Open Lengthening of the Achilles Tendon
Anna V. Cuomo
Norman Y. Otsuka
Richard E. Bowen
DEFINITION
Shortening of the Achilles tendon, gastrocsoleus complex (triceps surae), or both results in an equinus (plantarflexed) position of the calcaneus relative to the tibia.
An equinus deformity is either congenital or acquired and can be dynamic or rigid.
A dynamic deformity will correct with passive manipulation.
A rigid, or fixed, deformity does not correct.
Achilles or gastrocsoleus contracture often occurs in combination with other soft tissue contractures.
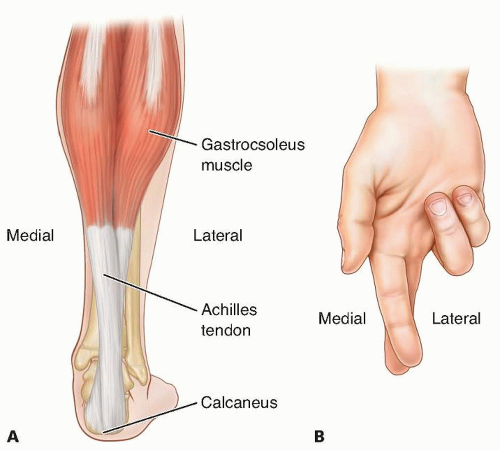
ANATOMY
The two heads of the gastrocnemius originate on the posterior aspect of the medial and lateral condyles of the distal femur.
The muscle fibers terminate at the muscle-tendon junction at the midcalf.
From here, the Achilles tendon is joined by tendon fibers from the posterior aspect of the soleus as the tendon courses distally.
The tendon is broad proximally and then becomes rounded at the midsection when it undergoes a 90-degree internal rotation before its insertion on the posterosuperior third of the calcaneus.
The rotation causes the medial fibers of the midtendon to insert on the posterior portion of the calcaneus (FIG 1).
The insertion footprint is delta-shaped, and a small portion of the fibers course distally to meet the origin of the plantar fascia.
The blood supply of the Achilles tendon is limited.
The proximal portion is supplied by branches from within the gastrocnemius muscle.
The distal portion is supplied by branches from the tendon-bone interface.
There is no true synovial sheath. Instead, the surrounding paratenon, comprising loose connective tissue, supplies the rest of the blood supply via branches from the posterior tibial artery and, to a lesser degree, the peroneal artery.2
There are two synovial bursae at the Achilles tendon insertion site.
One is subcutaneous, located between the skin and tendon, and the other is deep, located between the tendon and the calcaneus.
PATHOGENESIS
The pathogenesis of congenital equinus is poorly understood and it is often associated with other limb deformities such as clubfoot or congenital vertical talus.
Acquired equinus deformity secondary to cerebral palsy results from muscle spasticity or imbalance, leading to subsequent contracture of the Achilles tendon and gastrocsoleus complex.
Muscle imbalance and spasticity in spastic diplegic cerebral palsy often results in equinoplanovalgus deformity.
Muscle imbalance and spasticity in spastic hemiplegic cerebral palsy often results in equinus or equinovarus deformity.
Compensatory balance mechanisms to help maintain ambulation in patients with Duchenne muscular dystrophy also may result in equinus deformity.
Posttraumatic equinus can also be a result of severe burns and posterior scar contracture, postburn positioning, anterior leg muscle loss, or continued tibial growth in a rigid scar.3
Talocrural and subtalar capsular adhesions and an abnormal tibiotalar articulation may also contribute to loss of dorsiflexion and equinus deformity.7
NATURAL HISTORY
Fixed equinus deformity will not correct spontaneously and requires prescribed stretching, surgical intervention, or both.4
Equinus associated with cerebral palsy is progressive. Despite both conservative and surgical treatments, the deformity can recur due to persistent spasticity, muscle imbalance, or limb growth.
Equinus deformity results in abnormal gait because of altered ankle range of motion and decreased ankle plantarflexion
moment during terminal stance. It can result in chronic pain, poorly fitting footwear, callosities on the plantar forefoot, and possible skin ulceration in patients with altered sensation.
PATIENT HISTORY AND PHYSICAL FINDINGS
Birth history may reveal gestational or perinatal complications, such as traumatic brain injury or global hypoxic events, which are risk factors for cerebral palsy.
Family history may reveal a heritable neuromuscular disease or idiopathic toe walking.
A delay in gross motor milestones may suggest the presence of a static neurologic disorder such as cerebral palsy, whereas regression of gross motor function may suggest a progressive neuromuscular disease such as muscular dystrophy or Rett syndrome.
The age of equinus deformity onset will depend on the type and severity of the underlying condition.
Posttraumatic equinus, particularly a burn, should prompt questions regarding severity of the soft tissue loss, type of treatment, period of immobilization, and current problems with skin ulceration to assess the severity of scarring and overlying skin quality. Electrical burns can have extensive internal scarring well beyond the involvement of the overlying skin.
Physical examination should include a thorough examination of the entire lower extremities to look for associated deformities at the hip, knee, hindfoot, and forefoot.
The patient is examined supine on the examination table. It is important that the table has a hard surface so as not to mask any other contractures. The alignment and passive range of motion of the lumbosacral spine, pelvis, hips, and knees must also be tested because equinus may be a functional compensation for coexistent contractures.9
Ankle range of motion: Absence of dorsiflexion beyond neutral is ankle equinus.
Silfverskiöld test: A positive test indicates isolated gastrocnemius contracture. This is present if ankle equinus is present with the knee extended but improves with knee flexion.
Palpation of Achilles tendon: A tight tendon suggests spasticity of the gastrocsoleus complex or contracture of the Achilles tendon. Absence of a taut Achilles tendon with maximum dorsiflexion suggests tibiotalar joint deformity or a contracted posterior tibiotalar capsule.
Palpation of posterior tibial and peroneal tendons: Taut tendons suggest additional contracture or spasticity of the involved musculotendinous units contributing to the ankle equinus contracture.
Ankle clonus: More than two beats of clonus is abnormal and indicates gastrocsoleus spasticity or an upper motor neuron lesion.
Examination of the forefoot is important because isolated severe forefoot equinus may give a clinical appearance of hindfoot equinus. Lateral foot standing radiographs may be indicated if the physical examination is not clear. This is a common finding in the hereditary motor and sensory neuropathies.
If the child is ambulatory, the clinician should observe the gait in a hallway or large area where the patient can both walk and run.
Socks, shoes, and clothing that extend below the knee are removed.
Hindfoot alignment is best observed from behind.
The foot progression angle (axis of the foot to the axis of progression) and any associated coronal plane abnormalities, such as scissoring (excessive hip adduction during gait), knee progression angle, and pelvic rotation, are best observed from the front.
Ankle equinus and any associated sagittal plane abnormalities, such as a crouch gait (hip and/or knee flexion contracture) or a stiff-knee gait (decreased knee range of motion during swing phase), are best observed from the side.
In mild equinus, the normal heel-to-toe gait of the plantargrade foot will be replaced with early lift-off during stance. Subtle deformity in patients with cerebral palsy is often unmasked by asking the patient to run. In severe equinus, the heel will not make contact during heel strike.
Equinovarus or equinoplanovalgus deformity will cause initial contact during gait to occur on either the lateral or medial border of the foot, respectively. There may be a callus or foot pain at the area of initial contact.
Associated muscle spasticity or contracture in cerebral palsy should be diagnosed with the appropriate physical examination maneuvers described in the relevant chapters.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP) and lateral weight-bearing radiographs of the affected ankle should be obtained.
Ossification centers of the talus, calcaneus, and cuboid are present at infancy. The navicular does not appear until age 3 to 4 years.
Equinus deformity will result in a decreased lateral tibiocal-caneal angle. Normal values range from 25 to 60 degrees. It can be difficult to measure this angle in young children with a partially ossified calcaneus.
Although usually associated with hindfoot varus, equinus deformity can also result in a decreased lateral talocalcaneal angle (intersection of a line through the longitudinal axis of the talus and a line along the plantar surface of the calcaneus; FIG 2). The normal range is 25 to 55 degrees.
Bony abnormalities, such as a flattened talar dome or anterior talar neck and anterior distal tibial osteophytes, can also contribute to ankle equinus.
DIFFERENTIAL DIAGNOSIS
Congenital equinus
Talipes equinovarus (clubfoot)
Planovalgus
Congenital vertical talus
Arthrogryposis
Tibial longitudinal deficiency
Acquired equinus
Neuromuscular
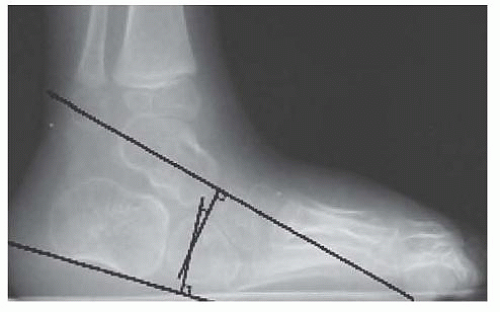
FIG 2 • Measurement of the lateral talocalcaneal angle. The normal range of 25 to 55 degrees is decreased in equinus.
Cerebral palsy
Myelomeningocele
Hereditary motor and sensory neuropathies
Spinal muscular atrophy
Sacral agenesis
Rett syndrome or other genetic neuromuscular diseases
Posttraumatic
Posterior scar contracture
Posttrauma positioning
Anterior leg muscle loss
Continued tibial growth in a rigid scar
Other
Idiopathic toe walking
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree