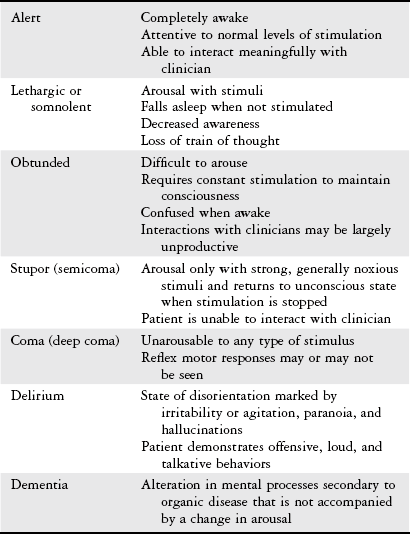
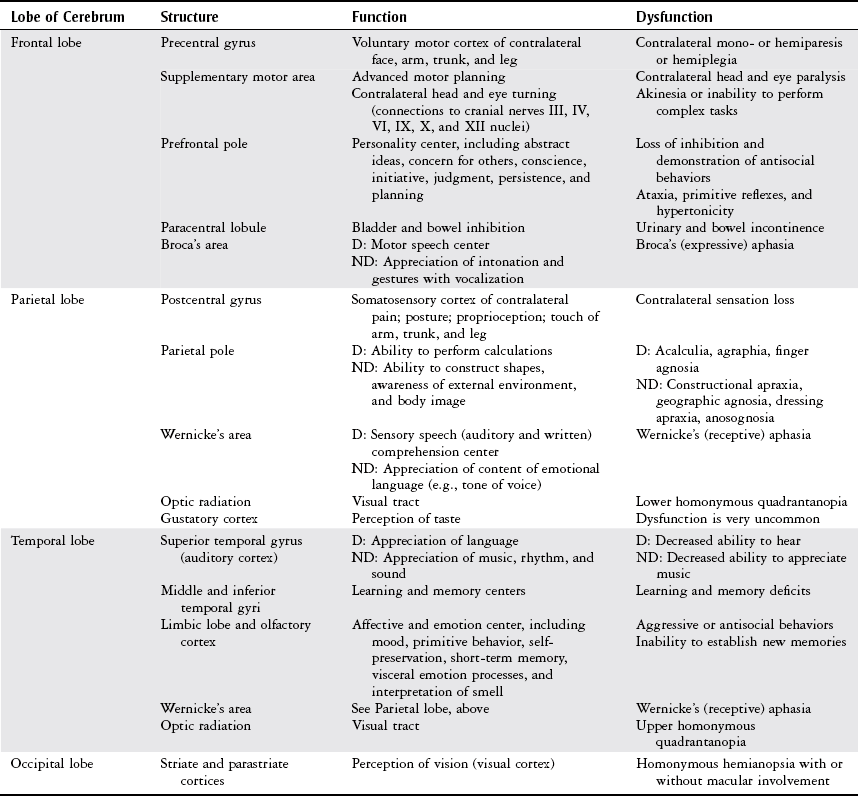
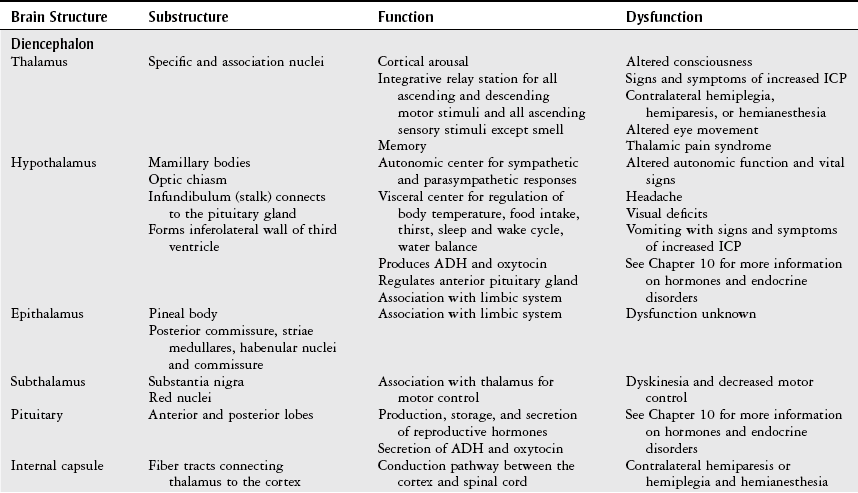
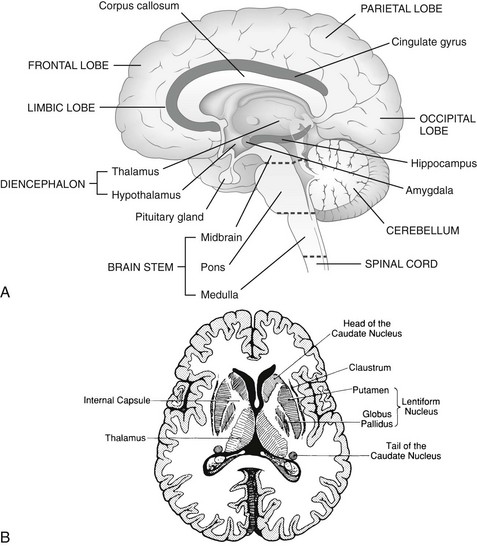
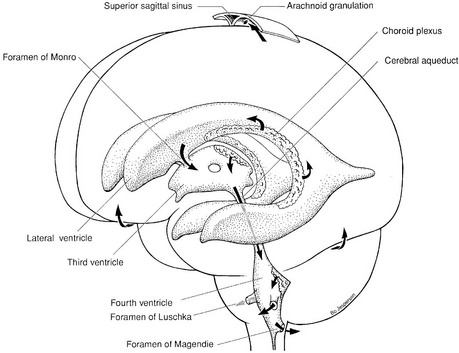
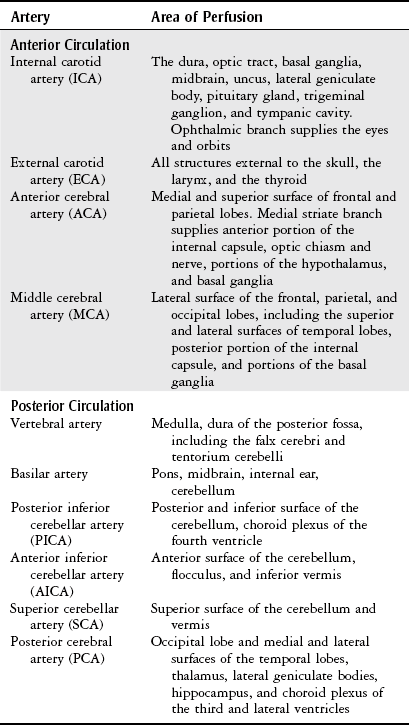
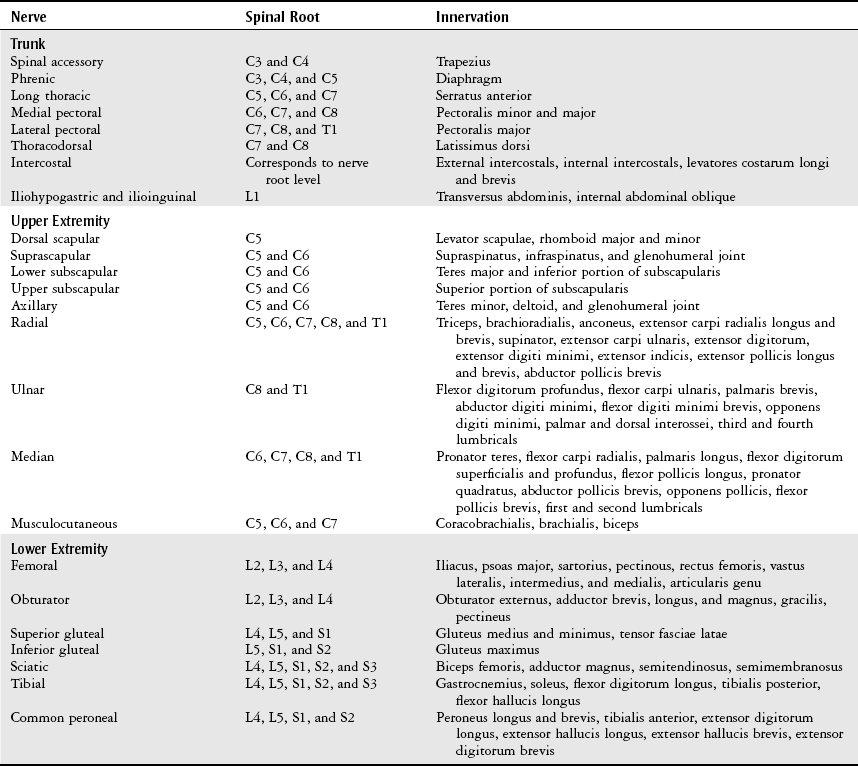
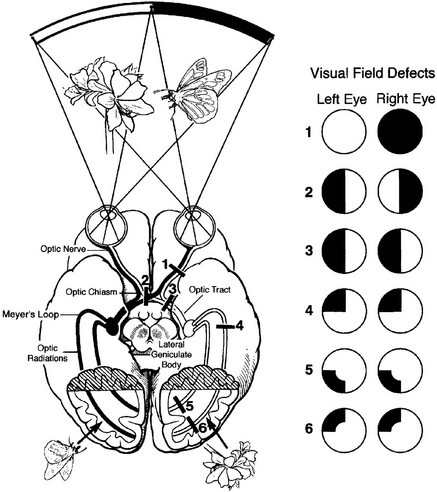
Chapter 6 The objectives of this chapter are to provide the following: 1 Provide a brief review of the structure and function of the nervous system 2 Give an overview of neurologic evaluation, including the physical examination and diagnostic tests 3 Describe common neurologic diseases and disorders, including clinical findings, medical and surgical management, and physical therapy interventions • Common Degenerative Central Nervous System Diseases (Amyotrophic Lateral Sclerosis, Guillain-Barré Syndrome, Multiple Sclerosis, Parkinson’s Disease, Huntington’s Disease): 5A, 5E, 5G, 6B, 6E, 7A • Vestibular Dysfunction (Bilateral Vestibular Hypofunction, Ménière’s Disease, Acute Vestibular Neuronitis, Benign Positional Paroxysmal Vertigo, Vertigo, Lightheadedness, Dysequilibrium): 5A • Neuroinfectious diseases (Encephalitis, Meningitis, and Poliomyelitis [more information in Chapter 13]): 4A, 5C, 5D, 5G, 5H, 6E, 7A • Seizure (Status Epilepticus, Epilepsy, Simple Partial Seizures, Complex Partial Seizures, Tonic-Clonic Seizures): 5A, 5C, 5D, 5E • Ventricular Dysfunction (Cerebrospinal Fluid Leak and Hydrocephalus): 5C, 5D • Spinal Cord Injury: 5H, 7A, 7C • Traumatic Brain Injury: 5C, 5D, 5I • Cerebrovascular Disease and Disorders (Transient Ischemic Attack, Cerebrovascular Accident, Dementia, Subarachnoid Hemorrhage, Arteriovenous Malformation and Cerebral Aneurysm): 5C, 5D, 5I, 6E, 6F, 7A Please refer to Appendix A for a complete list of the preferred practice patterns, as individual patient conditions are highly variable and other practice patterns may be applicable. The nervous system is divided as follows: • The central nervous system (CNS), consisting of the brain and spinal cord • The peripheral nervous system, consisting of efferent and afferent nerves outside the CNS The peripheral nervous system is divided into: • The autonomic (involuntary) nervous system, consisting of the sympathetic and parasympathetic systems innervating the viscera, smooth muscles, and glands • The somatic (voluntary) nervous system, consisting of efferent and afferent nerves to all parts of the body except the viscera, smooth muscles, and glands The brain is anatomically divided into the cerebral hemispheres, diencephalon, brain stem, and cerebellum. A midsagittal view of the brain is shown in Figure 6-1, A. Figure 6-1, B shows the basal ganglia and the internal capsule. Although each portion of the brain has its own function, it is linked to other portions via tracts and rarely works in isolation. When lesions occur, disruption of these functions can be predicted. Tables 6-1 and 6-2 describe the basic structure, function, and dysfunction of the cerebral hemispheres, diencephalon, brain stem, and cerebellum. TABLE 6-1 Structure, Function, and Dysfunction of the Cerebral Hemispheres Data from Gilman S, Newman SW, editors: Manter and Gatz’s essentials of clinical neuroanatomy and neurophysiology, ed 7, Philadelphia, 1989, FA Davis; Kiernan JA, editor: Introduction to human neuroscience, Philadelphia, 1987, Lippincott; Marieb EN, editor: Human anatomy and physiology, ed 5, San Francisco, 2001, Benjamin-Cummings; Thelan L, Davie J, Lough M, editors: Critical care nursing: diagnosis and management, ed 2, St Louis, 1994, Mosby; Mancell EL, editor: Gray’s clinical neuroanatomy: the anatomic basis for clinical neuroscience, Philadelphia, 2011, Elsevier Saunders; O’Sullivan SB, Schmitz TJ, editors: Physical rehabilitation, ed 5, Philadelphia, 2007, FA Davis. TABLE 6-2 Structure, Function, and Dysfunction of the Diencephalon, Brain Stem, and Cerebellum ADH, Antidiuretic hormone; CN, cranial nerve; ICP, intracranial pressure. Data from Gilman S, Newman SW, editors: Manter and Gatz’s essentials of clinical neuroanatomy and neurophysiology, ed 7, Philadelphia, 1989, FA Davis; Kiernan JA, editor: Introduction to human neuroscience, Philadelphia, 1987, Lippincott; Marieb EN, editor: Human anatomy and physiology, ed 5, San Francisco, 2001, Benjamin-Cummings; Thelan L, Davie J, Lough M, editors: Critical care nursing: diagnosis and management, ed 2, St Louis, 1994, Mosby; Mancell EL, editor: Gray’s clinical neuroanatomy: the anatomic basis for clinical neuroscience, Philadelphia, 2011, Elsevier Saunders; O’Sullivan SB, Schmitz TJ, editors: Physical rehabilitation, ed 5, Philadelphia, 2007, FA Davis. FIGURE 6-1 A, Schematic midsagittal view of the brain shows the relationship between the cerebral cortex, cerebellum, spinal cord, and brainstem and the subcortical structures important to functional movement. B, Horizontal section of the cerebrum showing the basal ganglia. (A, From Cech DJ, Martin ST: Functional movement development across the life span, ed 3, St Louis, 2012, Saunders. B, From Love RJ, Webb WG, editors: Neurology for the speech-language pathologist, ed 4, Boston, 2001, Butterworth-Heinemann, p 38.) The brain is protected by the cranium, meninges, ventricular system, and blood-brain barrier. The cranium encloses the brain. It is composed of eight cranial and 14 facial bones connected by sutures and contains approximately 85 foramina for the passage of the spinal cord, cranial nerves (CNs), and blood vessels.1 The cranium is divided into the cranial vault, or calvaria (the superolateral and posterior aspects), and the cranial floor, which is composed of fossae (the anterior fossa supports the frontal lobes; the middle fossa supports the temporal lobes; and the posterior fossa supports the cerebellum, pons, and medulla).2 The meninges are three layers of connective tissue that cover the brain and spinal cord. The dura mater, the outermost layer, lines the skull (periosteum) and has four major folds (Table 6-3). The arachnoid, the middle layer, loosely encloses the brain. The pia mater, the inner layer, covers the convolutions of the brain and forms a portion of the choroid plexus in the ventricular system. The three layers create very important anatomic and potential spaces in the brain, as shown in Figure 6-2 and described in Table 6-4. TABLE 6-3 Data from Wilkinson JL, editor: Neuroanatomy for medical students, ed 3, Oxford, UK, 1998, Butterworth-Heinemann. TABLE 6-4 The ventricular system nourishes the brain and acts as a cushion by increasing the buoyancy of the brain. It consists of four ventricles and a series of foramina, through which cerebrospinal fluid (CSF) passes to surround the CNS. CSF is a colorless, odorless solution produced by the choroid plexus of all ventricles at a rate of 400 to 500 ml per day.2 CSF circulates in a pulse-like fashion through the ventricles and around the spinal cord with the beating of ependymal cilia that line the ventricles and intracranial blood volume changes that occur with breathing and cardiac systole.3 The flow of CSF under normal conditions, as shown in Figure 6-3, is as follows4: FIGURE 6-3 The ventricular system of the brain. Arrows indicate the circulation of cerebrospinal fluid from the site of formation in the choroid plexus to the site of absorption in the villi of the sagittal sinus. (From Bogousslavsky J, Fisher M, editors: Textbook of neurology, Boston, 1998, Butterworth-Heinemann, p 656.) • From the lateral ventricles via the interventricular foramen to the third ventricle • From the third ventricle to the fourth ventricle via the cerebral aqueduct • From the fourth ventricle to the cisterns, subarachnoid space, and spinal cord via the median and lateral apertures When ventricular pressure is greater than venous pressure, CSF is absorbed into the venous system via the arachnoid villi, capillary walls of the pia mater, and lymphatics of the subarachnoid space near the optic nerve.2 The blood-brain barrier is the physiologic mechanism responsible for keeping toxins, such as amino acids, hormones, ions, and urea, from altering neuronal firing of the brain. It readily allows water, oxygen, carbon dioxide, glucose, some amino acids, and substances that are highly soluble in fat (e.g., alcohol, nicotine, and anesthetic agents) to pass across the barrier.5,6 The barrier consists of fused endothelial cells on a basement membrane that is surrounded by astrocytic foot extensions.6 Substances must therefore pass through, rather than around, these cells. The blood-brain barrier is absent near the hypothalamus, pineal region, anterior third ventricle, and floor of the fourth ventricle.3 The central brain systems are the reticular activating system and the limbic system. The reticular activating system (RAS) is composed of an ascending tract and a descending tract. The ascending RAS is responsible for human consciousness level and integrates the functions of the brain stem with cortical, cerebellar, thalamic, hypothalamic, and sensory receptor functions.5 The descending RAS promotes spinal cord antigravity reflexes or extensor tone needed to maintain standing.7 The limbic system is a complex interactive system, with primary connections between the cortex, hypothalamus, amygdala, and sensory receptors. The limbic system plays a major role in memory, emotion, and visceral and motor responses involved in defense and reproduction by mediating cortical autonomic function of internal and external stimuli.8,9 The brain receives blood from the internal carotid and vertebral arteries, which are linked together by the circle of Willis, as shown in Figure 6-4. Each vessel supplies blood to a certain part of the brain (Table 6-5). The circulation of the brain is discussed in terms of a single vessel or by region (usually as the anterior or posterior circulation). There are several anastomotic systems of the cerebral vasculature that provide essential blood flow to the brain. Blood is drained from the brain through a series of venous sinuses. The superior sagittal sinus, with its associated lacunae and villi, is the primary drainage site. The superior sagittal sinus and sinuses located in the dura and scalp then drain blood into the internal jugular vein for return to the heart. TABLE 6-5 Blood Supply of the Major Areas of the Brain Data from Rumbaugh CL, Wang A, Tsai FY, editors: Cerebrovascular disease imaging and interventional treatment options, New York, 1995, Igaku-Shoin Medical Publishers; Moore KI, Dalley AF, editors: Clinically oriented anatomy, ed 4, Baltimore, 1999, Lippincott Williams & Wilkins; O’Sullivan SB, Schmitz TJ, editors: Physical rehabilitation, ed 5, Philadelphia, 2007, FA Davis. The spinal cord lies within the spinal column and extends from the foramen magnum to the first lumbar vertebra, where it forms the conus medullaris and the cauda equina and attaches to the coccyx via the filum terminale. Divided into the cervical, thoracic, and lumbar portions, it is protected by mechanisms similar to those supporting the brain. The spinal cord is composed of gray and white matter and provides the pathway for the ascending and descending tracts, as shown in cross-section in Figure 6-5 and outlined in Table 6-6. TABLE 6-6 Major Ascending and Descending White Matter Tracts* *Sensory tracts ascend from the spinal cord; motor tracts descend from the brain to the spinal cord. Data from Gilman S, Newman SW, editors: Manter and Gatz’s essentials of clinical neuroanatomy and neurophysiology, ed 7, Philadelphia, 1989, FA Davis; Marieb EN, editor: Human anatomy and physiology, ed 5, San Francisco, 2001, Benjamin-Cummings. The peripheral nervous system consists of the cranial and spinal nerves and the reflex system. The primary structures include peripheral nerves, associated ganglia, and sensory receptors. There are 12 pairs of CNs, each with a unique pathway and function (sensory, motor, mixed, or autonomic). Thirty-one pairs of spinal nerves (all mixed) exit the spinal cord to form distinct plexuses (except T2 to T12). The peripheral nerves of the trunk and the upper and lower extremities are listed in Table 6-7, and the dermatomal system is shown in Figure 6-6. The reflex system includes spinal, deep tendon, stretch, and superficial reflexes and protective responses. TABLE 6-7 Major Peripheral Nerves of the Trunk, Upper Extremity, and Lower Extremity Data from Netter FH, editor: Atlas of human anatomy, Summit City, NJ, 1989, Ciba-Geigy; Moore KL, Dalley AF, editors: Clinically oriented anatomy, ed 4, Baltimore, 1999, Lippincott Williams & Wilkins. A detailed history, initially taken by the physician, is often the most helpful information used to delineate whether a patient presents with a true neurologic event or another process (usually cardiac or metabolic in nature). The history may be presented by the patient or, more commonly, by a family member or person witnessing the acute or progressive event(s) responsible for hospital admission. One common framework for organizing questions regarding each neurologic complaint, sign, or symptom is as follows10,11: • What is the patient feeling? • When did the problem initially occur, and has it progressed? • What relieves or exacerbates the problem? • What are the onset, frequency, and duration of signs or symptoms? In addition to the general medical record review (see Chapter 2), questions relevant to a complete neurologic history include: • Does the problem involve loss of consciousness? • Did a fall precede or follow the problem? • Is there headache, dizziness, or visual disturbance? • What are the functional deficits associated with the problem? • Is there an alteration of speech? • Does the patient demonstrate memory loss or altered cognition? • Does the patient have an altered sleep pattern? • What is the handedness of the patient? (Handedness is a predictor of brain [language] dominance.) Data that can be gathered from close or distant observation of the patient include the following: • Level of alertness, arousal, distress, or the need for restraint • Head, trunk, and extremity posture, including movement patterns • Amount and quality of active movement • Amount and quality of interaction with the environment or family members • Degree of ease or difficulty with activities of daily living • Presence of involuntary movements, such as tremor • Presence of hemibody or hemispace neglect • Respiratory rate and pattern Consciousness consists of arousal and the awareness of self and environment, including the ability to interact appropriately in response to any normal stimulus.12 Coma is often considered the opposite of consciousness. Table 6-8 describes the different states of consciousness. Evaluating a patient’s level of consciousness is important because it serves as a baseline to monitor stability, improvement, or decline in the patient’s condition. It also helps to determine the severity and prognosis of neurologic insult or disease state, thus directing the medical plan of care. The Glasgow Coma Scale (GCS) is a widely accepted measure of level of consciousness and responsiveness and is described in Table 6-9. The GCS evaluates best eye opening (E), motor response (M), and verbal response (V). To determine a patient’s overall GCS, add each score (i.e., E + M + V). Scores range from 3 to 15. A score of 8 or less signifies coma.13 TABLE 6-9 Data from Teasdale G, Jennett B: Assessment of coma and impaired consciousness: a practical scale, Lancet 2:81, 1974. Cognitive testing includes the assessment of attention, orientation, memory, abstract thought, and the ability to perform calculations or construct figures. General intelligence and vocabulary are estimated with questions regarding history, geography, or current events. Table 6-10 lists typical methods of testing the components of cognition. TABLE 6-10 Data from Bickley LS, Hoekelman RA, editors: Bates’ guide to physical examination and history taking, ed 7, Philadelphia, 1999, Lippincott Williams & Wilkins. Emotional state assessment entails observation and direct questioning to ascertain a patient’s mood, affect, perception, and thought process, as well as to evaluate for behavioral changes. Evaluation of emotion is not meant to be a full psychiatric examination; however, it provides insight as to how a patient may complete the cognitive portion of the mental status examination.14 The physician should perform a speech and language assessment as soon as possible according to the patient’s level of consciousness. The main goals of this assessment are to evaluate the patient’s ability to articulate and produce voice and the presence, extent, and severity of aphasia.15 These goals are achieved by testing comprehension and repetition of spoken speech, naming, quality and quantity of conversational speech, and reading and writing abilities.15 Blood pressure, heart rate, respiratory rate and pattern (see Table 4-3), temperature, and other vital signs from invasive monitoring (see Table 18-4) are assessed continuously or hourly to determine neurologic and hemodynamic stability. Cranial nerve (CN) testing provides information about the general neurologic status of the patient and the function of the special senses. The results assist in the differential diagnosis of neurologic dysfunction and may help in determining the location of a lesion. CNs I through XII are tested on admission, daily in the hospital, or when there is a suspected change in neurologic function (Table 6-11). TABLE 6-11 Origin, Purpose, and Testing of the Cranial Nerves CN, Cranial nerve; LMN, lower motor neuron; UMN, upper motor neuron. Data from Lindsay KW, Bone I, Callander R, editors: Neurology and neurosurgery illustrated, ed 2, Edinburgh, UK, 1991, Churchill Livingstone; Marieb EN, editor: Human anatomy and physiology, ed 5, San Francisco, 2001, Benjamin-Cummings; McNeill ME, editor: Neuroanatomy primer, Baltimore, 1997, Lippincott Williams & Wilkins; O’Sullivan SB, Schmitz TJ, editors: Physical rehabilitation, ed 5, Philadelphia, 2007, FA Davis. Vision testing is an important portion of the neurologic examination because alterations in vision can indicate neurologic lesions, as illustrated in Figure 6-7. In addition to the visual field, acuity, reflexive, and ophthalmoscopic testing performed by the physician during CN assessment, the pupils are further examined for size and equality, shape, and reactivity. PERRLA is an acronym that describes pupil function: pupils equal, round, and reactive to light and accommodation. FIGURE 6-7 Visual pathway with lesion sites and resulting visual field defects. The occipital lobe has been cut away to show the medial aspect and the calcarine sulci. (From Love RJ, Webb WG, editors: Neurology for the speech-language pathologist, ed 4, Boston, 2001, Butterworth-Heinemann, p 103.) • Size and equality: Pupil size is normally 2 to 4 mm or 4 to 8 mm in diameter in the light and dark, respectively.16 The pupils should be of equal size, although up to a 1-mm difference in diameter can normally occur between the left and right pupils.17 • Shape: Pupils are normally round but may become oval or irregularly shaped with neurologic dysfunction. • Reactivity: Pupils normally constrict in response to light, as a consensual response to light shone in the opposite eye or when fixed on a near object. Conversely, pupils normally dilate in the dark. Constriction and dilation occur briskly under normal circumstances. A variety of deviations of pupil characteristics can occur. Pupil reactivity can be tested by shining a light directly into the patient’s eye. Dilated, nonreactive (fixed), malpositioned, or disconjugate pupils can signify very serious neurologic conditions (especially oculomotor compression, increased ICP, or brain herniation).17 The presence of nystagmus during the visual exam should also be noted. Nystagmus is an involuntary rhythmic movement of the eyes that may be present at rest or occur with eye or head movements.18 Nystagmus can be the result of vestibular dysfunction, a cerebellar lesion, or an imbalance in the reflex activity coordinating the two. While observing nystagmus, it is important to note the orientation (vertical versus horizontal), direction (right versus left), and head motions that increase the nystagmus. This will aid the clinician in determining the cause. Nystagmus involving the tracts/reflexes between the vestibular system and cerebellum is usually horizontal in nature and more pronounced when looking to the side of the lesion.18 Vertical nystagmus is usually present with lesions involving the anterior vermis of the cerebellum or medulla and indicates a poor prognosis for recovery. Spontaneous (at rest) nystagmus is most often observed after an acute unilateral insult to the vestibular system.7 The evaluation of motor function consists of strength, tone, and reflex testing. Strength is the force output of a contracting muscle directly related to the amount of tension that it can produce.19 Strength can be graded in the following ways in the acute care setting: • Graded 0-5/0-N (normal) with manual muscle testing • Graded as strong or weak with resisted isometrics • Graded by the portion of a range of motion in which movement occurs (e.g., hip flexion through one fourth of available range) Muscle tone has been described in a multitude of ways; however, neither a precise definition nor a quantitative measure has been determined.20 It is beyond the scope of this book to discuss the various definitions of tone, including variants such as clonus and tremor. For simplicity, muscle tone is discussed in terms of hypertonicity, hypotonicity, or dystonia. Hypertonicity, an increase in muscle contractility, includes spasticity (velocity-dependent increase in resistance to passive stretch) and rigidity (increased uniform resistance that is present throughout the whole range of motion and is independent of velocity) secondary to a neurologic lesion of the CNS or upper motor neuron system.7 Hypotonicity, a decrease in muscle contractility, includes flaccidity (diminished resistance to passive stretching and tendon reflexes)21 from a neurologic lesion of the lower motor neuron system (or as in the early stage of spinal cord injury [SCI] known as spinal shock). Dystonia, a hyperkinetic movement disorder, is characterized by disordered tone and involuntary movements involving large portions of the body resulting from a lesion in the basal ganglia (as in Parkinson’s disease with excessive L-dopa therapy).7 Regardless of the specific definition of muscle tone, clinicians agree that muscle tone may change according to a variety of factors, including stress, febrile state, pain, body position, medical status, medication, CNS arousal, and degree of volitional movement.7 Muscle tone can be evaluated qualitatively in the following ways: • Passively as mild (i.e., mild resistance to movement with quick stretch), moderate (i.e., moderate resistance to movement, even without quick stretch), or severe (i.e., resistance great enough to prevent movement of a joint)22 • Passively or actively as the ability or inability to achieve full joint range of motion • Actively as the ability to complete functional mobility and volitional movement • As abnormal decorticate (flexion) or decerebrate (extension) posturing. (Decortication is the result of a hemispheric or internal capsule lesion that results in a disruption of the corticospinal tract.17 Decerebration is the result of a brain stem lesion and is thus considered a sign of deteriorating neurologic status.17 A patient may demonstrate one or both of these postures.) Muscle tone and spasticity can also be evaluated objectively using the following scales: • Modified Ashworth Scale as described in Table 6-12. This scale has been considered the “gold standard” of measuring muscle tone due to initial studies showing high interrater (0.84) and intrarater (0.83) reliability.23 However, more recent studies have had less favorable results, showing moderate reliability.24–26 TABLE 6-12 Modified Ashworth Scale for Grading Abnormal Tone From Bohannon RW, Smith MB: Interrater reliability of a Modified Ashworth Scale of Muscle Spasticity, Phys Ther 67:206, 1987. • Modified Tardieu Scale as described in Table 6-13. The Tardieu Scale was developed by Tardieu in 195426a (the patient is in the supine position) and modified by Boyd and Graham in 199926b (the patient is in supine, sitting, or standing, depending on the joint tested). This scale measures the quality of muscle reaction to passive stretch at three different velocities. Not only is the muscle reaction quantified (as in the Modified Ashworth Scale), but it also controls for the velocity of the stretch and measures the angle at which the catch, or clonus, occurs.26b This scale has been shown in recent studies to be a more accurate measure of spasticity than the Modified Ashworth Scale.27,28 TABLE 6-13 Tardieu Scale for Grading Spasticity From Tardieu G, Shentoub S, Delarue R: A la recherché d’une technique de mesure de la spasticite. Revue Neurologique. Research on a technic for measurement of spasticity, Rev Neurol (Paris) 91:143-144, 1954. A reflex is a motor response to a sensory stimulus and is used to assess the integrity of the motor system in the conscious or unconscious patient. The reflexes most commonly tested are deep tendon reflexes (DTRs). A DTR should elicit a muscle contraction of the tendon stimulated. Table 6-14 describes DTRs according to spinal level and expected response. DTR testing should proceed in the following manner: TABLE 6-14 Deep Tendon Reflexes of the Upper and Lower Extremities 1. The patient should be sitting or supine and as relaxed as possible. 2. The joint to be tested should be in midposition to stretch the tendon. 3. The tendon is then directly tapped with a reflex hammer. Both sides should be compared. Reflexes are typically graded as present (normal, exaggerated, or depressed) or absent. Reflexes can also be graded on a scale of 0 to 4, as described in Table 6-15. Depressed reflexes signify lower motor neuron disease or neuropathy. Exaggerated reflexes signify upper motor neuron disease, or they may be due to hyperthyroidism, electrolyte imbalance, or other metabolic abnormalities.29 TABLE 6-15 Deep Tendon Reflex Grades and Interpretation Data from Bickley LS, Hoekelman RA: Bates’ guide to physical examination and history taking, ed 7, Philadelphia, 1999, Lippincott Williams & Wilkins. The most commonly tested cutaneous reflex is the Babinski sign. A positive (abnormal) Babinski sign is great-toe extension with splaying of the toes in response to stroking the lateral plantar surface of the foot with the opposite end of a reflex hammer. It indicates corticospinal tract damage, as seen in spinal cord injury, stroke, and multiple sclerosis.30 Sensation testing evaluates the ability to sense light touch, proprioception, pressure, temperature, vibration sense, and pain. For each modality, the face, neck, trunk, and extremities are tested bilaterally, proceeding in a dermatomal pattern (see Figure 6-6). For more reliable sensation testing results, the patient should be asked to close his or her eyes or look away from the area being tested. Table 6-16 outlines the method of sensation testing by stimulus. TABLE 6-16 Data from Lindsay KW, Bone I, Callander R, editors: Neurology and neurosurgery illustrated, ed 2, Edinburgh, UK, 1991, Churchill Livingstone; Gilman S, Newman SW, editors: Manter and Gatz’s essentials of clinical neuroanatomy and neurophysiology, ed 7, Philadelphia, 1989, FA Davis; Hickey JV, editor: The clinical practice of neurological and neurosurgical nursing ed 4, Philadelphia, 1997, Lippincott.
Nervous System
Preferred Practice Patterns
Body Structure and Function of the Nervous System
Central Nervous System
Brain
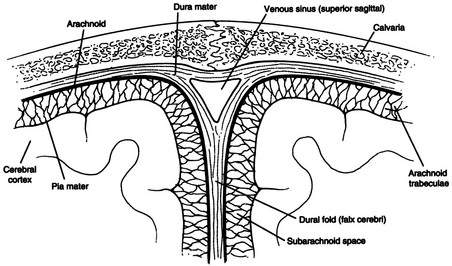
Protective Mechanisms.
Cranium.
Meninges.
Falx cerebri
Vertical fold that separates the two cerebral hemispheres to prevent horizontal displacement of these structures
Falx cerebelli
Vertical fold that separates the two cerebellar hemispheres to prevent horizontal displacement of these structures
Tentorium cerebelli
Horizontal fold that separates occipital lobes from the cerebellum to prevent vertical displacement of these structures
Diaphragm sellae
Horizontal fold that separates the subarachnoid space from the sella turcica and is perforated by the stalk of the pituitary gland
Epidural (extradural) space
Potential space between the skull and outer dura mater
Subdural space
Potential space between the dura and the arachnoid mater; a split in the dura contains the venous sinus
Subarachnoid space
Anatomic space between the arachnoid and pia mater containing cerebrospinal fluid and the vascular supply of the cortex
Ventricular System.
Blood-Brain Barrier.
Central Brain Systems.
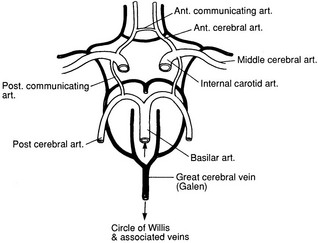
Circulation.
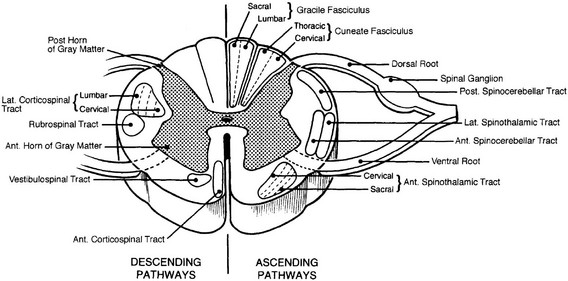
Spinal Cord
Tract
Function
Fasciculus gracilis
Sensory pathway for lower-extremity and lower-trunk joint proprioception, vibration, two-point discrimination, graphesthesia, and double simultaneous stimulation
Fasciculus cuneatus
Sensory pathway for upper-extremity, upper-trunk, and neck joint proprioception, vibration, two-point discrimination, graphesthesia, and double simultaneous stimulation
Lateral spinothalamic
Sensory pathway for pain, temperature, and light touch
Ventral spinocerebellar
Sensory pathway for ipsilateral subconscious proprioception
Dorsal spinocerebellar
Sensory pathway for ipsilateral and contralateral subconscious proprioception
Lateral corticospinal (pyramidal)
Motor pathway for contralateral voluntary fine-muscle movement
Anterior corticospinal (pyramidal)
Motor pathway for ipsilateral voluntary movement
Rubrospinal (extrapyramidal)
Motor pathway for gross postural tone
Tectospinal (extrapyramidal)
Motor pathway for contralateral gross postural muscle tone associated with auditory and visual stimuli
Vestibulospinal (extrapyramidal)
Motor pathway for ipsilateral gross postural adjustments associated with head movements
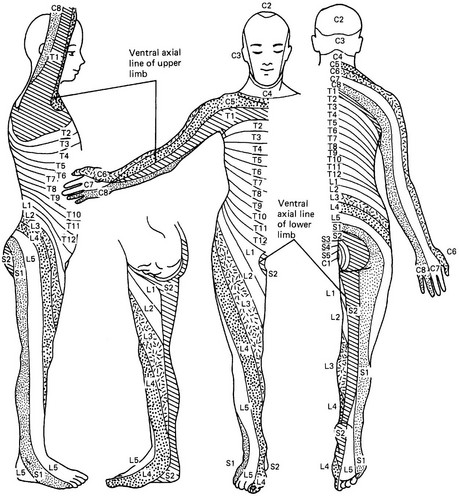
Peripheral Nervous System
Neurologic Examination
Patient History
Observation
Mental Status Examination
Level of Consciousness
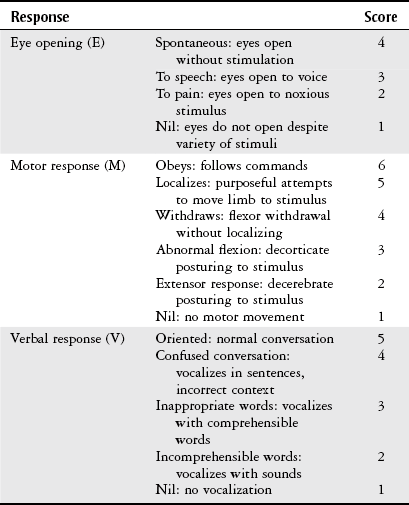
Glasgow Coma Scale.
Cognition
Cognitive Function
Definition
Task
Attention
Ability to attend to a specific stimulus or task
Repetition of a series of numbers or letters
Spelling words forward and backward
Orientation
Ability to orient to person, place, and time
Identify name, age, current date and season, birth date, present location, town, etc.
Memory
Immediate recall
Short-term memory
Long-term memory
Recount three words after a few seconds
Recount words (after a few minutes) or recent events
Recount past events
Calculation
Ability to perform verbal or written mathematical problems
Add, subtract, multiply, or divide whole numbers
Construction
Ability to construct a two- or three-dimensional figure or shape
Draw a figure after a verbal command or reproduce a figure from a picture
Abstraction
Ability to reason in an abstract rather than a literal or concrete fashion
Interpret proverbs
Discuss how two objects are similar or different
Judgment
Ability to reason (according to age and lifestyle)
Demonstrate common sense and safety
Emotional State
Speech and Language Ability
Vital Signs
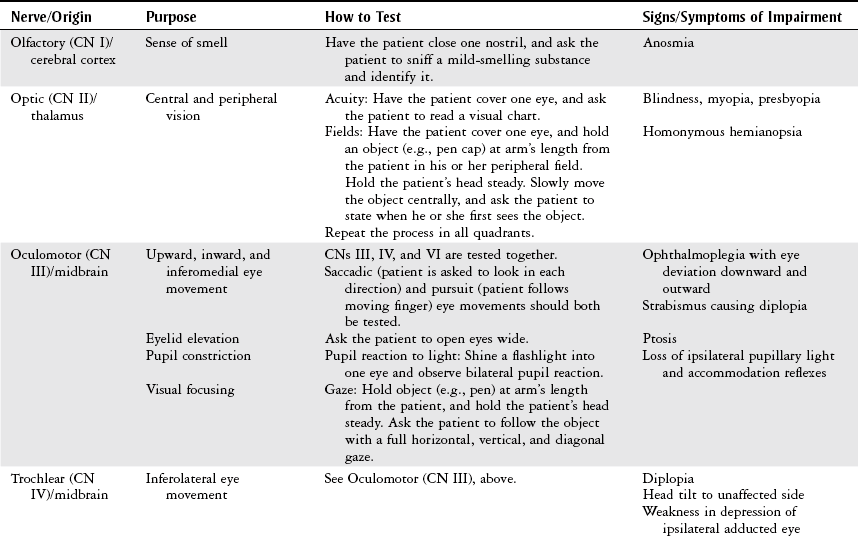
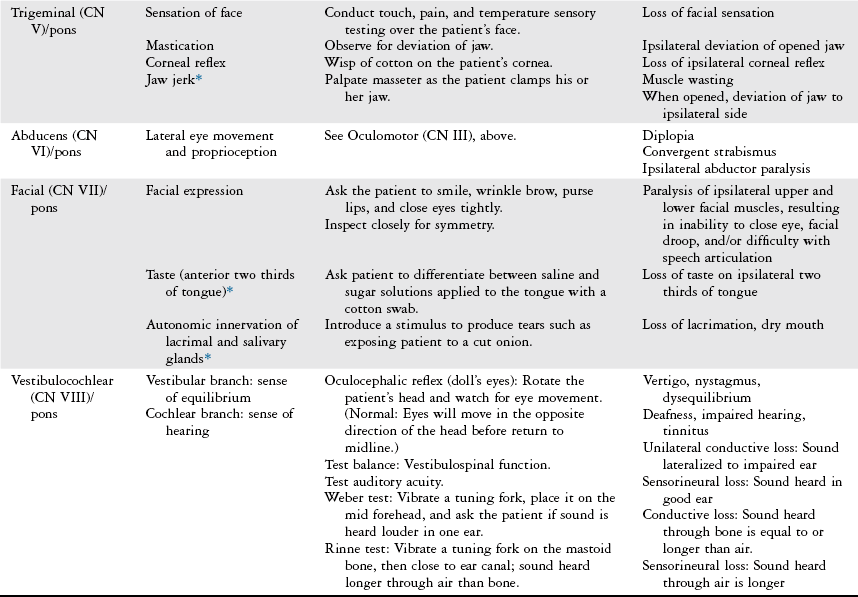
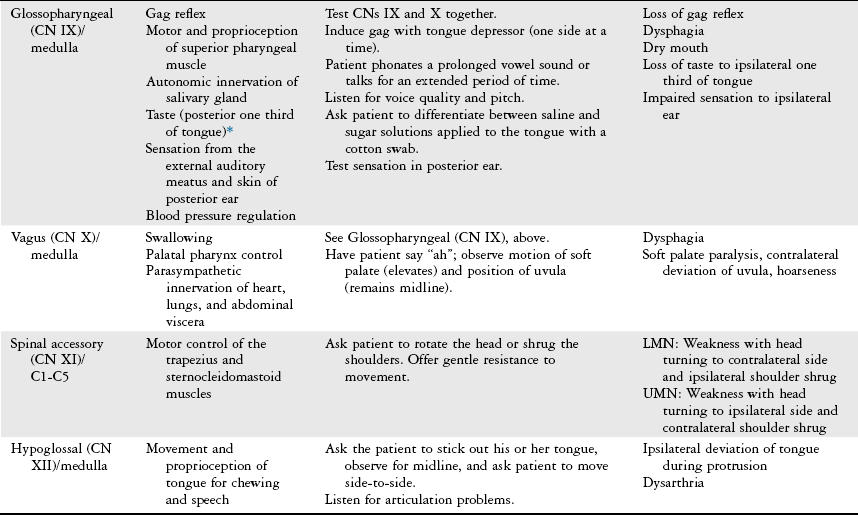
Cranial Nerves
Vision
Motor Function
Strength Testing
Muscle Tone
Grade
Description
0
No increase in muscle tone.
1
Slight increase in muscle tone, manifested by a slight catch and release or by minimal resistance at the end of the range of motion when the affected part(s) is moved in flexion or extension.
1+
Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the range of motion.
2
More marked increased in muscle tone through most of the range of motion, but affected part(s) easily moved.
3
Considerable increase in muscle tone; passive movement difficult.
4
Affected part(s) rigid in flexion and extension.
Grade
Description
0
No resistance throughout the course of movement.
1
Slight resistance throughout the course of movement, but no clear catch.
2
Clear catch at a precise angle, interrupting the movement, followed by release.
3
Fatigable clonus with less than 10 seconds when maintaining the pressure and appearing at a precise angle.
4
Unfatigable clonus with more than 10 seconds when maintaining the pressure and appearing at a precise angle.
5
Joint is immovable.
Reflexes
Reflex
Spinal Level
Normal Response
Biceps
C5
Elbow flexion
Brachioradialis
C6
Elbow flexion
Triceps
C7
Elbow extension
Patellar
L4
Knee extension
Posterior tibialis
L5
Plantar flexion and inversion
Achilles
S1
Plantar flexion
Grade
Response
Interpretation
0
No response
Abnormal
1+
Diminished or sluggish response
Low normal
2+
Active response
Normal
3+
Brisk response
High normal
4+
Very brisk response, with or without clonus
Abnormal
Sensation
Sensation
Modality and Method
Light touch
Apply light touch with the finger, a cotton ball, or washcloth over the extremities or trunk. The patient is asked to identify if there is a stimulus present and the location of the stimulus.
Pain
Touch a pin or pen cap over the extremities or trunk. Ask the patient to distinguish between dull (pen cap) and sharp (the pin) stimuli.
Pressure
Using the therapist’s fingertip, apply pressure on the skin surface that is firm enough to indent the skin and stimulate the deep receptors. The patient is asked to identify if there is a stimulus present.
Proprioception
Lightly grasp the distal interphalangeal joint of the patient’s finger or great toe, and move the joint slowly up and down. Ask the patient to state in which direction the joint is moved. Test distal to proximal (e.g., toe to ankle to knee).
Vibration
Activate a tuning fork and place on a bony prominence. Ask the patient to state when the vibration slows and stops. Proceed distal to proximal.
Temperature
Place test tubes filled with warm or cold water on the area of the patient’s body to be tested. Ask the patient to state the temperature. (Rarely done in the acute care setting.)
Stereognosis
Place a familiar object in the patient’s hand and ask the patient to identify it.
Two-point discrimination
Place two-point caliper or drafting compass on area to be tested. Ask the patient to distinguish whether it has one or two points.
Graphesthesia
Trace a letter or number in the patient’s open palm and ask the patient to state what was drawn.
Double simultaneous stimulation
Simultaneously touch two areas on the same side of the patient’s body. Ask patient to locate and distinguish both points.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nervous System
Only gold members can continue reading. Log In or Register to continue