Fig. 7.1
(a) A bur is used to outline the location of bone block on mandibular buccal cortex by a distance from the inferior border of mandible and alveolar crest.The mesial incision should be made in 3-4 mm away from the mental foramen (2 sided arrow). (b) Then the buccal bone surrounding the canal is removed carefully by reciprocal motion using an osteotome
2.
Nerve transpositioning: In cases where the edentulous area and ridge resorption include the premolar teeth, there is a need for transpositioning of the mental neurovascular bundle and transection of the incisive nerve with transposing of the nerve distally (associated with mental nerve and mental foramen involvement). This method has been called IAN distalization in some studies [2, 11–13] (Fig. 7.2). Another method that has been suggested is drilling the bone surrounding the canal using a handpiece and a round bur. In this technique, while the nerve is protected, minimum amount of bone is removed from the buccal cortex and the maximum amount of bone is preserved in an atrophic ridge for implant placement that results in maximum primary stability of the implant. Also, mandibular bone weakening is minimized in this method that is a great advantage of this technique. This instrument has been designed, patented, and manufactured by the author (Hassani nerve protector).
Fig. 7.2
Inferior alveolar nerve transpositioning (distalization). Different techniques of ostectomy. (a) A bur is used to outline the bone block area. An osteotome (chisel) is used to remove the bone block. (This technique that is usually performed for treatments other than dental implants) (b) The spongy bone is removed using a curette. In this technique, the preparation design includes the surroundings of the mental foramen. While keeping an adequate distance from mental foramen a circle is drawn with the center being the foramen using a round bur and the cortical bone is resected (c) In groove technique, while the nerve is protected by IAN protector, minimum amount of bone is removed from the buccal cortex by drilling the bone surrounding the canal using a handpiece and a round bur
7.3 Patient Selection and Keys of Reducing Nerve Damage
Generally, IAN repositioning is used for different treatment goals. It is used for implant placement in the atrophic posterior mandibular alveolar ridge [1, 2, 10–13], orthognatic surgery [7], pain reduction in the atrophic ridge caused by a dental prosthesis pressure on the mental foramen [15, 17, 18], treatment of pathologic lesions of the posterior of mandible [19, 20], and transoral access to the IAN for microsurgery or nerve grafting [21].
In this surgery, as in other surgical operations, the process of selecting the appropriate patient is the key to a successful treatment. The more eligible for surgery the selected patient is, the less postsurgical complications there will be. As the most important complication of this surgery relates to neurosensory deficit, selecting the right patient will help to minimize this problem with adequate informed consent.
7.3.1 Clinical and Radiographic Evaluation
For clinical assessment of a patient who is a candidate for dental implants and suffers from a reduced mandibular alveolar ridge height, first study casts should be prepared and then the occlusal relationship should be evaluated and recorded. The following points should also be considered:
1.
The area of the edentulous atrophic alveolar ridge:
If the edentulous area extends anteriorly to the canine region, the surgeon should consider the need for mental nerve transpositioning [12].
In edentulous patients, the absence of incisor sensation following nerve distalization does not cause problems, but in patients with mandibular incisor teeth this can result in an unpleasant sensation in the anterior segment that is usually described as a sense of dullness in these teeth [7].
2.
The distance between the occlusal surface of maxillary teeth and mandibular alveolar ridge:
In some cases, despite alveolar ridge resorption there is not enough clearance between the occlusal surfaces of the maxillary teeth and mandibular ridge that is required for constructing the implant prosthesis. This is usually due to the patient’s preexisting occlusion (mainly in deep bite cases) or super-eruption of the corresponding maxillary posterior teeth. Vertical augmentation methods often cannot be used due to the restricted inter-occlusal space (Fig. 7.3). In such cases, the only available option seems to be nerve repositioning [22, 23].


Fig. 7.3
Lack of adequate space for vertical augmentation
3.
Evaluation of the relationship between the mandibular alveolar ridge and maxillary alveolar ridge in the horizontal plane: The necessity of lateral augmentation simultaneous with nerve repositioning or vertical augmentation should also be evaluated by clinical examination and dental cast analysis.
4.
Radiographic evaluation: Every patient who is a candidate for nerve repositioning is required to obtain panoramic radiography and consideration should be given toward a CBCT scan.
The amount of bone above the IAC, other anomalies, the distance of the IAC from the buccal cortex, and the thickness of the cortex for ostectomy are all evaluated on panoramic radiography. Exact location and precise anatomy of the mental foramen and anterior loop may also be evaluated [24].
In rare cases, the IAC may be completely attached to the medial or lateral cortex as evidenced on CBCT. In such cases, implants may be placed buccal or lingual to the IAC with no need for nerve repositioning surgery. Additionally, by analysis and reconstruction of scanned images using CAD-CAM, it is feasible to determine the entire path of the IAC and place the implants in atrophic areas with caution.
7.3.2 Indications, Contraindications, and Limitations
Babbush mentioned several indications for nerve repositioning including the following: placement of removable prosthetics, stabilizing the remaining anterior teeth, stabilizing the TMJ, and establishing muscular balance following reconstruction of the dentoalveolar system. He also discussed some related limitations, primarily that this procedure is technically difficult and requires adequate expertise. The surgeon should have advanced surgical experience with this technique, as well as sufficient anatomic knowledge and necessary skills to fully manage perioperative and postoperative complications if they occur. According to Babbush, the most significant risk of surgery is nerve injury due to surgical manipulation of the IAN as a result of the surgical procedure itself. Although rare, mandibular fracture should also be considered as a risk, especially in cases with severe mandibular atrophy [25] (Fig. 7.4).


Fig. 7.4
Mandibular fracture in a patient with severe mandibular atrophy following nerve repositioning
Rosenquist et al. in their studies on the nerve repositioning procedure mentioned the following indications and contraindications for this operation:
Indications
1.
Less than 10–11-mm bone height above the IAC.
2.
When the quality of the spongy bone does not provide sufficient stability for implant placement.
7.3.3 Preoperative Consultation
Before choosing nerve repositioning, the required criteria must be assessed. According to the literature, 100 % of patients who undergo nerve repositioning develop various degrees of sensory nerve dysfunction of the IAN sensory distribution [1, 27–29]. Therefore, the patient and family members should be well informed relevant to the phases of treatment, duration of surgery, and postoperative general complications, and most importantly they should be provided with knowledge about the postoperative lower lip and chin (and possibly lower incisor) paresthesia which will definitely occur and may last for up to 6 months, and in some cases, if it lasts longer or is very severe, it may require microneurosurgical exploration and repair [1, 27, 29–31].
Despite the issues mentioned above, the patient may not fully comprehend the sensation of paresthesia, and in such cases, it is recommended to perform an IAN anesthetic block for the patient using bupivacaine for long-lasting anesthesia induction so that the patient can experience anesthesia and paresthesia for up to 8–12 h. The advantages of this treatment modality should also be explained to the patient including shorter treatment duration, no need for autogenous bone grafting and no donor site morbidity, minimum use of other bone replacement materials, and avoiding the need for additional surgeries [1, 2, 7, 27, 29].
7.3.4 Important Considerations in Nerve Repositioning Surgery
1.
Patient selection: The surgical process is complicated and occurrence of sensory disturbances is inevitable. Therefore, the surgeon should evaluate the patient’s general mental condition, since some patients are under stress and oversensitive even toward the smallest surgical complications. Such patients do not have the tolerance and compatibility skills and therefore are not good candidates for nerve repositioning surgery.
2.
Informed consent: The surgeon must provide data to the patient regarding all of the phases of surgery as well as the probable and possible complications. A thorough explanation should be provided for the patient in an understandable and comprehensible manner regarding surgical and neural complications. The sense of anesthesia that may occur should be well described for the patient, and it also should be mentioned that the anesthesia may be permanent and irreversible.
3.
Imaging: While in the past, panoramic radiography was sufficient for evaluation, presently CBCT, when available, should be considered for the precise evaluation of IAC position and surrounding bone thickness.
4.
Perioperative medications: Dexamethasone should be administered before the surgery in order to help decrease perineurial edema following nerve manipulation.
5.
Regional anatomy: The surgeon must have a full knowledge regarding local and regional anatomy of the mandible, as well as a working knowledge of the pathophysiology of nerve injuries, and be able to evaluate and follow the clinical course of nerve dysfunction after the surgery and make an appropriate referral to a microneurosurgeon or neurologist, if indicated.
6.
Surgeon experience: The surgeon’s skill and expertise are very important and consideration should be given toward the use of operating magnification with the use of magnification loops.
7.
Armamentarium: Delicate microsurgery instruments are required for this type of surgery and should be available. Also, the surgeon should have the knowledge, skills, and experience for repairing the nerve in case of IAN transection or severe axonal injury sustained during the nerve repositioning procedure.
8.
Anatomic variations: In cases where the IAC is located in the center of the mandible buccolingually or in a lingual position based upon CBCT, the surgeon should expect a more complex surgery and the risk of neurosensory complications is increased due to the more extensive surgical manipulation of the IAN.
9.
Posterior access: In cases where the nerve repositioning surgery extends further posteriorly and involves the first or second molar area for implant placement, the surgery can be more complicated due to the thicker cortical bone and limited access to this area.
10.
Adjunctive therapies: Following nerve repositioning surgery, sensory reeducation exercises should be used to augment spontaneous neurosensory recovery of the IAN. In addition, the use of low-level laser after surgery reduces perineurial inflammation and has been shown to improve spontaneous neurosensory recovery.
11.
Postoperative medications: Antibiotic therapy and administration of analgesics and NSAIDs postoperatively are similar to that following routine implant surgery, and there are no specific recommendations in this regard in the literature. Antibiotic and corticosteroid prophylaxis is recommended because of the extensiveness and duration of surgery. As mentioned, the use of corticosteroids pre- and postoperatively helps to decrease the symptoms of perineurial edema. However, there is no consensus in this regard, but since inflammation can be among the causes of nerve dysfunction, corticosteroid therapy can be beneficial.
7.4 Mechanism of Nerve Injury
IAN damage during the various stages of the nerve repositioning operation is possible. Generally nerve damage processes can be classified to five categories:
1.
Flap design
2.
Ostectomy to access the IAC
3.
Repositioning the neurovascular bundle outside of the IAC
4.
Nerve damage during IAN retraction from the canal for drilling and implant insertion
5.
Repositioning the neurovascular bundle inside the canal
7.4.1 Flap Design
The incision is made on alveolar crest starting from the anterior border of the ramus forward. At the mesial surface of the mandibular canine, a releasing incision is made anteriorly and toward the vestibular sulcus in order to avoid injuring mental nerve branches. If the anterior-releasing incision is not made at the mesial of the canine, there is a chance of injuring the mental nerve branches present in the vestibular soft tissues [12, 28, 29, 32]. When retracting the mucoperiosteal flap, the mental foramen is completely exposed and the dissection is extended toward the inferior border of the mandible. Considering the radiographic and CBCT evaluations along with the fact that the IAC is usually located 2 mm below the mental foramen, it is necessary to expose the lateral surface of the body of the mandible and release the periosteum around the mental nerve [6, 12, 17] (Figs. 7.5 and 7.6).
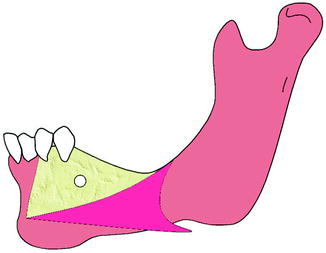
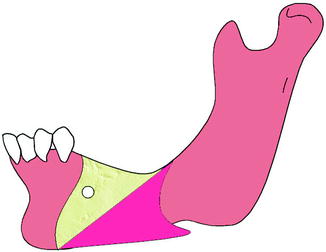
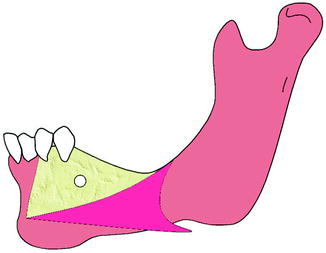
Fig. 7.5
Correct flap design: an incision is made on the alveolar crest with a releasing incision at the mesial of the mandibular canine
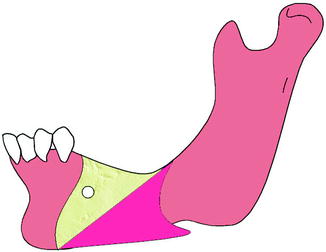
Fig. 7.6
Incorrect flap design: if the anterior-releasing incision is not made at the mesial of the canine, there is a chance of injuring the terminal mental nerve branches present in the vestibular soft tissues
The MN lies in the mandibular buccal soft tissues and is at risk of injury during the incision(s). Recognition of the changing anatomy of the edentulous mandible is particularly helpful in minimizing the risk of injury to the MN. As the patient ages, the alveolar bone in an edentulous area resorbs, and the position of the mental foramen becomes closer to the crest of the alveolar ridge. In some patients there is an actual dehiscence of the IAC, and the IAN and the MN come to lie on the alveolar ridge crest. Placement of an incision must, therefore, take these anatomic changes into consideration. During the retraction of the mucoperiosteal flap, it is possible to exert continuous undue pressure on the underlying MN with resultant neuropraxic (Sunderland grade I) injury. Gentle soft tissue retraction with frequent brief relaxations of retraction pressure is suggested [33].
7.4.2 Ostectomy to Access the IAC
Nerve injury is most likely to happen when performing the ostectomy to expose the IAC. According to the existing research, the technique of performing the ostectomy is effective in reducing postsurgical complications. There are two general techniques to accomplish this portion of the surgery.
In the first technique, which is usually performed for treatments other than dental implants, a piece of bone is removed as a block and then the IAC is exposed. This method can be indicated for simultaneous implant surgery where there is adequate bone height over the canal. In such cases, even after resecting a bone block, a sufficient amount of bone still remains at the lateral side of implant [7]. In the second technique, the ostectomy is performed with the “groove ostectomy” method, since more bone will be saved and primary implant stability will also be improved. These techniques can be modified to accomplish either nerve lateralization or transpositioning.
7.4.2.1 Nerve Lateralization
Method of removing bone block without the involvement of mental foramen: In this technique, a bur is used to outline the location of the bone block on the mandibular buccal cortex by a distance from the inferior border of the mandible and alveolar crest. The anterior border of the ostectomy should be made in 3–4 mm anterior to the mental foramen. It is worth mentioning that maintaining a 3–4-mm distance from the distal side of the mental foramen will also help to reduce the postsurgical neurosensory problems. Generally, more involvement between the mental nerve and the mental foramen during the surgery will increase the risk of neurosensory symptoms [11, 25] (Fig. 7.7a).
7.4.2.2 Nerve Transpositioning
Removal of bone block with mental foramen involvement: Similar to the previous method, a bur is used to outline the bone block area. An osteotome (chisel) is used to remove the bone block and the spongy bone is removed using a curette. In this technique, the preparation design includes the surroundings of the mental foramen. While keeping an adequate distance from the mental foramen, a circle is drawn with the center as the mental foramen using a round bur, and then the cortical bone is resected. This results in two bone blocks: one posterior to the mental foramen and the other one around the mental foramen through which the nerve has traversed. This mesial segment, with the nerve passing through it, is put aside with great caution, and when the operation is completed, it is returned to its original location. This technique is indicated when the edentulous atrophic area has extended to involve the premolar area, and there is a need for replacing the lost premolar teeth. This method may require incisive nerve transection in order to achieve improved nerve mobility from the IAC or when the planned implant is anterior to the mental foramen in the area of the incisive nerve. This method is also called nerve distalization [1–3, 7, 12] (Fig. 7.7b).
Groove ostectomy technique: Another method that has been described is drilling the bone surrounding the canal using a handpiece and a round bur. The surgeon carefully enters a probe (round end with no sharp edges) into the IAC through the mental foramen and determines the distal path of the IAC. Then, according to this test and after evaluating the canal path on the radiographs, the surgeon inserts the tip of the nerve protector into the canal. This instrument should be placed in between the nerve and the bone in order to protect the IAN. The buccal bone is drilled using a bur. By directing the bur distally, the nerve protector is also moved distally in between the nerve and bone to protect the nerve. The bone chips are collected by a bone collection device (suction trap) during this process. In this technique, while the IAN is protected, a minimum amount of bone is removed from the buccal cortex and the maximum amount of bone is preserved in an atrophic ridge for implant placement that results in maximum primary stability of the implant. Also, mandibular bone weakening is minimal in this method that is a great advantage of this technique to decrease the chance of mandibular fracture. This instrument has been designed, patented, and manufactured by the author (Hassani nerve protector) (Fig. 7.7c, d).
In patients with an atrophic alveolar ridge involving the premolar area or those with an edentulous mandibular ridge with alveolar crest atrophy who need implant placement and nerve transpositioning in the posterior mandible, mental nerve transpositioning is also necessary most of the time. This transpositioning is usually associated with incisive nerve transection (Fig. 7.7e). In such cases, the patients will not have any problems related to incisive nerve transection, but in cases where the patient has vital anterior mandibular teeth, incisive nerve transection may result in an unpleasant sensation in these incisor teeth. In some cases, root canal therapy may be required. However, several studies have reported that no problems related to anterior mandibular teeth were seen [1, 2, 12, 27, 29, 32]. Sectioning of the incisive branch of the IAN, and releasing the neurovascular bundle and moving it posterior in order to avoid traction is called nerve distalization [2]. It should be noted that in many cases it is possible to transpose the mental nerve without sectioning the incisive branch.
In the method of nerve repositioning without releasing the mental nerve, a great traction force is exerted on the nerve when holding it outside of the surgical implant site. According to the literature, the highest number of nerve injuries occurs during the anterior ostectomy because the nerve trunk becomes thinner at mental foramen and is therefore more susceptible to injury. This is the reason that nerve repositioning without involving the mental foramen has the least neurosensory complications and side effects. According to the literature, by preserving 3–4 mm of bone distal to the mental foramen during nerve repositioning, IAN damage can be reduced because the nerve is thinner and more susceptible to injury at this specific location [11, 29].
During ostectomy care must be taken not to injure the nerve with rotary instruments, curettes, or elevators. When removing the bone cortex over the nerve, it is recommended to use the nerve protector designed specifically for this purpose; it fits within the IAC lateral to the IAN. Direct contact of rotary or other surgical instruments with the nerve is among the most serious injuries in this type of surgery; a round diamond bur may be used to decrease the incidence of neural trauma as opposed to a round carbide bur if there is direct contact with the IAN.
Fig. 7.7
(a) Nerve lateralization. The anterior border of ostectomy should be 3–4 mm anterior to the mental foramen (double arrow). Maintaining a 3–4-mm distance from the distal of the mental foramen will reduce postsurgical paresthesia. (b) Nerve transpositioning with the block technique. Two bone segments are removed. (c, d) Nerve transpositioning with the groove technique. Nerve protector is used to protect the IAN and reduce paresthesia. (e) Transection of the incisive branch to facilitate nerve transpositioning (distalization)
7.4.3 Repositioning the Neurovascular Bundle Outside of the IAC
The portion of the surgery when the nerve is released and withdrawn from the IAC is one of the stages that may lead to nerve damage. The neurovascular bundle inside the canal is released using special curettes, and it is moved laterally using a blunt nerve hook. Bone removal in close vicinity to the neurovascular bundle should be performed patiently and thoroughly. This is usually performed using special curettes parallel to the surface of nerve bundles in an anteroposterior direction. Tiny bone spicules around the nerve should be removed. The area should be thoroughly irrigated so that the nerve bundle can be clearly seen. Spongy bone surrounding the nerve is removed using a special curved curette. The nerve is released and slowly retracted from the canal using a nerve hook. The hook should be rounded at the end and polished (Fig. 7.8). Care is taken to avoid any tension or sudden movement of the nerve, which may cause injury.
Fig. 7.8
(a) Spongy bone surrounding the nerve is removed using a special curved curette. (b) The nerve is released and slowly retracted from the canal using a nerve hook
7.4.4 Nerve Damage During IAN Retraction from the Canal for Drilling and Implant Insertion
Another important stage that may cause damage to the IAN is when the nerve is outside of the canal. Some studies have suggested various techniques for protecting the nerve outside of the canal and retracting it while drilling for implant placement. Such techniques include the use of a looped suture [6], small green cloth [34], piece of a suture cover [13], half of the rubber piston of a dental cartridge [35], umbilical tape [25], vessel loops [10, 16, 32], and elastic bands (author’s preference).
The important strategy for preventing nerve damage in this stage relies on increasing the contact surface in order to decrease pressure on the nerve. The more the contact surface decreases, the more the nerve damage will occur (pressure = force/area). So, avoid exerting too much traction upon the nerve when lateralizing the nerve and during nerve repositioning; attempt to transform the contact point to a contact area (Fig. 7.9). Then, a 10-mm-wide gauze cord or elastic band is passed below the IAN retracting it away from the surgical site decreasing ischemic trauma to the nerve. It also retracts the nerve away from the surgical site during the operation reducing the risk of iatrogenic nerve damage [2, 13, 30, 32] (Figs. 7.10 and 7.11). The advantage of using a wide elastic band is that it counteracts the tension of the nerve to some extent and also decreases the final pressure on the nerve due to its elasticity. Also, the retracted neurovascular bundle must be constantly moistened by normal saline.
Fig. 7.9
Avoid forming a contact point (a) between the retracting tape and the IAN. Contact between these two should be in the form of a contact area (b) rather than a contact point
Fig. 7.10
The nerve is retracted from the site (a) using 10-mm-wide umbilical tape (b) or elastic band (c) in order to protect it from any damage during implant placement. The advantage of an elastic band is that if it is pulled during surgery, the traction is neutralized by the band and not transferred to the nerve. Other techniques include looped suture (d), small green cloth (e), piece of a suture cover (f), half of the rubber piston of a dental cartridge (g), and vessel loop (h)
Fig. 7.11
Implant osteotomy preparation with lateral nerve retraction (a, b)
7.4.5 Repositioning the Neurovascular Bundle Inside the Canal
Finally, the last stage of possible nerve damage refers to the process of nerve repositioning, when the nerve is replaced back into the IAC, and the contact between the nerve and the implant occurs. Prior to this phase, the surgeon should decide whether or not to place material(s) between the implant and the nerve. There is a lot of controversy in this regard and some studies have been performed on animal models in this respect. In a study by Yoshimoto et al. with rabbits, no difference was observed microscopically after placing and not placing a membrane between the implant and the nerve bundle [36]. On the other hand, in the Kahnberg et al. dog study, healing was not complete after 14 weeks, but none of the implants were exposed. Histologic examination showed that in cases where a membrane had not been placed, a small contact was present between the nerve bundle and the implant. When a membrane is used, the distance between the nerve bundle and the implant will be four to eight times greater. There is no contact between the nerve and the implant when using a membrane, but the bone is not seen around the implant either [37]. An autogenous bone graft, either from the bone removed to unroof the IAC or elsewhere, or banked bone, is always placed between the repositioned nerve and the associated implants to prevent direct contact of the IAN and thermal transmission or metallic sensitivity with the implant(s). Also, artificial material, such as calcium hydroxyapatite, should never be placed in direct contact with the nerve. A severe inflammatory reaction in the nerve, similar to a chemical burn with dense scarring, accompanied by considerable pain, is often the unfortunate result. Surgical treatment of such injuries is problematic [33]. The author’s preference is to place a collagen membrane or autogenous bone graft in between the implant and IAN [10, 33]. A potential advantage of bone grafting over membrane placement is that if proper healing occurs in the area, the contact area of implant and bone will increase for osseointegration (Fig. 7.12).
Fig. 7.12
Replacement of the IAN within the IAC. (a) Direct contact of nerve and implant (not recommended). (b) Membrane placement (arrow) between the implant and IAN. (c) Placement of a bone graft (arrow) between the repositioned IAN and implant L: Lingual, B: Buccal
Therefore, attention should be paid during and after surgery to minimize the factors responsible for ischemia and mechanical neurotrauma. Such factors in the order of most common to the least common during nerve repositioning surgery include:
1.
Avoid exerting too much traction on the nerve. When lateralizing the nerve and during nerve repositioning, try to transform the contact point to a contact area.
2.
During ostectomy care must be taken to not injure the nerve with rotary instruments, curettes, or elevators. Direct contact of rotary or other surgical instruments with the nerve is among the most serious injuries in this type of surgery. Consider using a nerve protector.
3.
In order to lateralize the nerve, use instruments with minimal traction and prevent ischemia to the nerve. Instruments that have large contact area with the nerve and minimum thickness are preferred to be placed between the nerve and the location of drilling for implant placement.
4.
The retracted IAN bundle should be constantly moistened with normal saline.
5.
Prevent development of a hematoma since it places pressure on the nerve trunk.
7.5 Histological Findings Associated with Nerve Repositioning and Implant Placement
Yoshimoto et al. evaluated the condition of the tissues surrounding the implant 8 weeks after nerve repositioning surgery and simultaneous implant placement; they observed that none of the implants were exposed, and all were stable. No infection or inflammation was observed at the site. In all cases bone formation between the implant and neurovascular bundle was observed, and no direct contact was seen between them (Fig. 7.13). Research demonstrates that bone formation around the implant surface sandblasted with aluminum oxide was 2.5 times greater than a smooth titanium surface. Bone formation around the neurovascular bundle prevents the implant from having direct physical contact with the bundle, and therefore the nerve structure will be protected from mechanical or thermal trauma. Microscopic sections show the formation of a vascular network in the adjacent tissues that demonstrates that there is no need for placing a barrier or any kind of graft material to separate the nerve from the implant [36].
Fig. 7.13
Fluorescent microscopy showing relationship of IAN and implant following nerve repositioning surgery in a rabbit (star implant, arrow IAN). Bone formation is shown by fluorescent indicators (a, b) [36]
In Kahnberg et al. study on a dog, healing was not complete after 14 weeks, but none of the implants were exposed. Histologic examination showed that in cases where a membrane had not been placed, a small contact was present between the nerve bundle and the implant (Fig. 7.14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








