Musculoskeletal Ultrasound: Introduction
Musculoskeletal ultrasound (MSUS) imaging has been incorporated in the care of the rheumatologic patient for more than a decade in Europe. On the contrary, MSUS is a relatively recent addition in the diagnostic armamentarium of rheumatologists in the United States.
MSUS can significantly advance the diagnostic potential in rheumatology and improve the accuracy of musculoskeletal procedural interventions. The most experience with ultrasound stems from its applications in arthritic conditions. However, the diagnosis of a wide spectrum of rheumatologic conditions can be facilitated by its use.
Ultrasound Technology
Ultrasound machines consist of a processing unit and a transducer. Many models of different sizes and degrees of portability are available by various manufacturers. Ultrasound technology couples gray scale imaging and Doppler imaging to evaluate anatomic integrity and tissue inflammation.
The human ear can perceive sound waves in frequencies between 20 Hz and 20,000 Hz. Sound waves above the hearing frequency are called ultrasounds.
The acquisition of ultrasound images is based on the echo phenomenon. A transducer attached to the ultrasound machine transmits ultrasound waves that “travel” through the tissues. Each tissue has different acoustic properties based on their consistency, compressibility, and density. Different acoustic properties translate into differences in the velocity with which ultrasound waves are transmitted through each particular tissue. Reflection at tissue interfaces generates returning echoes that are collected by piezoelectric crystals in the transducer. The electric potentials generated at the piezoelectric crystals are then transformed to gray scale imaging displayed on a monitor.
The more echoes returned, the more “white” the tissues that generated the echoes will appear.
Structures without internal reflectors do not return any echoes, and this results in black areas in the ultrasound image. Such structures are fluid collections or tissues containing high concentrations of water such as the cartilage or joint effusions. These tissues are called hypoechoic in ultrasound terminology.
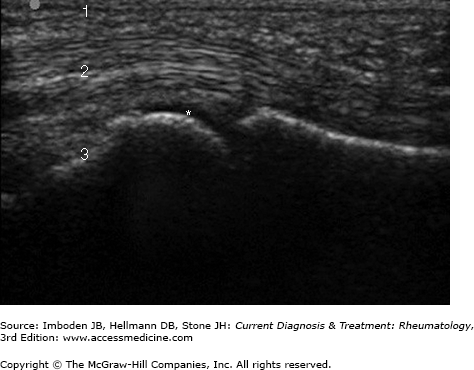
Structures that produce weaker ultrasound reflections generate low level echoes and correspond to dark gray areas in the ultrasound images. These structures are called isoechoic and include muscle, tendons, synovial tissue, and nerves (Figure 66–1).
Lastly, tissues with strong internal reflectors return strong echoes and generate bright gray or white areas in the ultrasound image. These structures are called hyperechoic and include bone, calcifications, and foreign bodies.
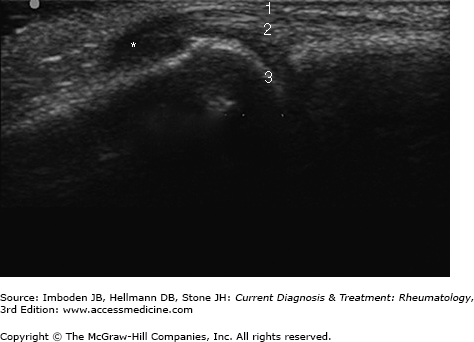
Inflammation is associated with local hyperemia. Increased blood flow in synovitis (Figure 66–2 and Plate 50), tenosynovitis, and enthesitis (Figure 66–3) can be detected with the use of Doppler ultrasonography. The detection of blood flow locally is transformed to a color signal that is coupled with the gray image obtained as described above. The more intense the inflammation the more intense is the color signal. More details about the physics of the Doppler phenomenon are beyond the scope of this book.
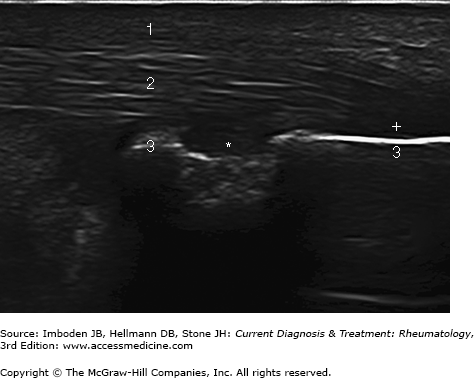
Figure 66–3.
Achilles tendon enthesitis. Key: 1, subcutaneous tissue; 2, Achilles tendon; 3, calcaneous; +, hypoechoic area at the enthesis of the Achilles tendon indicative of inflammation (decreased tendon echogenicity); *, the center of a discontinuation of the cortical surface of the calcaneous corresponding to an erosion.
Doppler sonography can permit differentiation between inflammatory and degenerative conditions, monitor the response to anti-inflammatory treatment, and detect mild inflammation that may not be obvious or may be ambiguous with only gray scale imaging.
Most of the MSUS machines are portable. As opposed to MRI and plain radiography, ultrasound imaging can take place at bedside. This allows for immediate imaging at the time of the clinical evaluation and frequently obviates the need for referrals to radiology. MSUS allows dynamic evaluation of joints and also evaluation of multiple joints in one session depending on the needs of the clinical encounter. It is a low-cost procedure and there is no radiation exposure. Contraindications to other imaging modalities such as claustrophobia or metal implants do not apply to ultrasound imaging.
Research has shown that patients with arthritis have lower expectations for their health and may compromise with a lower quality of life. Engaging the patient to actively participate in his or her treatment would potentially improve outcomes. Since ultrasound imaging is an interactive process performed by the treating rheumatologist, it allows the physician to share with the patient how inflammation responds to treatment, compare images acquired before and after initiation of therapy, or justify more aggressive treatment. This permits education, better collaboration with the patient, and possibly better patient outcomes.
Applications of MSUS
Gray scale imaging allows the detection of inflammation within the joints by assessing the thickness of the synovium, the presence of fluid, and the synovial tissue compressibility. Doppler imaging may reveal the presence of low blood flow state and hyperemia associated with synovitis.
Ultrasound can detect synovitis early (Figure 66–2). Studies have shown superiority compared to clinical examination and equivalency compared to MRI. Ultrasound imaging may allow the detection of residual inflammation in patients otherwise—by physical examination or by traditional outcome measures—thought to be in remission. Erosions can also be detected at an earlier stage and with higher sensitivity compared to plain radiography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree