Occipitocervical and C1-C2 Fusion with Instrumentation
S. Babak Kalantar
Youjeong Kim
Maneesh Bawa
John M. Rhee
John G. Heller
DEFINITION
The term occipitocervical and atlantoaxial instability encompasses a number of varied conditions that compromise the normal function of the O-C1 and C1-C2 joints, resulting in either pain, spinal cord dysfunction, or the threat thereof.
Instability can result from trauma, including fractures of the articular masses and occipital condyles, rupture of the transverse ligament, odontoid fracture, or Jefferson fracture. Nontraumatic causes include inflammatory arthropathy (most commonly rheumatoid arthritis), osteoarthritis, congenital anomalies, rotatory subluxation, tumor, and infection.
Several methods have been described for stabilizing the atlantoaxial complex, as well as the occipitocervical junction, including wiring techniques, transarticular screw fixation, plate and screw fixation, and screw and rod fixation.
We describe our technique for occipitocervical plating; transarticular screw fixation; articular mass screw and rod construct to achieve atlantoaxial arthrodesis with C2 pars, pedicle, and translaminar screw fixation; and C1-C2 wiring techniques.
ANATOMY
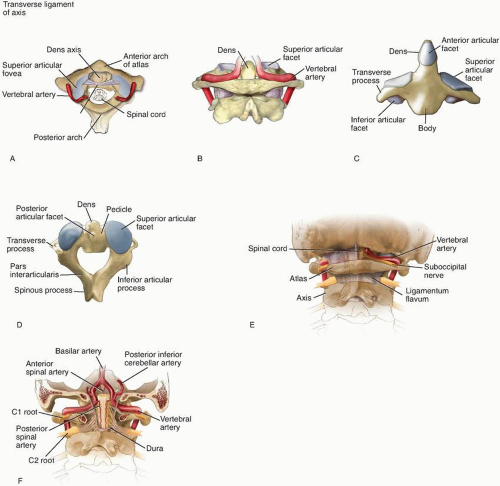
The base of the skull is composed of the external occipital protuberance (EOP), the occipital condyles (which articulate with the C1 lateral masses), and foramen magnum. Landmarks noted on posterior dissection are the posterior edge of the foramen magnum, the superior nuchal line, the inferior nuchal line, and the external protuberance (FIG 1).
The nuchal lines serve as attachments to the paired neck muscles. The trapezius attaches to the superior line and the rectus capitis attaches to the inferior line
The nuchal ligament attaches to the external protuberance.
The thickness of the bone in the suboccipital region varies depending on location. In the midline, the internal occipital crest has a mean thickness of 8.3 mm at the level of the inferior nuchal line, increasing to a mean of 13.8 mm at the EOP. The lateral bone is thinner, ranging from a mean of 3.7 mm at the level of the inferior nuchal line and increasing to a mean of 8.3 mm at the level of the superior nuchal line.1
The first cervical vertebra, or the atlas (C1), is unlike any other in that it lacks a vertebral body and spinous process. It consists of an anterior and posterior arch connected by two articular masses, forming a ring that pivots about the odontoid process of C2 (FIG 2A).
On each side of the cranial surface of the C1 posterior arch, there is a groove for the vertebral artery, the first cervical nerve, and their associated venous complex (FIG 2B). In a small subset of the population, this groove is covered by an arch of bone, the ponticulus posticus. The resulting foramen is identified as the arcuate foramen.2
The articular masses of C1 give rise to the superior and inferior articular facets, which are broad and articulate, with the occipital condyles superiorly and the axis inferiorly.
A synovial joint also is located between the posterior aspect of C1 and the odontoid process of the axis.
The axis (C2) has thicker laminae and a larger bifid spinous process than the subaxial cervical vertebra. It is characterized further by an odontoid process that projects upward from the vertebral body. Lateral to the odontoid process, or dens, are the sloping superior articular surfaces, which articulate with the inferior articular facets of C1, forming the atlantoaxial joint. The C2 pedicle can be identified in a zone between the lamina and vertebral body, projecting superomedially (FIG 2C,D).
O-C1 articulation: The kidney-shaped lateral masses of the atlas articulate cranially with the kidney-shaped occipital condyles. The joint allows for 15 to 20 degrees flexion and extension with 5 to 10 degrees of lateral bending.3 Stability depends on the joint ligaments, the tectorial membrane, and the longitudinal bands of the cruciate ligaments.
C1-C2 articulation: The C1-C2 complex is composed of three articulations—two laterally composed of the inferior C1 and superior C2 articular facets, and one anteriorly between the dens and the posterior aspect of the anterior C1 arch.
The C1-C2 articulation allows for 47 degrees of rotation to either side, which is approximately 50% of the lateral rotation of the entire cervical spine.4 Panjabi and associates5 showed that in the healthy spine, C1-C2 flexion is 11.5 degrees, extension is 10.9 degrees, lateral bending is 6.7 degrees, and axial rotation to each side is 38.9 degrees.
The vertebral artery, which is the first branch of the subclavian artery medial to the anterior scalene muscle, ascends behind the common carotid artery. It then ascends through
the foramina transversaria from C6 to C1. After traversing through the foramina transversaria at C1, the artery takes a sharp turn medially and posteriorly to course behind the C1 articular mass along the groove in the posterior arch of C1. It then passes through the posterior atlanto-occipital membrane before ascending through the foramen magnum as it merges with its counterpart to form the basilar artery (FIG 2E,F).
The C1 nerve root, or the suboccipital nerve, exits cranial to the posterior arch of C1 and innervates muscles of the suboccipital triangle. The C2 nerve root, or greater occipital nerve, exits between the posterior arches of C1 and C2, posterior to the superior C1-C2 articulation. It does not exit through a true foramen like the remaining subaxial cervical nerve roots. It traverses inferior to the obliquus capitis inferiorly to ascend through the semispinalis capitis to lie superficial to the rectus capitis. Injury to the greater occipital nerve can lead to dysesthesia of the posterior scalp and can be troublesome to patients.
PATHOGENESIS
Stability of the O-C1 articulation relies on the ligamentous support and anatomic contour of the occipital condyles on the lateral masses of C1. Occipital condyle fractures may be stable or represent the bony component of an occipitocervical dissociation (OCD). OCD involves disruption of the ligamentous constraints resulting in an injury with high mortality rate.6
Stability of the C1-C2 articulation relies heavily on its ligamentous restraints, including the transverse, alar, and apical ligaments, and the facet capsules. Trauma may disrupt these ligamentous restraints. Also, with the advanced degeneration found in arthritic conditions, these ligamentous structures may become incompetent.
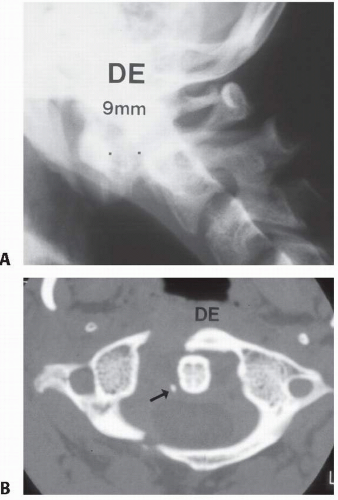
Up to 3 mm of anterior translation of C1 on C2, as measured by the anterior atlantodental interval (AADI) on a lateral cervical radiograph, is normal. An atlantodental interval of 3.5 to 5 mm in an adult indicates potential damage to the transverse ligament, whereas an interval greater than 5 mm indicates probable injury to the transverse ligament and accessory ligaments (FIG 3A).
In cases of trauma, an atlantodental interval greater than 3.5 mm probably is an indication for further evaluation and most likely requires C1-C2 arthrodesis.
In patients with inflammatory arthropathy, including rheumatoid arthritis, a canal diameter identified as posterior atlantodental interval (PADI) smaller than 14 mm is associated with a worse outcome and is an indication for decompression and fusion.7 The exact AADI measurement is not as relevant in these patients as with trauma patients.
Fractures that involve the osseous structures of C1 and C2 also may result in atlantoaxial instability and require arthrodesis (FIG 3B).
NATURAL HISTORY
In the event of trauma to the occipital condyles, careful evaluation with computed tomography (CT) and possibly magnetic resonance imaging (MRI) is indicated to rule out associated OCD. In the setting of an OCD, patient mortality can be high and operative management is recommended. Any translation or distraction at that level is an indication for intervention. Traction is contraindicated. Immediate immobilization followed by occipitocervical fusion is indicated.
In the event of C1-C2 trauma, the potential need for surgery arises in the setting of ligamentous instability, fractures, or a combination of the two. Atlantoaxial instability due to rupture of the transverse ligament represents a threat to the cervical spinal cord with a low likelihood of successful healing. Thus, C1-C2 fusion is indicated.
Transverse ligament disruption in association with a Jefferson fracture may represent an exception to this rule, in that, successful nonoperative fracture treatment (halo vest) can lead to a “stable” C1-C2 segment on flexion-extension radiographs.
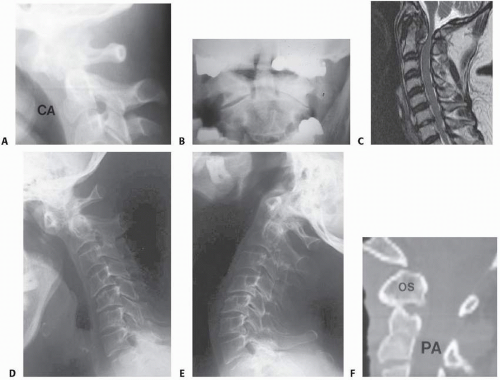
Fractures of the odontoid process may represent a primary indication for C1-C2 fusion if nonoperative means (eg, halo vest immobilization) cannot obtain or maintain an appropriate reduction or if a patient elects surgery to avoid the use of a halo. Displaced odontoid fractures have an increased likelihood of resulting in either non- or malunion in the cases of type II and III fractures, respectively (FIG 4A).
Primary atlantoaxial osteoarthritis is quite painful and responds poorly to nonoperative means. C1-C2 fusion affords a high likelihood of symptom relief (FIG 4B).
Cervical myelopathy due to either rheumatoid pannus or pseudopannus formation, as seen in older individuals with extensive subaxial spondylosis and spontaneous fusion, is unlikely to improve without fusion of the C1-C2 segment (FIG 4C).
C1-C2 instability due to rheumatoid arthritis may be neither symptomatic nor a neurologic threat. Thus, in this case, an ADI exceeding 3.5 mm is not, by itself, an indication for surgery. A PADI of less than 14 mm or the presence of myelopathy is a poor prognostic sign and indicates the need for surgery. Painful C1-C2 rheumatoid involvement in the face of adequate medical therapy also indicates the need for surgery.
Basilar invagination or cranial setting of the occipitocervical junction due to rheumatoid arthritis can result in cervicomedullary cord compression. Especially in the presence of myelopathic symptoms, occipitocervical fusion with or without decompression is indicated.
Progressive C1-C2 subluxation, especially with cranial settling, also has an unfavorable natural history. C1-C2 fusion in this instance will obviate the need for a future occipitocervical fusion, which has a less favorable influence on the overall condition of the cervical spine (FIG 4D,E).
The natural history of asymptomatic C1-C2 instability associated with miscellaneous conditions such as os odontoideum (FIG 4F) and Down syndrome is less clear. When such patients have symptoms, myelopathic signs, or an insufficient PADI, the potential benefits of a C1-C2 fusion probably outweigh the risks of the natural history. The patient’s age, lifestyle, and activity level also must be considered in determining the need for surgery.
HISTORY AND PHYSICAL FINDINGS
A complete history and physical examination, including a thorough neurologic examination, should be performed when evaluating a patient with occipitocervical and/or C1-C2 pathology. The complaints offered will vary with the presentation (eg, trauma, inflammatory arthritis, developmental, congenital).
Patients with a traumatic injury may not only complain of isolated pain but also may present with neurologic deficits. A low threshold of suspicion should be maintained for patients with blunt trauma to the head or face or with known noncontiguous fractures of the spine.
Some patients with rheumatoid arthritis may complain only of axial neck pain, whereas others may present with deteriorating gait and bilateral hand numbness or clumsiness without significant neck pain.
Patients with primary atlantoaxial arthritis will complain of severe neck and head pain, most often unilateral, with varying degrees of refusal to rotate their head, especially ipsilaterally toward the pain. Locking or crepitation of the affected joint may be both audible and palpable.
Physical examination should include the following:
Active self-limited rotation of the head, especially toward the side of the pain. Normal rotation is up to 50 degrees of rotation to either side. C1-C2 pathology often causes pain that limits rotation.
Palpation of the suboccipital area near the interval between the posterior arches of C1 and C2 may elicit pain. When asked, the patient often can point to the source of their pain.
Response to traction versus compression combined with passive C1-C2 rotation. The patient is examined supine with his or her head resting comfortably on a pillow. Passive lateral head rotation is measured with slight manual traction. In cases of C1-C2 arthritis, this maneuver should provide more motion and less pain than similar motion with an axial load. With slight manual traction, head rotation is increased, whereas an axial load may cause pain and result in decreased rotation.
In the setting of potential traumatic instability, however, these examination maneuvers are not applicable. The cervical spine must be immobilized until the radiographic and CT findings are known.
IMAGING AND OTHER DIAGNOSTIC STUDIES
In the setting of blunt trauma, plain radiographs of the cervical spine, specifically the upper cervical spine, have been shown to be inadequate. McCulloch et al8 reported that plain radiographs have a sensitivity of 52%, a specificity of 98%, a positive predictive value (PPV) of 81%, and a negative predictive value (NPV) of 93%, whereas helical CT had a sensitivity and specificity of 98%, PPV of 81%, and NPV of 93%. They concluded that although helical CT has limited ability to detect pure ligamentous injury, it is superior to plain radiographs when evaluating patients with high-energy trauma for cervical spine fractures.
MRI scan is the most effective diagnostic tool for identification of ligamentous and other soft tissue injury.9
Patient-controlled flexion-extension plane radiographs may be beneficial in certain situations. However, studies have shown that even extensive damage to the intervertebral structures may inconsistently result in abnormal findings using this tool.10 In addition, patient effort may play a role in the ability to obtain reliable results.11
CT with sagittal and coronal reconstruction is done routinely for diagnostic purposes as well as for preoperative planning.
Fractures of either C1 or C2 indicate a significant likelihood of additional cervical spine fractures. As many as 50% of C1 fractures may be associated with other fractures.
A vertebral artery angiogram is recommended when there is any question of acute injury or history of injury to the vertebral arteries. A unilateral vertebral artery injury rarely is symptomatic because of sufficient collateral flow through the contralateral vertebral artery as well as the circle of Willis. A patient with a vertebral artery injury who presents with neurologic deficits due to a concomitant spinal cord injury may be especially difficult to diagnose clinically.
We recommend imaging with either an angiogram or an magnetic resonance arthrogram (MRA) in all patients presenting with a significant flexion-distraction injury, fracture that extends into the transverse foramen, or facet dislocation (FIG 5).
The method of treatment of vertebral artery injuries associated with cervical trauma remains controversial, especially with asymptomatic injuries. When discovered, symptomatic vertebral artery injuries may be treated with anticoagulation to prevent thromboembolic complications. If a surgical procedure is necessary, anticoagulation is stopped before and restarted after surgery.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree