Current Concepts and Techniques in Foot and Ankle Surgery
Pinch Graft Harvesting Technique for Surgical Closure of the Diabetic Foot
Keywords
• Diabetic foot • Wound • Surgery • Pinch grafts • Skin grafts • Neuropathy
Introduction
Skin grafting remains a mainstay of treatment for diabetic wounds that cannot be closed primarily or through standard local wound care. This procedure dates back to ancient times, first mentioned in Sanskrit manuscripts in 3000 bc, yet was first published for healing of ulcerations in 1869.1 The decision to use a skin graft depends on wound condition, location, size, and esthetic considerations.2 Specific techniques for skin grafting have evolved over time with regard to choices in donor sites, harvesting, and postoperative management of both the donor and recipient sites. Options for expedited, definitive closure can be limited based on the nature and location of the wound, as often seen in diabetic patients presenting with soft tissue loss following surgical debridement for complex foot infections.3 Pinch grafting has served as a viable method for treatment of venous and diabetic ulcerations of the leg1; however, the surgical approach consisting of both donor and recipient sites located in the foot is unique. A case is presented illustrating the technique for pinch grafting harvested from the plantar forefoot to address a chronic diabetic foot ulceration.
Case report
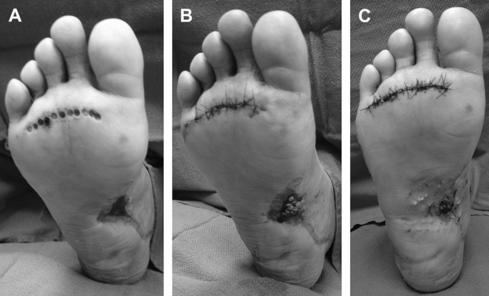
The patient was medically optimized by her primary care physician before surgery. Intravenous sedation with local anesthesia was administered to the patient in the operating room setting. Recipient wound bed preparation was performed to stimulate healthy bleeding via curettage and hydrosurgical debridement. The remaining 4 × 1-cm wound had no infection or necrosis and had a completely granular base. At the plantar aspect of the ipsilateral forefoot, just distal to the metatarsal heads, the donor site was marked with 2 semi-elliptical converging lines where the multiple pinch grafts were going to be harvested. The donor skin was infiltrated with 3 mL of 1% lidocaine with epinephrine and then using a 4-mm punch biopsy instrument, 11 separate pinch grafts were obtained through full-thickness skin, avoiding subcutaneous fat. The grafts were placed in saline temporarily while the remaining skin at the donor site was sharply excised in elliptical fashion following the previous markings. Primary closure of the donor site was performed using nonabsorbable suture in simple interrupted technique without tension. All 11 pinch grafts were carefully placed into the recipient wound bed at approximately 2-mm intervals, filling the defect. Topical thrombin was applied to the grafted site followed by a bolster-type dressing consisting of nonadherent gauze and saline-moistened sponges secured in place by skin staples and dry gauze dressing (Fig. 1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree