Open Reduction and Internal Fixation of Femoral Head Fractures
Darin Friess
Thomas Ellis
DEFINITION
Fractures of the femoral head are rare and occur almost exclusively with associated high-energy hip dislocations, where they may be seen in 5% to 15% of cases.
Associated injuries to the femur, acetabulum, or acetabular labrum can affect treatment options.
ANATOMY
The spherical femoral head is almost completely covered by articular cartilage, which often is damaged during the hip dislocation.
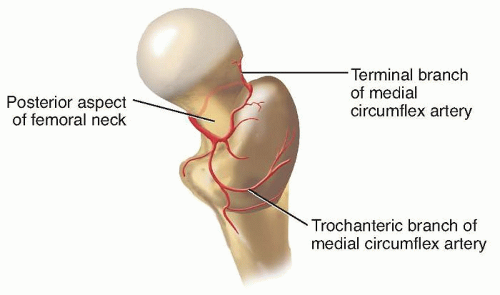
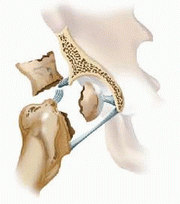
Blood is primarily supplied to the superior dome of the femoral head by the medial femoral circumflex artery, which travels around the posterior aspect of the proximal femur, traveling deep to the quadratus femoris and penetrating the joint capsule just inferior to the piriformis tendon (FIG 1).
Additional vascular support is supplied by the lateral femoral circumflex artery and the foveal artery within the ligamentum teres.
The anterior half of the femoral neck is devoid of vascular structures. Therefore, anterior surgical approaches to the hip joint do not compromise the vascular supply of the femoral head.
The acetabular labrum increases the coverage of the femoral head but may be damaged during hip dislocation.
PATHOGENESIS
The fracture is a shearing injury as the femoral head strikes the acetabular rim. Injury to the articular cartilage of the femoral head is common with femoral head fractures, and posterior wall fractures also can occur with this injury.
Both the position of the leg at the time of impact and the patient’s hip anatomy have been shown to play a role in the etiology of hip fracture-dislocations.
Posterior dislocations, the most common type, occur when the hip is in a flexed, adducted, and internally rotated position.
Decreased femoral anteroversion leads to reduced femoral head coverage by the acetabulum and increases the risk of hip dislocation.
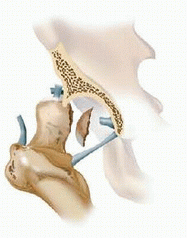
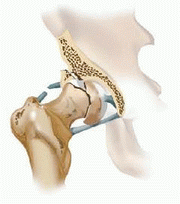
Anterior dislocations are less common. They occur when the hip is in an abducted and externally rotated position, which results in an impaction injury to the anterolateral femoral head (FIG 2).
NATURAL HISTORY
In an intermediate-term follow-up study by Jacob et al,3 despite open or closed treatment, only 40% of patients had satisfactory results after hip dislocation at an average of 4.5 years after injury. More than half of the patients had posttraumatic arthrosis.
Osteonecrosis of the femoral head may develop in 20% of patients with femoral head fractures despite anatomic reduction.
PATIENT HISTORY AND PHYSICAL FINDINGS
Because of the high energy required to induce a fracturedislocation of the hip, all patients should undergo a thorough trauma evaluation for associated injuries.
Airway, cardiovascular, head, and spine injuries should be stabilized emergently.
Narcotic pain medication usually is required.
Careful evaluation of the affected extremity is essential.
The leg often appears shortened and internally rotated after a posterior hip dislocation.
Suspicion for associated injuries, particularly around the knee, should remain high; such injuries can be recognized on physical examination.
Injury to the knee ligaments or extensor mechanism is associated with traumatic hip dislocation and should be assessed with a knee stability examination.
Because sciatic nerve injuries are common, motor and sensory examination of the affected extremity is critical, with particular attention paid to strength grades (1 to 5) and sensation in the peroneal and tibial nerve distribution.
IMAGING AND OTHER DIAGNOSTIC STUDIES
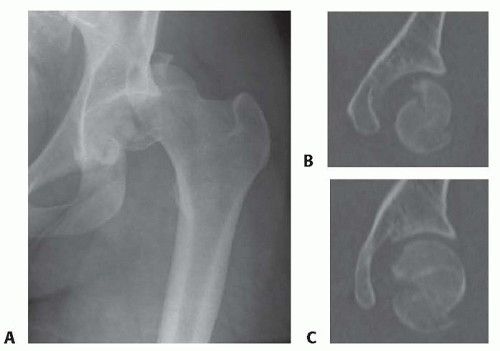
The hip fracture-dislocation is first evaluated on the trauma anteroposterior (AP) pelvis radiograph (FIG 3A). The goal should be to emergently reduce the hip, and further imaging should not excessively delay reduction of the dislocated hip.
Associated injuries such as femoral neck fractures, acetabular fractures, or pelvis fractures may require additional dedicated hip, Judet view, or pelvic inlet and outlet radiographs.
A fine-cut computed tomography (CT) scan of the pelvis and femoral neck with coronal and sagittal reconstructions will further define the anatomy of the femoral head fracture and associated injuries (FIG 3B,C).
This should be obtained after reduction of the hip. A prereduction CT scan of the hip is not typically indicated.
Although magnetic resonance imaging (MRI) can be used to evaluate femoral head osteonecrosis in follow-up care, acute imaging has not been demonstrated to be prognostic of this complication.
DIFFERENTIAL DIAGNOSIS
Femoral head fractures typically are classified according to
Pipkin (Table 1).
An isolated posterior wall fragment may be confused with a femoral head fracture.
Table 1 Pipkin Classification of Femoral Head Fractures | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NONOPERATIVE MANAGEMENT
Surgical management to reconstruct the femoral articular surface usually is indicated.
Nonoperative management is used only in Pipkin type I fractures with small articular fragments with an associated concentric reduction of the hip.
No quality clinical studies are available to define the size of the fragment or amount of displacement that can be tolerated.
The accepted guideline is that the fragment should be congruent with the intact femoral head.
Small impaction injuries associated with anterior dislocation also may be treated nonoperatively in many cases.
Patients managed nonoperatively should remain toe-touch weight bearing for 8 to 12 weeks. For posterior dislocations, hip flexion beyond 90 degrees should be avoided for 6 weeks to protect the posterior capsule.
SURGICAL MANAGEMENT
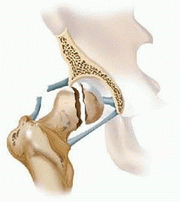
Most patients with femoral head fractures require surgery to provide an anatomic reduction of the femoral head, remove osteochondral loose bodies, or obtain a concentric reduction of the hip joint. Loose body removal can delay the onset of arthrosis.
Large, displaced fragments should be anatomically fixed.
Smaller fragments inferior to the fovea can be excised if a quality, stable reduction of the fracture fragment cannot be obtained.
Although their significance is unknown, labral tears often can be evaluated and treated surgically.
Hip arthroplasty is another good treatment option in elderly patients, especially with large head fragments. Femoral head fractures in this age group tend to have a large amount of articular cartilage damage and impaction of the bone at the fracture line, which compromises the patient’s outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree