Open Reduction and Internal Fixation of Displaced Lateral Condyle Fractures of the Humerus
Kristan A. Pierz
Brian G. Smith
DEFINITION
Lateral condyle fractures refer to fractures of the outer (lateral) aspect of the distal humerus and may involve any or all of the following: metaphysis, physis, epiphysis, and articular surface.
Fractures of the lateral condyle of the distal humerus account for 10% to 15% of all pediatric elbow fractures, second in frequency only to supracondylar distal humerus fractures.6
Nondisplaced fractures may hinge on the articular cartilage, making them more stable than their unstable, displaced counterparts.
ANATOMY
Proximally, lateral condyle fractures almost always include some portion of the posterolateral metaphysis and then propagate along the physis before exiting through or around the ossification center of the capitellum.
The articular cartilage may or may not be violated.
The extensor carpi radialis longus and brevis muscles and lateral collateral ligament typically remain attached to the distal fragment.
Anterior and posterior portions of the elbow joint capsule may be torn if there is significant displacement.
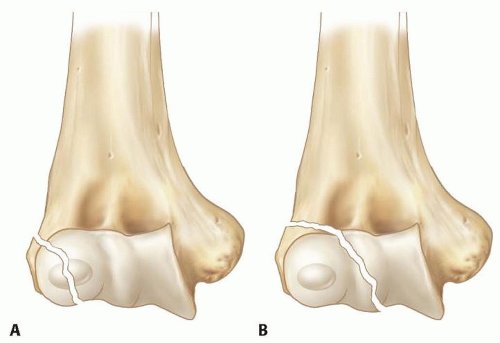
Milch11 classified lateral condyle fractures based on the distal portion of the fracture line (FIG 1).
Milch type I fractures (the less common) traverse the metaphysis and physis as well as extend across the ossification center of the lateral condyle.
Milch type II fractures (the more common) extend from the metaphysis, through the physis, and exit in the unossified trochlea, medial to the capitellum ossification center. Displacement of the trochlear crista allows lateral translation of the forearm and increases the instability of this pattern.
It is difficult to apply the Salter-Harris classification system to lateral condyle fractures because portions of the distal humeral epiphysis may not yet be ossified.
A fracture propagating from the metaphysis through the physis and then through the capitellum ossification center (Milch I) is analogous to a Salter-Harris type IV fracture.
A fracture that extends from the metaphysis through the physis and exits through the unossified trochlea medial to the capitellar ossification center (Milch II) may appear radiographically analogous to a Salter-Harris type II fracture, but its involvement of the articular cartilage is analogous to Salter-Harris types III and IV.
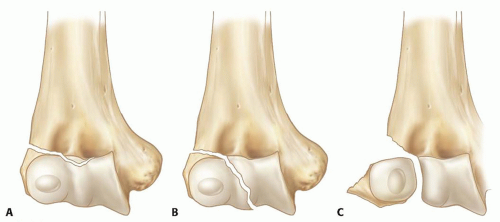
Stage I fractures involve the metaphysis and physis but often do not violate the articular cartilage, thus limiting their ability to displace. Displacement is less than 2 mm.
Stage II fractures cross the articular surface but are minimally displaced. Displacement is 2 to 4 mm.
Stage III fractures are displaced fractures that cross the metaphysis, physis, and articular surface, frequently resulting in rotation of the distal fragment (FIG 2).
PATHOGENESIS
The typical mechanism for a lateral condyle fracture is a fall on an outstretched hand.
Adduction of a supinated forearm with the elbow extended can result in avulsion of the lateral condyle.
Axial load of the forearm combined with valgus force can also propagate a fracture through the lateral condyle.
Lateral condyle fractures usually occur as isolated injuries, although elbow joint subluxation and radial head or olecranon fractures may be associated.
NATURAL HISTORY
The natural history of lateral condyle fractures depends on the fracture displacement as well as the long-term viability of the growing physis.5
Completely nondisplaced lateral condyle fractures may heal regardless of treatment.
Nondisplaced fractures can displace over time if the articular cartilage is violated or if there is significant associated soft tissue injury.
Delayed union can occur even in nondisplaced fractures and may be due to poor metaphyseal circulation, bathing of the
fracture in synovial fluid, or tension on the condylar fragment by attached muscles.
Fractures that heal in near-anatomic alignment can yield excellent functional and cosmetic outcomes.
Lateral condyle fractures associated with lateral physeal arrest can result in valgus deformity and tardy ulnar nerve palsy.
Lateral condyle fractures associated with central physeal arrest can result in a “fishtail” deformity due to continued growth medially and laterally but limited growth in between.
PATIENT HISTORY AND PHYSICAL FINDINGS
Most patients report a fall, either on an outstretched hand or from some height, resulting in pain and inability to fully move the elbow.
It may be difficult to obtain a history from a young child; therefore, parents or caregivers may need to be questioned.
The clinician should be patient during the physical examination. Young children may be very fearful. The clinician should ask the child to point to what hurts most, and this part should be examined last. This allows the clinician to establish the patient’s trust and rule out other associated injuries.
The clinician should look for obvious deformity, swelling, ecchymosis, and open wounds about the elbow.
The clinician should assess for pulses and capillary refill.
Sensation is assessed by comparison with the uninvolved side. Rather than stroking a finger and asking a young child, “Do you feel this?”, the clinician can rub the same site on both hands and ask, “Does it feel the same or different?”
Motor function is assessed by observing for spontaneous movement during the entire encounter. A scared child may refuse to move when asked by a physician but may demonstrate voluntary movement when asked by a parent or sibling. Being playful during the examination can help. For example, when testing for ulnar nerve function, asking a 5-year-old to show you how old he or she is may be more rewarding than asking the child to spread his or her fingers.
The wrist and shoulder are palpated before touching the elbow.
A single finger is used to gently palpate the olecranon, medial epicondyle, posterior humerus, lateral condyle, and radial head to try to localize the specific site of injury. Crepitus suggests displacement and instability of the fracture fragment.
Increased motion during varus stress testing suggests instability of the fracture. Due to pain, however, this test can rarely be done on an awake child. It is often reserved for intraoperative assessment rather than preoperative diagnosis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
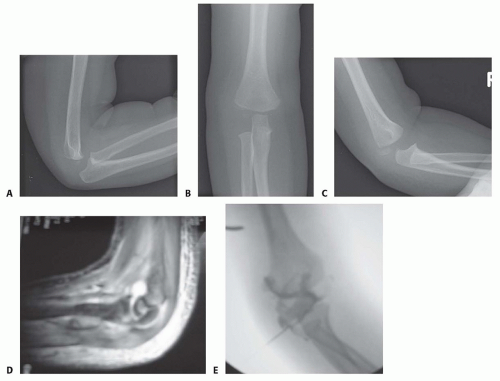
Radiographs of a suspected lateral condyle fracture should include anteroposterior (AP), lateral, and internal oblique views (FIG 3A-C).
Valgus and varus stress radiographs can provide information about the stability of the fracture. Because such films are poorly tolerated in an awake child, they are rarely obtained outside of the operating room.
For nondisplaced or minimally displaced fractures, magnetic resonance imaging (MRI) can be used to determine whether the articular surface is violated7 (FIG 3D).
Such studies, however, are expensive, are rarely needed for surgical decision making, and frequently require sedation in young children, so they are not obtained routinely.
DIFFERENTIAL DIAGNOSIS
Contusion
Lateral collateral ligament strain or sprain
Radial head or neck fracture
Supracondylar distal humerus fracture
Transphyseal fractures
Medial condyle fractures
Proximal ulnar or Monteggia fractures
Elbow dislocation
Child abuse
NONOPERATIVE MANAGEMENT
Nonoperative management of lateral condyle fractures is typically reserved for nondisplaced or minimally displaced (<2 mm) fractures.
The upper extremity is immobilized in a long-arm splint or cast with the elbow flexed 90 degrees and the forearm in neutral.
Casts that are excessively heavy or short on the upper arm tend to slide down, thus increasing the risk of later displacement.
Follow-up radiographs should be obtained in 3 to 5 days to assess for further displacement.
If displacement occurs, operative treatment is indicated.
If the fracture remains nondisplaced, long-arm casting is continued for another week, and then repeat radiographs are obtained.
If still nondisplaced, the fracture is maintained in a long-arm cast until there is radiographic evidence of fracture union, typically at 4 to 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree