Neurovascular Injury Following Total Hip Arthroplasty
Gregg R. Klein
Harlan B. Levine
Neurologic Injury
Neurologic injury following total hip arthroplasty is a rare but devastating complication that can have potentially significant short- and long-term sequela resulting in morbidity for the patient and potential legal exposure for the surgeon. Fortunately, neurologic injury associated with total hip arthroplasty is an infrequent complication.
Case
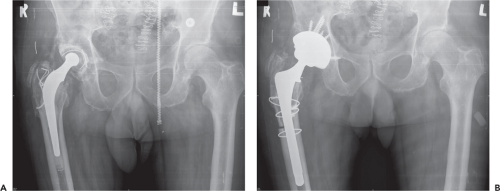
A 78-year-old male had a complex right hip revision after a Charnley arthroplasty 28 years earlier (Fig. 83.1A). Intraoperatively there was acetabular osteolysis and bone loss. A revision of the acetabular component was performed with multiple screws used for fixation. An extended trochanteric osteotomy was performed for cement removal and a fully coated femoral stem was placed (Fig. 83.1B). Postoperatively the patient was noted to be unable to dorsiflex his ankle or to extend his great toe. Plantarflexion, however, was noted to be 5/5. An injury to the peroneal branch of the sciatic nerve was diagnosed. A neurology consult was obtained and an AFO was ordered. An electromyography (EMG) performed at 6 weeks revealed an injury to the common peroneal branch of the sciatic nerve.
Central Nervous System Injury
Stroke
Central nervous system injury following total hip arthroplasty occurs rarely and often manifests either as a cerebral vascular accident or as the sequela of fat embolism. Lalmohamed et al. (1) found a 4.7-fold increased risk of ischemic stroke and a 4.4-fold increased risk of hemorrhagic stroke within the first 2 weeks following total hip arthroplasty in the Danish registry (66,583 THAs between 1998 and 2007). This risk remained elevated during the first six postoperative weeks for ischemic stroke and the first 12 weeks for hemorrhagic stroke. They
found that antiplatelet drug usage reduced the 6-week risk for ischemic stroke by 70% but did not affect the risk of hemorrhagic stroke. Similarly, Popa et al. (2) found a 3.9% increased risk of stroke in the first year following THA. Age greater than 75 years old, as well as a history of atrial fibrillation, hip fracture repair, aspirin usage, and previous stroke were identified as univariate risk factors CVA following THA in that series.
found that antiplatelet drug usage reduced the 6-week risk for ischemic stroke by 70% but did not affect the risk of hemorrhagic stroke. Similarly, Popa et al. (2) found a 3.9% increased risk of stroke in the first year following THA. Age greater than 75 years old, as well as a history of atrial fibrillation, hip fracture repair, aspirin usage, and previous stroke were identified as univariate risk factors CVA following THA in that series.
Fat Embolism Syndrome
Fat embolism syndrome (FES) is diagnosed following total hip arthroplasty by varying degrees of respiratory distress, cerebral dysfunction, and petechial rash. Typical pulmonary findings included shortness of breath and hypoxemia. Mental status changes range from agitation to delirium or coma. Although respiratory distress and cerebral dysfunction are earlier findings in FES, the petechial rash typically presents later 24 to 48 hours after surgery. A high index of suspicion is necessary in making the diagnosis as not all of these clinical findings are necessarily found in cases of FES. For example, a petechial rash over the anterior torso and upper arms has been thought to be pathognomonic of FES. However, this rash is only seen in approximately 20% to 50% of cases.
FES occurs when bone marrow contents including fat are released into the bloodstream. During total hip arthroplasty, such translocation of bone marrow contents may occur during femoral canal preparation including broaching, reaming, irrigation, cementation as well as during implant placement (3). The onset of fat emboli syndrome occurs infrequently and the pathophysiology of FES is poorly defined. It is felt that both a mechanical blockage of the capillaries in the end organs as well as the release of fatty acids cause local toxicity to the endothelial lining of the vasculature which culminates in the onset of FES. The diagnosis of FES is made by clinical diagnosis. There are no distinct radiographic or laboratory findings for FES. A chest x-ray may look like a “snowstorm” secondary to the uniform distribution of small pulmonary shadows, and/or may show enlarged pulmonary markings and an enlarged right heart. Interleukin-6 has been evaluated as an early marker of FES in a trauma setting. Prakash found that elevated serum IL-6 levels at 12 hours after pelvic or long bone fractures correlated with an increased probability of FES development (3).
The treatment for FES is supportive care and maintenance of pulmonary function. Corticosteroids have been used to decrease the sequela of FES. However, there are no large studies to support their widespread usage as a treatment for FES. In a meta-analysis, Bederman et al. (4) found that corticosteroids may help to prevent FES and hypoxia but not mortality in a trauma patient population. With early diagnosis and appropriate supportive care the prognosis for FES is typically good (5).
PERIPHERAL NERVE INJURY
Peripheral nerve injury is a rare complication associated with total hip arthroplasty. Such injuries range from a dysfunction in the normal nerve conduction pathways (neuropraxia) to a fulminant structural blockage in nerve conduction (axonotmesis or neurotmesis). There are few studies that report on the rate of nerve injury in the literature. Oldenburg found a rate of peripheral nerve injury following THA of 2.24% in a retrospective review of 2,713 cases. In this series there were 13 (0.48%) sciatic nerve injuries, 33 (1.2%) peroneal nerve injuries, and 15 (0.5%) femoral nerve injuries. The risk in revision THA was 3.06% and found to be increased in isolated acetabular revision (8.5%.), potentially related to the difficulties in exposure when the stem was retained (6). Others report rates of injury ranging from 0.1% to 1.9% (7,8,9).
Yacub et al. (10) reviewed 14,979 patients who underwent either a total hip arthroplasty, total knee arthroplasty, or knee arthroscopy and found that there was a peripheral nerve injury rate of 0.03% following total hip arthroplasty. Schmalzried reviewed a series of 3,126 total hip arthroplasties and found a neurologic injury rate of 1.7% in patients who were being treated for a hip diagnosis other than hip dysplasia. The rate of neurologic injury went up to 5.2%, however, for patients being treated for hip dysplasia. In addition, in this series of patients, the rate of peripheral nerve injury in revision total hip arthroplasty was 3.2% (11). Others have reported a 7.5% rate of peripheral nerve injury in revision total hip arthroplasty (7).
However, the rate of peripheral nerve injury following total hip arthroplasty may be underdiagnosed as the signs and symptoms of such injuries may be falsely attributed to other sources of pain and dysfunction more commonly seen in the postoperative period. In addition, the signs and symptoms of peripheral nerve injury may be too mild to meet the clinical threshold for diagnosis. Weber et al. (12) examined 30 hips in patients receiving a total hip arthroplasty with preoperative and postoperative EMGs and found an asymptomatic peripheral nerve injury rate approaching 70%.
The nerves that are most in jeopardy during total hip arthroplasty are those that are near the surgical field. Typically these include the sciatic, femoral–obturator, and superior gluteal nerves (Table 83.1). In most cases, the mechanism of injury is unknown (Table 83.2) (7).
Lumbar spine disease including stenosis and disc disease potentiates the risk for peripheral nerve injury through a so-called “double crush phenomenon” (13). Although the exact pathogenesis for this increased susceptibility to injury remains unknown it is theorized that a proximal lesion causes disturbances in axonal flow kinetics which lowers the downstream injury threshold (14). Therefore a history of lumbar spinal disease, radiculopathy or other proximal nerve lesions should be noted preoperatively so as to appropriately guide the patient’s expectations as well as the postoperative management of peripheral nerve injuries.
Table 83.1 Distribution of Nerve Injury after THA | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
The risk of peripheral nerve injury does not appear to be influenced by the type of anesthesia used during total hip
arthroplasty. In comparing the risk of peripheral nerve injury with the use of general anesthesia versus neuraxial anesthesia or peripheral nerve blockade in cohort of 12,998 patients over a 20-year period, Jacob et al. (15) found no difference in the risk of peripheral nerve injury. In this study the risk for peripheral nerve injury was associated with younger age, female sex, prolonged operative times, and the use of a posterior surgical approach.
arthroplasty. In comparing the risk of peripheral nerve injury with the use of general anesthesia versus neuraxial anesthesia or peripheral nerve blockade in cohort of 12,998 patients over a 20-year period, Jacob et al. (15) found no difference in the risk of peripheral nerve injury. In this study the risk for peripheral nerve injury was associated with younger age, female sex, prolonged operative times, and the use of a posterior surgical approach.
Table 83.2 Mechanism of Nerve Injury | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Sciatic Nerve
By far the sciatic nerve remains the most commonly injured nerve, accounting for up to 80% of peripheral nerve injuries in total hip arthroplasty (Fig. 83.2). At the level of the hip joint the peroneal and tibial fibers travel within the same nerve sheath and are both susceptible to injury. However, the peroneal fibers are most vulnerable and studies have shown that they are involved in approximately 94% to 99% of sciatic nerve injuries, with the tibial fibers involved in 41% (7,11). Isolated peroneal involvement has been reported in 47% to 65% cases and isolated tibial involvement in only 0.5% and 2% of sciatic nerve injuries.
The peroneal division of the sciatic nerve is more susceptible to injury for several reasons including a greater density of nerve fibers relative to tibial nerve and its more lateral position places it closer to the operative field (Fig. 83.2), making them more susceptible to compression and stretching during total hip arthroplasty (16,17). Several risk factors for sciatic nerve injury have been identified (Table 83.3) and include leg lengthening greater than 2.7 to 4.0 cm, hip dysplasia, female sex, excision of heterotopic bone, a deficient posterior wall, a posterior surgical approach, use of a cementless femoral implant, and revision as opposed to primary hip arthroplasty (11,18,19,20).
Femoral Nerve
Injury to the femoral nerve is the second most frequent peripheral nerve injury in total hip arthroplasty. Schmalzried found that femoral nerve injuries accounted for 13% of peripheral nerve injuries following total hip arthroplasty (7). In a consecutive series of 440 total hip arthroplasties performed over a 1-year period, there were 10 femoral nerve injuries (2.3%) (9). Injury to the femoral nerve typically happens through direct injury from an anterior acetabular retractor, or the placement of prosthetic components including the acetabular cup, acetabular screws, or cement. Typically the femoral nerve is protected by the iliopsoas muscle which lies anterior to the anterior wall of the acetabulum (Fig. 83.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree