Open and Arthroscopic Radial Styloidectomy
Bruce A. Monaghan
DEFINITION
Arthritis between the radial styloid and the distal aspect of the scaphoid can lead to pain, weakness of grip, and limitation of motion. This arthritis can occur in the early stages of a variety of pathologic states of the radiocarpal joint.
Radial styloidectomy is a technique that involves resection of the distalmost aspect of the articular surface of the distal radius.
A radial styloidectomy can be performed as a distinct procedure via an open incision or by arthroscopic means. It is more commonly undertaken as an adjunct procedure with reconstructive or salvage procedures for scaphoid nonunions, carpal instabilities, Kienböck disease, or posttraumatic arthritis of the radiocarpal joint.10,22
ANATOMY
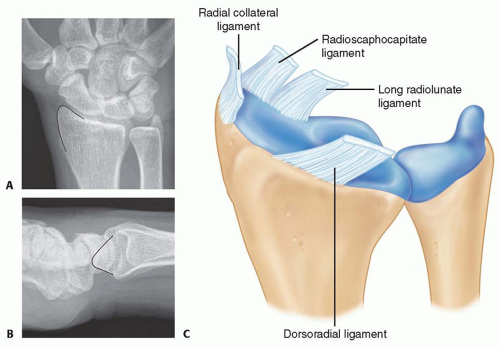
The radial styloid is the distalmost projection on the lateral aspect of the terminal end of the radius (FIG 1A,B).
When viewed from the lateral aspect, the styloid has a gentle slope volarly, placing it below the midcoronal longitudinal axis of the radius.
The intra-articular component of the radial styloid encompasses part of the scaphoid facet.
The extra-articular aspect of the styloid serves as the origin of several dorsal, palmar, and radial extrinsic ligaments that are vital to normal carpal kinematics (FIG 1C).
The palmar radiocarpal ligaments serve as a constraint to radiocarpal pronation, ulnar translation, and distal pole scaphoid stabilization. Global disruption of this complex has been implicated in perilunate dislocation. The palmar radiocarpal ligaments are composed of the following structures:
The radial collateral ligament (RCL) is a thin structure that originates from the tip of the radial styloid and inserts into the waist and distal aspect of the scaphoid. The integrity of the ligament is always sacrificed with a radial styloidectomy, but no untoward effects have been reported.3,4
The radioscaphocapitate (RSC) ligament originates from the palmar cortex of the distal radius coursing distally and ulnarly, attaching to the waist and proximal cortex of the distal pole of the scaphoid and the body of the capitate.3,4
The dorsal radiocarpal (DRC) ligament originates broadly from the dorsal rim of the distal radius around the tubercle of Lister, coursing ulnarly, distally, and obliquely to insert on the dorsal tubercle of the triquetrum.
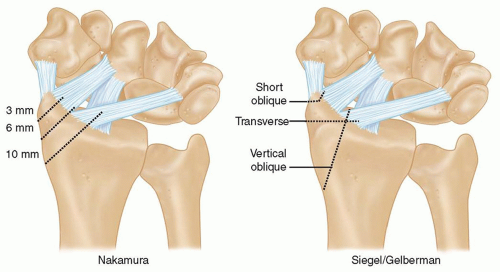
Siegel and Gelberman16 examined the effect of three different styloidectomy configurations on palmar radiocarpal ligament integrity in a cadaver model (FIG 2).
The most conservative osteotomy (short oblique) removed only 9% of the RSC and none of the LRL ligaments.
A vertical oblique osteotomy sacrificed 92% of the RSC and 21% of the LRL ligaments.
A transverse styloidectomy was the most aggressive and resulted in loss of 95% of the RSC and 42% loss of the LRL ligaments.
Nakamura et al12 examined the effect of radial styloidectomy on carpal alignment and ulnar translation in cadaveric limbs. They demonstrated that as a larger segment of the radial styloid was resected (see FIG 2), a greater tendency toward ulnar translation, as manifested by decreased stiffness, was observed. No frank ulnar translation with axial loading was observed.
Based on their analysis, they recommended that no more than 3 to 4 mm of radial styloid should be resected. This correlated with a short oblique styloidectomy as described by Siegel and Gelberman.16
Although ulnar translation is a stated complication of overly vigorous styloidectomy, Viegas et al19 demonstrated in a cadaver model that ulnar translation can occur only with resection of the DRC, RSC, LRL, and short radiolunate (SRL) ligaments.
PATHOGENESIS AND NATURAL HISTORY
Scapholunate Instability
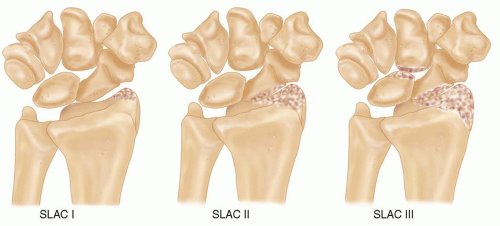
Watson and Ballet21 reviewed radiographs of individuals with scapholunate dissociation to establish the sequential progression of arthritis in the scapholunate advanced collapse (SLAC) wrist (FIG 3).
SLAC I: Degenerative changes are confined to the radial styloid area.
SLAC II: Changes are characterized by joint space narrowing involving the entire radioscaphoid articulation.
SLAC III: Changes involve additional arthritis between the capitate and lunate.
Several authors have examined the mechanics of scapholunate dissociation in cadaver models and have demonstrated that scapholunate instability leads to a shift in the contact pressures from the proximal pole of scaphoid articulation with the radial articular surface toward the distal pole of the scaphoid with the dorsal lip of the radial styloid.7,8 The pathomechanics of these changes can occur even before the frank radiographic appearance of scapholunate diastasis is present (ie, static scapholunate instability). Prolonged exposure to these abnormal contact stresses leads to the predictable arthritic changes described earlier.
Scaphoid nonunion
With an unstable scaphoid fracture, the proximal pole of the scaphoid remains firmly fixed to and extends with the lunate through an intact scapholunate interosseous ligament. The distal pole adopts a flexed posture, which can then impinge on the radial styloid, leading to abnormal contact stresses and arthritic changes.
The natural history of scaphoid nonunion has not been established by rigorous prospective analysis. Nonetheless, most surgeons believe that unstable scaphoid fractures result in abnormal carpal kinematics with a dorsal intercalated segment instability (DISI) deformity and subsequent arthritis (scaphoid nonunion advanced collapse [SNAC] wrist).
Vender et al18 examined the radiographs of 64 patients with symptomatic scaphoid nonunions and showed a high frequency of degenerative changes that occurred in a predictable sequence similar to the findings of SLAC wrist. Initial degenerative changes were seen between the radial styloid and the distal fragment of the scaphoid nonunion. Changes then progressed to include the midcarpal joint with sparing of the proximal pole scaphoid and radiolunate articulation.18 Inoue and Sakuma9 reviewed 102 patients with scaphoid nonunions clinically and radiographically; they found that arthritis initially developed at the scaphoid-radial styloid articulation and subsequently the midcarpal joint. All patients had radiographic arthritis within 10 years of injury. They also demonstrated that although radiographic progression did not correlate with wrist pain, it did correlate with a decrease in grip strength and range of motion.
Impingement after triscaphe (scaphoid-trapezoid-trapezium) fusion
Rogers and Watson14 reviewed 93 patients after triscaphe fusion and found a 33% incidence of painful impingement between the fusion mass and the radial styloid that resolved after limited radial styloidectomy. They hypothesized that the fixed scaphoid could no longer be accommodated in the fossa and impacted on the radial styloid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree