10. Myofascial release techniques and connective tissue massage
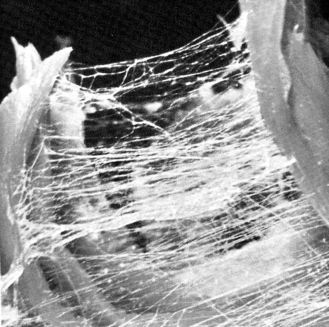
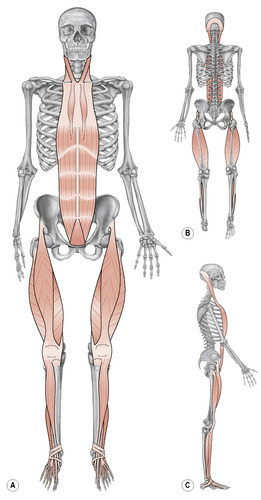
Connective tissue (Fig. 10.1) is one of the most abundant tissue forms in the human body. It serves to connect, support, bind, and separate either organs or other forms of tissue. It is divided into ordinary and specialized connective tissue subgroups.
 |
| Figure 10.1 |
Ordinary connective tissue provides a mechanical link between muscles and bones, or bones and joints, and binds cells together into tissues, organs, and systems (Watkins 1999). Examples include: tendons, aponeuroses, ligaments, fasciae, Sharpey’s fibers, joint capsules, loose irregular connective tissue that serves as a pathway for nerves and blood vessels, and adipose tissue (Watkins, 1999 and Stanborough, 2004).
Specialized connective tissue comprises bone, cartilage, and blood (Watkins, 1999 and Stanborough, 2004).
Examples of ordinary connective tissue structures frequently treated by sports massage therapists are fasciae, tendons, aponeuroses, ligaments, joint capsules, and dysfunctional states like fibrotic tissue and adhesions. The fascial connective tissue in the human body is often described as a three-dimensional web or network, to which many other structures are linked in one way or another as it runs through the body. Ida Rolf, one of the pioneers of myofascial work, called this fascial web “the organ of structure” (Smith 2005).
Connective tissue(Fig. 10.1)
In reality, it may be somewhat difficult to functionally separate muscles, fasciae, nerves, and blood vessels from each other since these structures work in unison during movement (Myers 2002). Additionally, most manual treatment forms will affect all these structures simultaneously, albeit more or less effectively. The realization of the structural importance of fascial connective tissue, and its consequences on function or health if dysfunctional, inspired the development of more specific connective tissue and myofascial treatment techniques.
Exercises strongly affecting the myofascial system can be traced back to at least as far as the roots of Hatha yoga, and several manual treatment forms, including massage, have existed since ancient times. In Sweden, Per Henrik Ling founded in the early 1800s the “Swedish movement cure,” where massage, stretching, and exercise were combined to generate health. In the USA, Dr. Andrew Taylor Still founded osteopathy in 1874 (Chikly 2005), which addressed movement restrictions and compression of nerves, blood, and lymph vessels by bone, muscles, or inflammatory swelling (Chikly 2005). These conditions were initially treated by gently manipulating the joints, particularly in the spine. Osteopathy later evolved to include a wide range of specific myofascial and other soft tissue techniques.
Dr. Oakley Smith, one of the first dozen chiropractors in the USA, founded the manual therapy discipline naprapathy in 1905 after realizing the extent to which scar and/or generally shortened connective tissue could interfere with the function of blood vessels, nerves, and other structures, ultimately causing pathology (Smith, 1919, Smith, 1966 and Smith, 1932). He stated that not only traumatic injuries could cause debilitating changes in connective tissue, but poor diet, insufficient rest, and poor personal hygiene might as well (Smith 1932). Smith established that through different angles in sequence, repeatedly stretching the connective tissue fibers of contractures with specially developed manipulation techniques could normalize dysfunction and also release nerve interference along the spinal column (Smith 1932). He consequently called the techniques “stretchments” (or “naprapathic directos”) instead of “adjustments,” to emphasize the treatment intention, and considered this a key to producing more lasting relief for the patient (Smith 1932). Moreover, Smith considered scar tissue to be one of the most stubborn conditions the body must deal with, and that it could account for the chronic nature of many symptoms (Smith 1932).
After many years of extensive research, Dr. Ida Rolf founded “structural integration” in the 1960s (Smith 2005) to address structural and postural dysfunctional patterns in the body. This treatment form is commonly referred to nowadays as Rolfing (Stanborough 2004), and it is practiced by many manual therapists around the world. Rolfing has been demonstrated to produce physiological effects on myofascial structures and the peripheral nervous system (Jones 2004). The method is traditionally performed in a series of ten treatments, each addressing different areas or conditions of the body.
Several other myofascial treatment systems have emerged over the years, each offering different perspectives and additions. Some were created by former students of Ida Rolf, or her institute, such as Joseph Heller—Heller work, Judith Aston—Aston patterning, Tom Myers—anatomy trains, and Erik Dalton—myoskeletal alignment techniques; whilst additional methods were formed by other therapists like Dr. Leon Chaitow—soft tissue manipulation, John F. Barnes—one of the forces behind myofascial release, Jack Painter—postural integration, William Leigh—Zen bodytherapy, and others (Myers, 2002 and Smith, 2005). Today, myofascial release is a very popular soft tissue treatment method comprising several styles, some gentler whilst others present a more forceful approach.
Myofascial release techniques are valuable in sports massage therapy since they can assist the athlete toward optimal posture, movement ability, and recovery. For instance, it has been shown that myofascial release massage supports recovery back to preexercise levels with regard to heart rate variability and diastolic blood pressure after high-intensity exercise (Arroyo-Morales et al. 2008). It is indicated that patients with carpal tunnel syndrome treated with myofascial release manipulation and self-stretching improved clinically (Sucher 1993). Myofascial release also produces effects on the autonomic nervous system (Henley et al. 2008), and it is suggested that runners who present coexisting sacroiliac joint dysfunction and internal snapping hip syndrome may benefit from myofascial release in combination with proprioceptive neuromuscular facilitation (Konczak & Ames 2005). Fascia is somewhat pliable, and myofascial release uses this tissue plasticity in the treatment to achieve more lasting results. Research suggests that the integration of plasticity from connective tissue with the nervous system may possibly clarify mechanisms of an assortment of treatment methods that may reverse chronic lower back pain by employing mechanical forces to soft tissue (Langevin & Sherman 2007).
Fascial connective tissues have previously been viewed as solely passive structures, capable only of conveying mechanical tension produced by muscle activation or an external force (Schleip et al. 2005). It is now suggested, however, that there is evidence of contractile cells in fascia, possibly enabling a contraction with similar behavior to smooth muscle (Schleip et al. 2005). Successful demonstrations of autonomous contraction of human lumbar fascia, in vitro studies with fascia, and pharmacological stimulation of temporary contractions in ordinary fascia in rats, support this hypothesis (Schleip et al. 2005). If confirmed by additional research, active fascial contractibility could present remarkable benefits for the comprehension of certain musculoskeletal pathologies, and a deeper understanding of the effects of treatments like myofascial release techniques (Schleip et al. 2005).
Effects in the fascial network
Fascia comprises three layers in the human body: the superficial fascia secures the dermis of the skin to underlying structures, deep fascia surrounds individual organs and muscles, and the subserous fascia, situated between the internal layer of the deep fascia and the serous membranes, lines the cavities of the body.
The fascial “network” in the body is formed when several fascial structures are linked to each other in specific patterns. A shortening of the connective tissue in one part will therefore have an effect in another, possibly more distant, area of the body (Fig. 10.2). A recent study demonstrated the presence of myofascial force transmission between antagonistic muscles. Lengthening of the extensor digitorum longus muscle in the lower leg changed forces applied on the tibia and forces exerted by the antagonistic peroneal muscle group, which could be possible only through existing “extramuscular myofascial connections” (Huijing & Baan 2008).
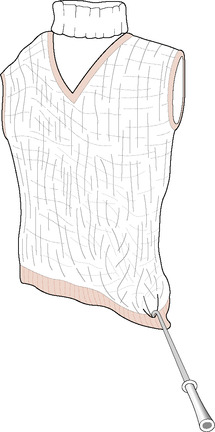 |
| Figure 10.2 |
Thomas Myers describes the linked fascial structures as “myofascial meridians” (Myers 2002) that form specific pathways, or individual “anatomy train lines” (Myers 2002), as they run through the body. These pathways generate structural tensile strength and support in the body, but can create dysfunctions if adaptively shortened or injured. Having an understanding of the principle of the fascial trajectory enables the sports massage therapist to more effectively assess and treat structural connective tissue distortions.
Myers’ (2002) principle of “anatomy trains” presents myofascial meridian lines represented in seven groups:
1. Superficial back line.
2. Superficial front line.
3. Lateral line.
4. Spiral line.
5. Arm lines.
6. Deep front line.
7. Functional lines.
Techniques
As a general rule, myofascial release techniques are at first applied to superficial layers and then deeper structures are addressed as the more superficial fascial distortions treated release. Anterior–posterior balance is addressed firstly by working on the posterior and anterior superficial lines (Smith 2005). This is commonly followed by treatment of lateral distortions, followed by rotational issues.
Examples of myofascial release stroke applications
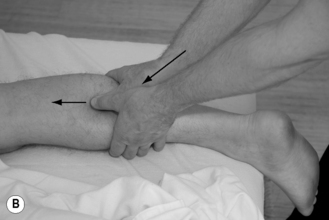
The myofascial release strokes are performed with fingers, loose fists, forearms, or elbows (Fig. 10.3), and are executed slowly to minimize activation of the myotatic/stretch reflex. The stroke is taken to the appropriate depth, and it is important the therapist continuously feels contact with the fascial layer and registers the body’s response. By applying body weight, the stroke slowly slides through the tissue (Smith 2005). Should the glide ratio be too high, the “grip” in the fascia is lost, and the stroke must be reapplied. The amount of emollient used is consequently sparse to ensure maximal stretch effect without injuring the skin.
 |
 |
 |
 |
| Figure 10.3 Example of myofascial release stroke applicationsA Fingers/“chisel” (Smith 2005) stroke B Fist stroke C Forearm stroke D Elbow stroke |
The stroke angle can also be modified during implementation to ensure a continued stretch effect in the fascial structure. Typically, a 45-degree angle into both the tissue and treatment direction will ensure the desired stretch effect, but a supplementary 45-degree angle across the fiber direction may also be required. The athlete can also assist upon the therapist’s command by actively generating slow movements, thus lengthening the treated tissue into an augmented stretch, and moreover simultaneously assisting in proprioceptive conditioning (Smith 2005).
The following are examples of basic myofascial release techniques of the back, front, and lateral lines. Additional techniques are presented in Chapter 14.
Superficial back line
The superficial back line (SBL) connects the whole posterior aspect of the body (Fig. 10.4). It consists of two lines, parallel to the midline, running from the bottom of the feet to the top of the head. The SBL holds an important postural function, which generally renders fascial structures thicker and stronger.
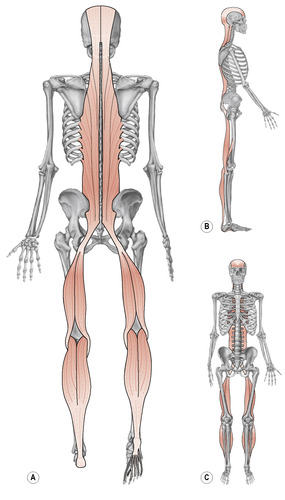 |
| Figure 10.4 Reproduced with permission from Myers 2002 |
Important myofascial structures of the SBL (Myers 2002)
• Plantar aponeurosis.
• Calcaneus tendon.
• Ischiocrural/hamstring fasciae including the tendons.
• Sacrotuberous ligament.
• Thoracolumbar fascia.
• Longitudinal fascial aspect of the erector spinae group.
• Structures at the occipital ridge.
Fist glide of the plantar aponeurosis
The therapist uses the fist with major contact on the second and third knuckle area to initiate the stroke just anterior to the calcaneus bone (Fig. 10.5). As the stroke slowly glides toward the toes, the athlete is simultaneously asked to slowly extend the toes.
 |
| Figure 10.5 |
Fist glide and thumb glide on triceps surae muscle
The athlete lies prone. The therapist glides with the fist supported by the other hand, or with a reinforced thumb (Fig. 10.6) from just superior to the athlete’s heel. The stroke is gradually worked up to the posterior aspect of the knee. The athlete can assist with slow active dorsiflexion of the ankle joint.
The ischiocrural/hamstring muscle group
The athlete remains prone but with the knee resting in flexion (Fig. 10.7). The therapist uses the flat part of the elbow to gradually massage and stretch the fascial layers up to the ischial tuberosity. The athlete can assist with active extension of the knee joint.
 |
| Figure 10.7 |
The ischiocrural/hamstring muscles and tendons located at the knee serve to assist the anterior cruciate ligament by supporting the integration between the tibia and femur when forces stress the tibia anteriorly (Di Fabio et al. 1992).
Thoracolumbar fascia
The athlete rests prone in the yoga pose named “child’s pose” (Smith 2005) (Fig. 10.8). The therapist uses the forearm or palm heel to slowly glide up toward the 12th rib area. The stroke is performed both in a direction along the spine and at a 45-degree angle away from the spine.
 |
| Figure 10.8 |
Erector spinae fasciae
The athlete rests in a sitting position. The therapist uses the fists of both hands on both sides of the athlete’s spine, starting in the lower neck area (Fig. 10.9). The athlete is asked to slowly and gradually bend forward, starting with the head, as the therapist’s fists slowly glide downward, stretching the longitudinal fascial layers all the way to the sacrum.
 |
| Figure 10.9 |
Posterior aspect of the neck
The athlete lies supine. The therapist hooks the fingertips on one side of the neck just lateral to the spine in the T1/C7 area (Fig. 10.10). The therapist slowly lifts the head, with active assistance from the athlete, as the fingers slowly glide laterally. The stroke is segmentally performed up to the occipital bone, and then repeated on the opposite side.
Superficial front line
The superficial front line (SFL) connects the whole anterior aspect of the body, starting from the dorsum of the toes and feet, and running up to the lateral aspects of the skull (Fig. 10.11). The SFL and SBL mutually support and balance each other during postural activity (Myers 2002).
 Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|