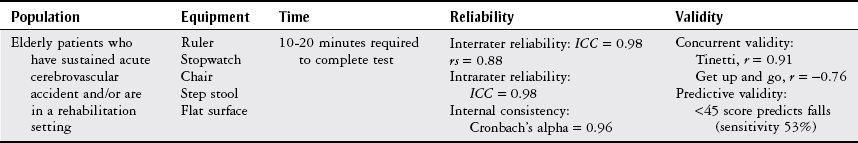
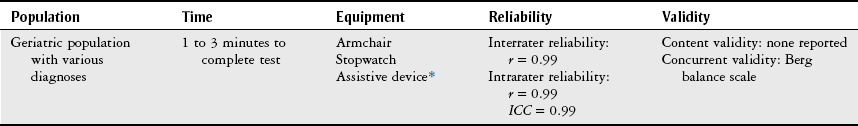
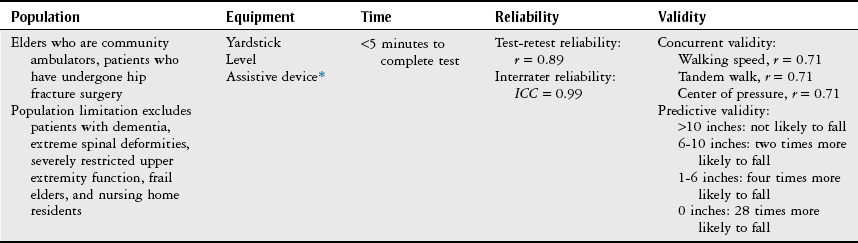
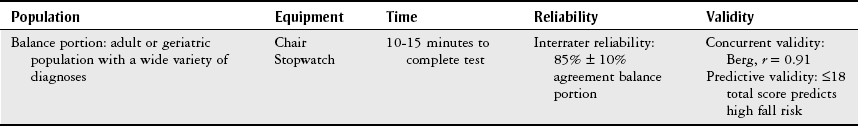
Chapter 23 These functional tests and outcome measures apply to many body systems. For this reason, specific practice patterns are not delineated in this chapter. Please refer to Appendix A for a complete list of the preferred practice patterns in order to best delineate the most applicable practice pattern for a given patient. The functional tests presented in this chapter were selected because of their ease of use, reliable and valid test results, and the appropriate population in the acute care setting. Where applicable, interrater (tested by different therapists) and intrarater (retested over time by a single therapist) reliability3 and content,* construct,† and predictive‡ validity will be noted in the respective description of each test.3 The Berg Balance Scale (BBS) is a 56-point scale that evaluates 14 tasks. Katherine Berg developed this test to assess the level of function and balance in various patient populations.4 Table 23-1 describes the appropriate population, required equipment, completion time, reliability, and validity of the BBS. TABLE 23-1 Overview of the Berg Balance Scale Data from Thorbahn L, Newton R: Use of the Berg Balance Test to predict falls in elderly persons, Phys Ther 76(6):576-583, 1996; Conradsson M, Lundin-Olsson L, Lindelof N et al: Berg Balance Scale: intrarater test-retest reliability among older people dependent in activities of daily living and living in residential care facilities, Phys Ther 87:1155-1163, 2007; Thompson M, Medley A: Performance of community dwelling elderly on the timed up and go test, Phys Occup Ther Geriatr 13(3):17-30, 1995; Whitney S, Poole J, Cass S: A review of balance instruments for older adults, Am J Occup Ther 52(8):666-671, 1998; Berg K, Wood-Dauphinee S, Williams JI, et al: Measuring balance in the elderly: preliminary development of an instrument, Physiother Can 41:304, 1989. The patient is evaluated and graded on a sequence of balance activities, such as sitting unsupported with arms folded, rising, standing, transferring between one surface and another, reaching forward in standing, picking up objects off the floor, turning around in a full circle, and standing on one leg.4 Scoring for each task ranges from 0 to 4. A score of 0 indicates that the patient is unable to complete a particular task. A score of 4 indicates that the patient can completely carry out the task.4 The 14 tasks consist of6: • Reaching forward with an outstretched arm • Retrieving object from floor • Placing alternate foot on stool • Standing with one foot in front of the other foot A short form of the BBS has been developed and demonstrates psychometric test properties similar to those of the original BBS. The short form of the BBS includes 7 activities rather than 14, and the scoring levels are reduced to three (0, 2, 4). This modified BBS has been shown to have good validity and reliability in patients who have had a cerebrovascular accident (CVA).6 Box 23-1 outlines the seven items on this modified BBS. Higher scores on the BBS indicate greater independence and better ability to balance.7 In contrast, lower scores indicate a greater fall risk. Prior evidence suggested that a total score of less than 45 predicted that the patient is at risk for falls.8,9 However, more recent literature by Katherine Berg discourages the use the score as a dichotomous scale (i.e., determining fall risk based on values being greater than or less than 45 points).10 Rather, the score should be used to represent a continuum of balance, through the use of likelihood ratios.10 The “up and go” test was originally developed in 1986 to serve as a clinical measure of balance in elderly people.12 The original test used a numeric scoring system to determine a patient’s level of balance but was later modified to a timed version by Posiadlo and Richardson in 1991.13 The TUG test uses a time score to assess gait and balance in the elderly population and is summarized in Table 23-2.14 TABLE 23-2 Overview of the Timed “Up and Go” Test ICC, Intraclass correlation coefficient; r, correlation coefficient. *If necessary, an assistive device may be used while performing this test. Data from Whitney S, Poole J, Cass S: A review of balance instruments for older adults, Am J Occup Ther 52(8):666-671, 1998; Posiadlo D, Richardson S: The timed “up and go”: a test of basic functional mobility for frail elderly persons, J Am Geriatr Soc 39:142-148, 1991; Berg KO, Wood-Dauphinee SL, Williams JI et al: Measuring balance in the elderly: validation of an instrument, Can J Public Health 83:S7-S11, 1992; Portney LG, Watkins MP, editors: Foundations of clinical research applications to practice, Norwalk, CT, 1993, Appleton & Lange. The patient is timed during a five-part mobility task from start to finish. The task consists of the following15: Test completion in fewer than 20 seconds indicates that the patient is independent with functional mobility.15 The time needed to complete the test may improve for many reasons, including: (1) altering the use of an assistive device, (2) actual change in function, and (3) increased familiarity of the test, or a combination of these. Therefore it is important to periodically perform this test over the course of a patient’s physical therapy intervention to allow for comparison to baseline results. As described in Table 23-2, when compared to other functional tests (i.e., BBS), with regard to balance testing, the TUG test is a consistent test of the balance characteristics in this population. The ability or inability to complete the TUG test helps to stratify patients according to their fall risk. Patients who are unable to complete the TUG test for nonphysical reasons (including refusal or inability to follow instructions [e.g., dementia or delirium]) appear to have higher rates of falling as compared to patients who are unable to do the TUG test for physical reasons (inability to sit, stand, or walk independently, or with standby assistance).16 Additionally, patients who have undergone hip fracture surgery and are discharged from the acute care setting with a TUG score of 24 seconds or more are more likely to fall in the next 6 months than are patients with scores of less than 24 seconds.17 When used in an acute care setting, this test can objectively demonstrate improvements in balance and ambulation. Over the course of therapy, it is expected that the time the patient takes to complete the TUG test will decrease as the patient improves.14 The functional reach test was developed to assess the risk for falls in the elderly population and is a dynamic measure of stability during a self-initiated movement.19 The functional reach test evaluates balance by measuring the maximum distance an elderly person can reach forward, backward, and out to the side while standing on the floor at a fixed position (Table 23-3).7 TABLE 23-3 Overview of the Functional Reach Test ICC, Intraclass correlation coefficient; r, correlation coefficient. *An assistive device may be used while performing this test if it is necessary. Data from Thapa PB, Gideon P, Fought RL et al: Comparison of clinical and biomechanical measures of balance and mobility in elderly nursing home residents, J Am Geriatr Soc 42:493-500, 1994; Portney LG, Watkins MP, editors: Foundations of clinical research applications to practice, Norwalk, CT, 1993, Appleton & Lange, p 689; Sherrington C, Lord SR: Reliability of simple portable tests of physical performance in older people after hip fracture, Clin Rehabil 19:496-504, 2005. The procedure involves a series of three trials of the distance a patient is willing to reach from a fixed surface.7 After every reach, distance is measured with a yardstick attached to the wall at shoulder level. The difference in inches between a person’s arm length and maximal forward, backward, and sideward reach with the shoulder flexed to 90 degrees while maintaining a fixed base of support in standing is then recorded.12,20 The mean of three trials is the score. The functional reach in inches correlates with the patient’s relative risk for falling (Table 23-4).19 TABLE 23-4 Data from Duncan PW, Weiner DK, Chandler J, et al: Functional reach: a new clinical measure of balance, J Gerontol 45:M192-M197, 1990. The Tinetti Performance Oriented Mobility Assessment (POMA) is a performance test of balance and gait maneuvers used during normal daily activities.22 This test has two subscales of balance and gait, as described in Table 23-5. There are 13 maneuvers in the balance portion and 9 maneuvers in the gait portion. The balance subscale, the performance oriented assessment of balance (POAB), can be used individually as a separate test of balance. TABLE 23-5 Overview of the Tinetti Performance Oriented Mobility Assessment Data from King MB, Judge JO, Whipple L et al: Reliability and responsiveness of two physical performance measures examined of a functional training intervention, Phys Ther 80(1):8-16, 2000; Tinetti M: Performance oriented assessment of mobility problems in elderly patients, J Am Geriatr Soc 41:479, 1986; Nakamura DM, Holm MB, Wilson A: Measures of balance and fear of falling in the elderly: a review, Phys Occup Ther Geriatr 15(4):17-32, 1998; Wee JYM, Bagg SD, Palepu A: The Berg Balance Scale as a predictor of length of stay and discharge destination in an acute stroke rehabilitation setting, Arch Phys Med Rehabil 80(4):448-452, 1999; Anemaet W, Moffa-Trotter M: Functional tools for assessing balance and gait impairments, Top Geriatr Rehabil 15(1):66-83, 1999.
Functional Tests
Preferred Practice Patterns
Berg Balance Scale
Procedure
Interpretation of Results
Timed “Up and Go” Test
Procedure
Interpretation of Results
Functional Reach Test
Procedure
Interpretation of Results
Reach
Likelihood of Falling
>10 inches
Not likely
6-10 inches
2 times more likely
1-6 inches
4 times more likely
Subject unwilling to reach
28 times more likely
Tinetti Performance Oriented Mobility Assessment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







