Revision of Failed Ankle Implants
Keywords
• Total ankle joint replacement • Ankle joint arthrodesis • Degeneration • Arthritis
Introduction
Total ankle joint replacement (TAR) has been offered as an alternative to ankle joint arthrodesis since the 1970s. Historically, ankle arthrodesis has been viewed as the gold standard of treatment of end-stage arthritis, because it offers reliable reduction of pain with good functional outcomes.1 However, as with any surgical endeavor there are complications, including nonunion, malalignment, and gait alterations. These issues, in addition to a tenuous postoperative course, may decrease patient satisfaction and functional outcomes. In addition, degeneration of joints adjacent to the ankle, specifically the subtalar joint, is a concern and may predispose the joints to arthritis after ankle arthrodesis has been performed.2
Alternately, TAR offers the benefit of perseveration of joint motion, with potential decreased occurrence of adjacent joint degeneration, and a more expedient path to weight bearing. Studies have demonstrated inherently better patient outcomes with ankle arthroplasties, when performed with the second-generation implants.2,3
Since their introduction, TAR devices have undergone a variety of modifications, specifically in regards to the number and type of components used. These modifications have been necessary because previous success rates of TAR long-term outcomes did not equivocate with those of total knee and hip replacements.4,5 The reasoning behind this trend is thought to be multifactorial. It may be because a high proportion of patients suffering from degeneration of the ankle joint are often younger, more active patients who have likely suffered a traumatic injury.6 Generally, lower patient outcome scores have been related to younger populations, whereas higher rated outcomes are seen with older patients who have a smaller body mass index.7
Overview of TAR and systems
Indications for TAR include posttraumatic osteoarthritis, systemic arthritis, primary arthritis, or revision from prior ankle arthrodesis.3
The early implant models were cemented, and constructed of two components, which were described as constrained, semiconstrained, or nonconstrained.8 These early models proved to be unstable when applied, leading to high rates of failure and disappointing long-term results.9,10
The initial models were followed by a generation of three-component models that had a central component that allowed multiaxial motion of the joint.8 The models used currently are typically cementless, with a mobile-bearing polyethylene component. Each of the available models varies in structure and composition. The Salto (Tornier SA, St. Ismier, France) device is composed of cobalt-chrome alloy, followed by a layer of pure titanium and calcium hydroxyapatite.11 This hydroxyapatite layer is intended to decrease the occurrence of radiolucency surrounding the implant. Another commonly used implant device is the Agility Total Ankle System (DePuy, Warsaw, IN).3 This product has two components, which are composed of titanium and cobalt-chromium, and is semiconstrained. Bone ingrowth is a key factor for secure implantation of this device because cement is not used for application.3 In addition, this implant partially relies on fusion of the distal tibiofibular syndesmosis for added stability.12
The Scandinavian Total Ankle Replacement (STAR) has three uncemented components, and is considered to be a mobile-bearing unit. The tibial and talar components are composed of cobalt-chrome, with a double coat of titanium and calcium phosphate. The third piece is ultra-high molecular weight polyethylene.9
Another implant device is the AES (Ankle Evolution System, Biomet, Nimes, France). This is an uncemented, three-component, meniscal-bearing unit, offering a triangular-shaped tibial stem, which offers increased stability.13
Preoperative planning to prevent failure of TAR is a key component for positive outcomes. Chances for postoperative lack of range of motion, implant instability, and lack of fusion of the tibiofibular syndesmosis may be avoided with thorough preoperative evaluation of the mechanical axis of the causing deformity.12 Furthermore, realistic expectations regarding outcomes after the procedure must be conveyed to the patient. Specifically, a decrease in the amount of ankle joint range of motion as compared with a normal joint is likely to be expected and has been documented.14
Mechanisms of failure
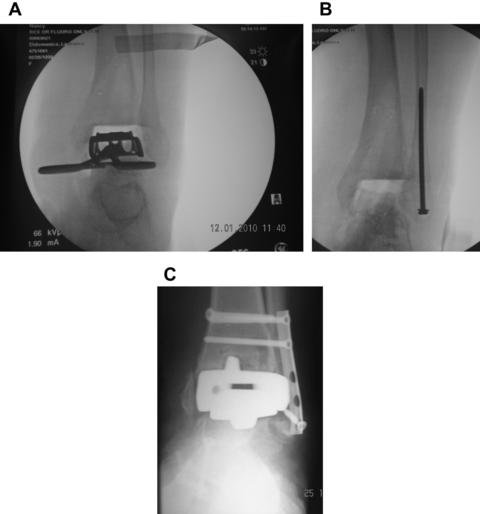
Complications leading to failure of TAR can be caused by several factors. The necessity for revision may be linked to the type of implant system used, surgeon experience in performing the procedure, or the severity of the patient’s preoperative condition. Specifically, it has been found that surgeon experience can be related to long-term survival rate of ankle implants. Research has shown that after the surgeon has performed the application of 30 implants, the 5-year success rate increases from 70% to 86% (Fig. 1).11
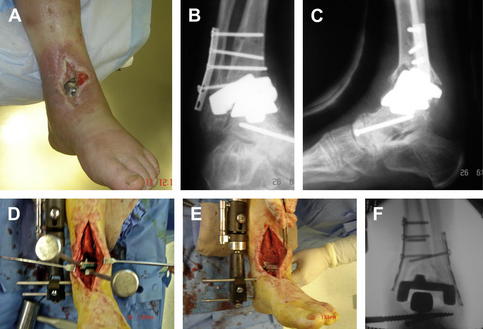
Historically, aseptic prosthetic loosening and wound healing issues were among the most common complications arising after TAR with mechanical loosening occurring most commonly.2,8,11 Other problems that frequently occur include infection of bone and soft tissue, nonunion of the tibiofibular syndesmosis, malalignment, joint impingement, and persistent pain (Fig. 2).5
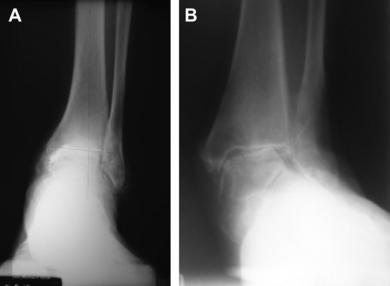
A thorough understanding of ankle joint anatomy is key for interpreting the mechanical and functional relationship between the prosthesis and joint, and may lend insight into mechanisms of failure.15 Because of the lack of muscular reinforcement between the talus and surrounding bony structures, there is increased importance placed on the quality and integrity of the surrounding ligamentous structures (Fig. 3).16
One of the factors that make successful application of TAR inherently challenging is that many of the conditions that warrant the initial need for augmentation of the joint may cause complications after application. Preoperative failure to recognize inherent soft tissue or bony structural deformities contributes to this problem. Furthermore, inadequate soft tissue repair or component placement could be contributory factors to subsequent failure.7,17 Tibiotalar varus or valgus have been linked to the highest incidence of complications.6 It has been recommend that TAR procedures be avoided in patients with a coronal deformity of greater than 10 to 15 degrees.18 In addition, equinus deformity has been noted to be an impacting factor in TAR, and some authors have recommended performing lengthening of the Achilles tendon if less than 5 degrees of dorsiflexion is achieved after placement of the implant.11 This and other adjunctive procedures including osteotomies, arthrodesis, or tendon transfers may be necessary to provide the best environment for successful TAR outcomes (Fig. 4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree