CHAPTER 21 Negative pressure wound therapy
1. Compare and contrast two different types of negative pressure wound therapy (NPWT).
2. Discuss three mechanisms for the effects of NPWT on wound healing.
3. Describe three indications, contraindications, and precautions for NPWT.
4. Describe the application of NPWT, including in undermined or sinus areas.
Negative pressure wound therapy (NPWT) is the application of subatmospheric (negative) pressure to a wound through suction to facilitate healing and collect wound fluid (Campbell et al, 2008; Vikatmaa et al, 2008). The use of NPWT as an open wound therapy was developed during the 1940s in Germany (Vikatmaa et al, 2008). During the 1970s and 1980s, the concept was applied to the management of draining wounds, such as enteric fistulas, by placing a suction catheter or fenestrated drain tube on a moist gauze-covered wound bed, connecting the catheter to wall suction, and covering the wound (and exit site of the catheter) with a transparent adhesive dressing (Chariker et al, 1989; Irrgang and Bryant, 1984; Orringer et al, 1987). This technique was referred to as closed suction wound drainage, with the primary objective of containing drainage.
During the 1990s, NPWT was further explored by Morykwas et al (1997). A porous polyurethane foam was introduced as the filler dressing. Since that time, NPWT has evolved to worldwide acceptance in wound healing (Vikatmaa et al, 2008).
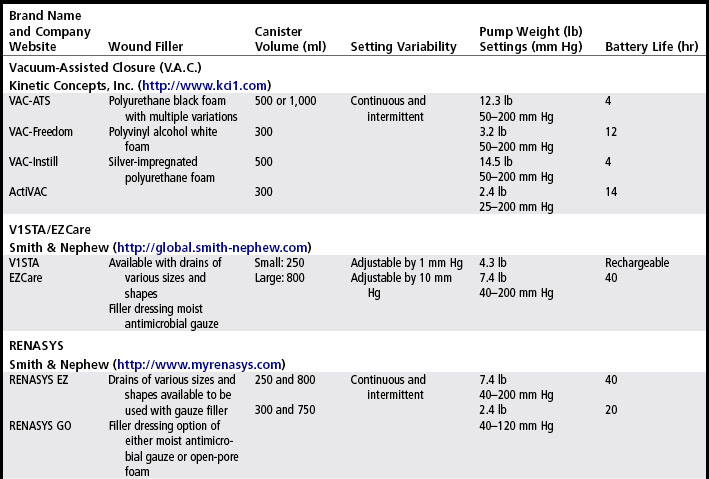
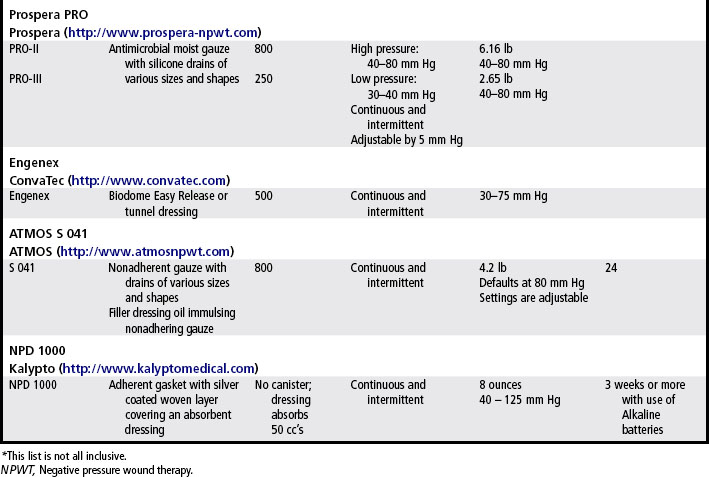
Today, several systems are available that provide NPWT (Table 21-1). The components of NPWT include a wound filler dressing, suction catheter, transparent cover dressing, suction source (i.e., pump) and collection container. Various wound filler dressings are now used: (1) open cell foam, (2) silicone tubing wrapped with gauze (either plain or antimicrobial), (3) honeycomb configured nonadherent matrix, and (4) non-woven superabsorbent polymer.
Mechanism of action
NPWT expedites wound healing through the use of controlled subatmospheric pressure using the body’s own defense mechanisms to enhance moist wound healing (Ubbink et al, 2008). Thus far, the mechanisms of action have been elucidated through animal and in vivo models (Saxena et al, 2004). Primary effects have been categorized as (1) edema reduction and fluid removal, (2) macro-deformation and wound contraction, and (3) micro-deformation and mechanical stretch perfusion. Secondary effects include increased angiogenesis, granulation tissue formation, and reduction in bacterial bioburden (Orgill et al, 2009).
Edema reduction and removal of wound fluid
Removal of exudate containing toxic cytokines, bacteria, and matrix metalloproteinases and reduction of interstitial edema is a primary benefit of NPWT (Ubbink et al, 2008). By reducing tissue edema, the compressive effects of edema upon the periwound vasculature are decreased, thereby improving tissue perfusion, delivery of nutrients, and uptake of oxygen culminating in the wound’s ability to resist bacterial proliferation and microbial penetration (Orgill et al, 2009). A decrease in wound bacterial load was first described in the porcine model by Morykwas et al (1997). Three mechanisms have been theorized to address the reduced wound bioburden associated with NPWT: (1) removal of stagnant wound fluid, (2) direct removal of bacteria from the wound bed, and (3) increased perfusion and thus increased immunity and oxygenation (Orgill et al, 2009). A porcine model study with daily biopsies revealed a reduction of Staphylococcus aureus from 108 to 105 by days 4 and 5 when the wound was treated with NPWT. In comparison, the moist saline dressing wound did not experience a decrease in Staphylococcus until day 11 (Banwell and Téot, 2003). Additional inconsistent reductions in bioburden have been reported. For example, NPWT has created a significant decrease in nonfermentative, gram-negative bacilli, but an increase in S. aureus was found in the NPWT wound (Moues et al, 2004). Removal and collection of wound exudate allow closed system containment that significantly reduces the frequency of dressing changes and exposure to external contaminants (Pham et al, 2006).
Macro-deformation and wound contraction
Intact skin and soft tissue have a natural tension that, when disrupted, causes skin and soft tissues to typically pull apart (separate). Distractive tissue forces may act to keep a wound open, with vectors that oppose contraction, thereby delaying healing. Negative pressure dressings can oppose these distractive soft tissue vectors (Franz et al, 2008). The application of suction allows contraction or pulling together of the wound edges, simulating the application of an abdominal binder. The pulling together of the wound edges (contraction) has allowed earlier healing, with delayed primary or secondary intention. This contraction process occurs three dimensionally through mechanical forces, thus allowing decreased wound volume symmetrically and facilitating faster wound closure (Orgill et al, 2009; Ubbink et al, 2008).
Micro-deformation and mechanical stretch
Histologic wound sections have demonstrated micro-deformations of the wound surface present with NPWT that is not present underneath occlusive dressings alone (Saxena et al, 2004). Mechanically, deformation results in fluid flow within the matrix and strain where the matrix cells are anchored. Thus, cells are subjected to both mechanical stretch mediated by their attachments to the matrix as well as shear stresses due to fluid flow. Fluid shear stresses are known to regulate cellular proliferation (Ubbink et al, 2008).
Wound surface micro-deformations seem to stimulate increased vascular growth. The stretching of the wound surface is hypothesized to stimulate cell division, proliferation, and angiogenesis (Orgill et al, 2004). In vivo models have demonstrated that cells respond to tension with directional growth and specific gene release (vascular endothelial growth factor) when mechanical tension has been applied (Orgill et al, 2004; Saxena et al, 2004). Saxena et al (2004) hypothesized that application of mechanical force initiates cellular response inducing a cascade of cellular proliferation, angiogenesis, and thus promotion of wound healing. The term mechanotransduction has been adopted to denote this cellular and physiologic response to mechanical strain (Orgill et al, 2009). In terms of the effect of NPWT on surrounding skin perfusion, it is hypothesized that increased perfusion occurs with the treatment, although the testing mechanism (laser Doppler) was criticized as being an indirect measure of blood flow (Morykwas et al, 2006; Orgill et al, 2009).
Morykwas et al (1997) reported an increase of more than 60% in granulation tissue formation using NPWT in comparison to moist gauze in porcine wounds. Numerous human studies have found increased and/or faster closure rates of wounds when treated with NPWT versus standard practice. Comparison of NPWT to standard compression therapy in primarily venous lower leg ulcerations revealed faster wound bed preparation (7 vs 17 days) and faster healing rates (29 vs 45 days) (Vuerstack et al, 2006). Faster granulation tissue coverage over diabetic foot wounds resulted in accelerated wound closure when NPWT was used (Blume et al, 2008).
Indications and uses
NPWT is approved for use with chronic, acute, traumatic, subacute and dehisced wounds, partial-thickness burns, ulcers (e.g., diabetic or pressure), and flaps and grafts once nonviable tissue is removed. The modality is used clinically with wounds of all sizes and depths but most favorably in complicated deep wounds. It can be used with tunnels, undermining, or sinus tracts as long as the type of wound filler dressing used can be easily retrieved and is compatible with the chosen system. Granulation tissue has formed with NPWT over orthopedic hardware, tendons, and bone. NPWT can be used in the presence of wound infection or osteomyelitis only after appropriate debridement and antibiotics have been initiated (Andros et al, 2006).
Among national evidence-based guidelines for chronic wounds, NPWT is recommended for the treatment of nonhealing pressure ulcers and diabetic wounds when conventional therapies have failed (NPUAP-EPUAP, 2009; Steed et al, 2006; Whitney et al, 2006). The WOCN reports increased rates of healing associated with Stage III and IV pressure ulcers (WOCN, 2010). Arterial ulcer treatment guidelines note NPWT may have an adjunct role in the management of arterial ulcers (Hopf et al, 2006). Acute wound healing guidelines advocate NPWT to oppose distractive soft tissue vectors that may act to delay healing and keep an acute wound, especially an open abdominal wound (Franz et al, 2008). NPWT has been identified as a strong option for preparation and management of skin graft/flap (Gray and Peirce, 2004; Robson et al, 2006).
Contraindications and precautions
Although serious adverse events are rare (Gray and Peirce, 2004), the U.S. Food and Drug Administration (FDA) has released reports of six deaths and 77 injuries associated with NPWT (FDA, 2009). The contraindications and precautions for NPWT use are given in Checklist 21-1. NPWT is contraindicated in the presence of untreated osteomyelitis, necrotic tissue, exposed blood vessels, exposed organs, nonenteric or unexplored fistulas, and malignancy in the wound (select manufacturers). Precautions and close monitoring are indicated with the use of NPWT in the presence of treated infection, treated osteomyelitis, potential for hemorrhage, anticoagulation therapy, postsurgical malignancy excision, and poor patient compliance with supervision (Andros et al, 2006).