be assessed clinically and confirmed radiographically.
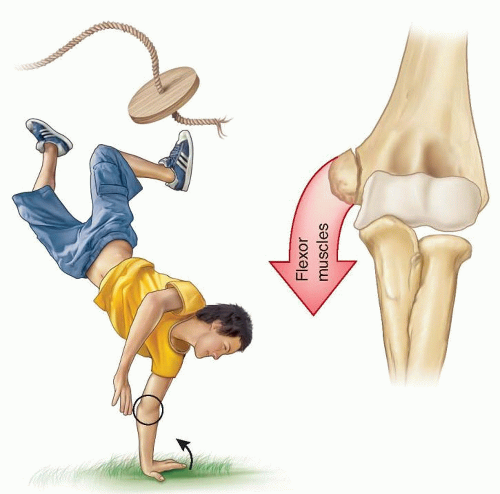
FIG 2 • A common mechanism of injury: a fall on an outstretched arm causing either a “pull-off” or a “push-off” avulsion of the medial epicondyle.
Assessment of medial elbow stability is often important in determining treatment.
A positive valgus stress test confirms medial elbow instability. Persistence of medial elbow instability may cause significant elbow disability in athletes or those doing heavy labor.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard anteroposterior (AP) and lateral radiographs of the elbow are required, but oblique views are often helpful to visualize the medial epicondyle, which is on the posteromedial aspect of the distal humerus.
Widening of the apophysis may be the only sign of injury, so comparison views of the unaffected elbow are often helpful to assess and determine subtle degrees of displacement.
If there is radiographic absence of the medial epicondyle and suspected joint incarceration, an arthrogram, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may occasionally be needed.
DIFFERENTIAL DIAGNOSIS
Medial condylar fractures
Supracondylar fractures
Elbow dislocation
NONOPERATIVE MANAGEMENT
Smith in 1950 became a strong advocate of nonoperative management of this injury, pointing out that the fracture involved an apophysis rather than a physis and thus future growth was not compromised. He also documented that imperfect reduction or even nonunion was not automatically associated with a poor outcome in terms of elbow function and strength.3
A more recent study from Sweden where all patients were treated nonoperatively showed 96% good to excellent results. Over 60% of the patients had a fibrous union or nonunion.3
Two studies have compared nonoperative and operative treatment. Bede and associates1 found that nonoperative treatment had better outcomes than operative treatment.
Farsetti and coworkers5 demonstrated similar results of nonoperative treatment and open reduction and internal fixation (ORIF) with Kirschner wires in displaced fractures.
Indications for nonoperative management of medial epicondyle fractures include patients who do not place high physical demands on their elbows and most nondominant elbows.
Nonoperative treatment encompasses splinting for 5 to 7 days or until acute soft tissue swelling resolves and then early active range of motion starting as soon as possible after the injury.
Physical therapy may be required if range of motion is slow to return, but passive stretch may cause more injury and should be avoided.
SURGICAL MANAGEMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree