Open Reduction and Internal Fixation and Closed Reduction and Percutaneous Fixation of Femoral Neck Fractures
Brian Mullis
Jeff Anglen
DEFINITION
Femoral neck fractures occur in two patient populations.
Most commonly, they happen in older osteopenic patients after low-energy trauma, such as falls.
When they occur in younger patients with normal bone, they are usually the result of high-energy trauma, such as a motor vehicle collision.
Femoral neck fractures can be classified by several characteristics. The most important distinguishing feature in regard to treatment decisions is the degree of displacement.
Fractures that are nondisplaced or impacted into valgus can usually be treated with fixation in situ using percutaneous methods.
Displaced fractures usually require reduction and fixation or replacement.
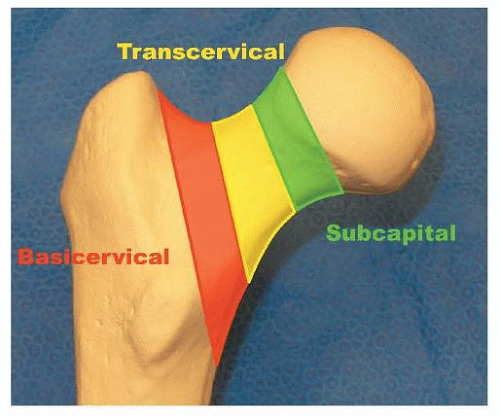
The location of the fracture in the femoral neck can be described as subcapital, transcervical, or basicervical (FIG 1).
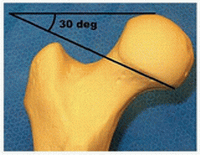
Transcervical femoral neck fractures can be further characterized by the angle of the fracture line with respect to the perpendicular of the femoral shaft axis. This is the Pauwels classification (Table 1).
The importance of this feature is to recognize highangle fractures (more vertical), which have the greater risk of displacement when treated with screws along the neck axis.
ANATOMY
The femoral neck axis forms an angle of about 140 degrees to the femoral shaft axis. In addition, it is anteverted about
15 degrees with reference to the plane of the posterior condyles of the distal femur.
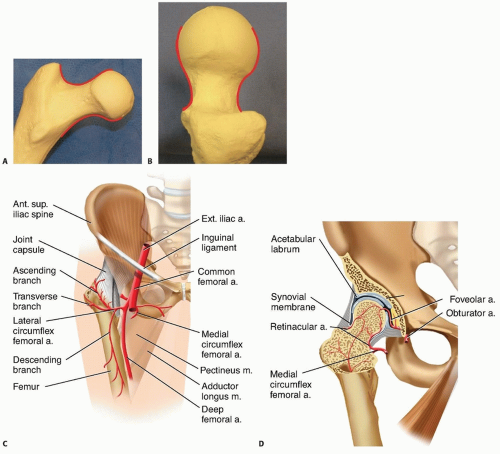
When viewed in both anteroposterior (AP) and lateral radiographic views, the normal contour of the femoral head and neck forms a gentle S (FIG 2A,B).
The vascular supply of the proximal femur relies on the medial femoral circumflex artery, particularly the posterior branch, which feeds the retinacula of Weitbrecht. Minor contributions come from the artery of the ligamentum teres (FIG 2C,D).
PATHOGENESIS
Low-energy femoral neck fractures generally are a result of a fall from standing height in an osteoporotic individual.
This is an increasing public health problem, with projections of 512,000 total hip fractures in the United States by the year 2040.1
High-energy (comminuted) femoral neck fractures generally result from high-speed motor vehicle collision or falls from greater than 10 feet.
These patients frequently have multiple injuries, which can complicate treatment.
NATURAL HISTORY
Nondisplaced or minimally displaced fractures that are not surgically stabilized are likely to suffer worsened displacement owing to the high mechanical forces associated with hip motion and the instability that comes from comminution of the cortical bone.
The intra-articular location of the femoral neck means that there is not a well-vascularized soft tissue envelope, and the fracture is exposed to synovial fluid, which contains enzymes that lyse blood clot, the required first stage in bone healing. As a result, femoral neck fracture healing is slowed.
In addition, the blood supply comes from tenuous retrograde blood flow.
Nonunion rate for untreated displaced fractures approaches 100%.
Nonunion of the femoral neck leads to a shortened limb, variable restriction in motion, and pain with weight bearing.
Table 1 Pauwels Classification of Transcervical Femoral Neck Fractures
Classification
Fracture Plane Angle*
Example
Effect of Vertical Forces on Fracture Site
Fixation
Pauwels 1
Low, ≤30 degrees
Compression, stable
Lag screws in axis of femoral neck
Pauwels 2
30-50 degrees
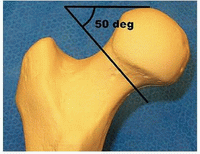
Variable
Lag screws in axis of femoral neck
Pauwels 3
High, ≥50 degrees
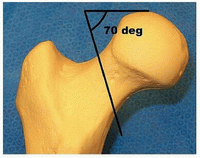
Shear, unstable; tends to displace into shortened, varus position
At least one lag screw perpendicular to fracture plane
* Fracture plane angle is relative to a line perpendicular to the femoral axis on AP radiograph.
Fracture of the femoral neck can lead to interruption of the blood supply to the femoral head due to kinking or disruption of vessels or tamponade from hemarthrosis.
This results in avascular necrosis in about 15% of cases.2
Many surgeons believe that time to treatment is an important factor, with delay increasing the incidence. This is difficult to prove, and the time imperative probably varies from patient to patient.
Femoral neck fractures in the elderly are associated with about 20% 1-year mortality.4
About 50% of patients return to their previous level of function after surgery.3
PATIENT HISTORY AND PHYSICAL FINDINGS
In most patients with femoral neck fracture, the history will contain a distinct traumatic episode, after which the patient could not ambulate.
Physical findings reveal limb shortening, external rotation, and pain on attempted hip motion.
In some patients, the onset of pain is more insidious.
It is usually associated with weight bearing, and it is located in the groin rather than in the buttock or trochanteric area.
In the case of a stress fracture, the history of increased activity over a short period of time is suggestive.
Night or rest pain suggests pathologic fracture or impending fracture.
In highly osteoporotic patients with minor trauma, a history of groin pain with weight bearing may be a symptom of occult femoral neck fracture, which is a nondisplaced fracture not visible on plain radiographs.
Physical examination should include the following:
Observation of the lower extremities with comparison of foot position in the supine patient. A shortened, externally rotated limb indicates fracture.
Gait observation. Groin pain on attempted weight bearing or an antalgic gait suggests occult femoral neck fracture.
Internal and external rotation. Pain in the groin is concerning for femoral neck fracture but may also be caused by fractures of the anterior pelvic ring.
Impaction of the heel of the injured leg. Groin pain that did not exist at rest implies hip fracture.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard plain radiographs consist of an AP view of the pelvis and AP and frog-leg lateral films of the hip.
An AP traction film with internal rotation can be helpful if initial films are difficult to interpret in terms of the location of injury or fracture pattern.
If clinical suspicion is high (eg, an elderly patient who cannot ambulate because of groin pain) but plain radiographs are negative, a bone scan or magnetic resonance imaging (MRI) may be obtained for low-energy injuries.
The bone scan will not turn positive for 24 to 72 hours, but the MRI should be diagnostic within hours of injury.
Some studies have suggested that any multiply injured patient with a high-energy femur fracture should have imaging of the femoral neck with a CT scan in addition to plain films to identify minimally displaced femoral neck fractures. However, the CT scan may be false negative as well, and the routine use of this modality is controversial.
DIFFERENTIAL DIAGNOSIS
Intertrochanteric, pertrochanteric, or subtrochanteric fracture
Anterior pelvic ring (ramus) fracture
Hip dislocation
Femoral head fracture
Pathologic lesion, including neoplasm or infection
Arthritis
Avascular necrosis
Contusion
Muscle strain
NONOPERATIVE MANAGEMENT
Nonoperative treatment may be appropriate in patients who are nonambulators, neurologically impaired, moribund, or in extremis.
Nonoperative treatment should initially consist of bed rest, appropriate analgesia, protection against decubitus ulcers, and appropriate medical supportive treatment.
Buck traction or pillow splints may be helpful in reducing pain.
Some valgus impacted fractures may be treated nonoperatively, particularly if discovered after several weeks, but there is a risk of displacement of up to 46%.
Nonoperative treatment for these patients should consist of mobilization on crutches or a walker.5
Stress fractures may be treated nonoperatively if they are caught early and are nondisplaced and if the fracture line does not extend to the tension side or superior neck.
SURGICAL MANAGEMENT
Most patients with femoral neck fracture should be considered for surgical treatment.
Displaced femoral neck fractures in some patient populations may be better served by hemiarthroplasty or total hip arthroplasty, which is beyond the scope of this chapter.
This includes elderly patients, osteoporotic patients, those with neurologic disease, patients with preexisting hip arthritis, and those with medical illnesses impairing bone healing or longevity (eg, renal failure, diabetes, malignancy, or anticonvulsant treatment).
Nondisplaced fractures, valgus impacted femoral neck fractures in the elderly, or stress fractures in athletes can be treated with fixation in situ through percutaneous techniques.
Open reduction and internal fixation is the standard for highenergy injuries in younger healthy patients with good bone.
Closed reduction of a displaced femoral neck fracture in the young patient is difficult, and one should not accept a lessthan-perfect reduction to avoid an open procedure.
The quality of the reduction is the most important surgeoncontrolled factor in outcome.
Preoperative Planning
Once the decision for operative treatment is made, preoperative planning begins with evaluation of patient-specific factors that may alter the timing or technique for fixation of the femoral neck fracture.
In the elderly population, optimization of medical conditions is advisable, including evaluation of hydration and cardiac and pulmonary function and management of chronic medical conditions. However, delay of surgery beyond the first 2 to 4 days increases the risk of perioperative complications and the length of stay.
In younger patients, it is important to consider other injuries that may affect operative positioning or fixation. For example, ipsilateral lower extremity injuries at another level may affect the use of the fracture table.
Good-quality radiographs in two planes are necessary to understand the location and orientation of the fracture. In some cases, radiographs of the contralateral side may help select an implant with the correct length, diameter, or neck-shaft angle.
The anticipated implants should be verified present before the case. It is useful to have arthroplasty instruments and implants in the hospital in the event of unexpected findings. Fortunately, this will rarely be needed.
Nondisplaced fractures in the subcapital or transcervical region can be treated with two or three cannulated screws, but most surgeons believe that basicervical fractures should be treated with a fixed-angle device, such as a sliding hip screw or cephalomedullary nail.
Positioning
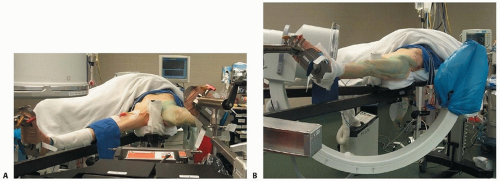
The patient is positioned on a fracture table with both hips extended. The contralateral leg is abducted to allow the C-arm to be positioned between the legs (FIG 3A).
Owing to the risk of compartment syndrome, the surgeon should avoid using the “well-leg holder,” which puts the contralateral leg in a hemilithotomy position (hip and knee flexed, elevating the leg).
Intraoperative fluoroscopy is used, and good visualization of the hip and the fracture reduction in both AP and lateral projections should be verified before preparing the leg (FIG 3B).
A closed reduction may sometimes be obtained by applying gentle traction and internal rotation under fluoroscopic control (see FIG 3A). Vigorous and complicated reduction maneuvers are unlikely to be effective and should be avoided. If simple,
gentle positioning is not successful in achieving acceptable position, open reduction should be strongly considered. The patient should be well relaxed by the anesthesia team.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree