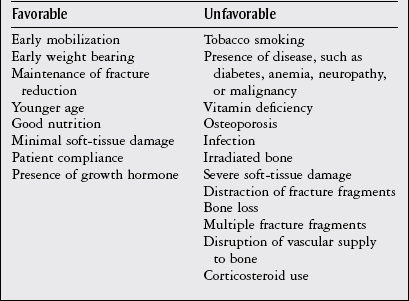
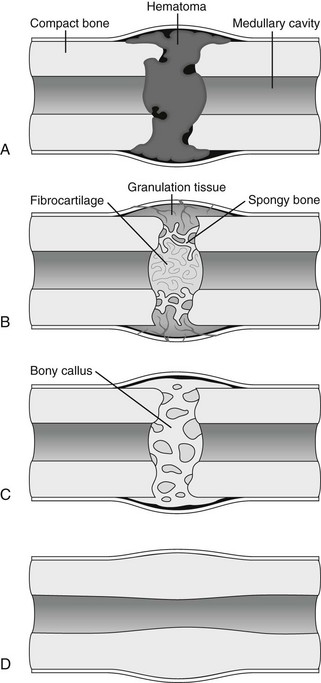
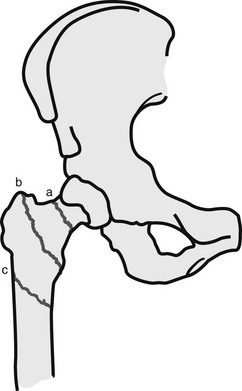
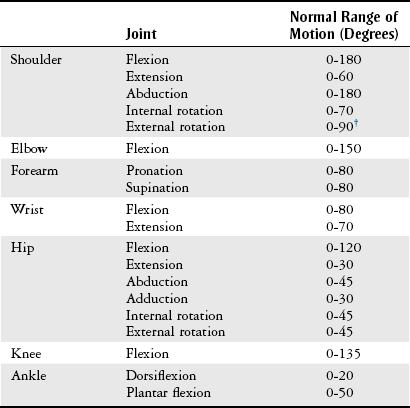
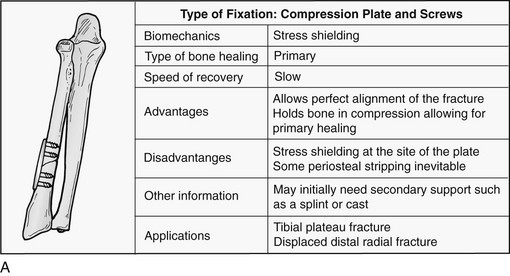
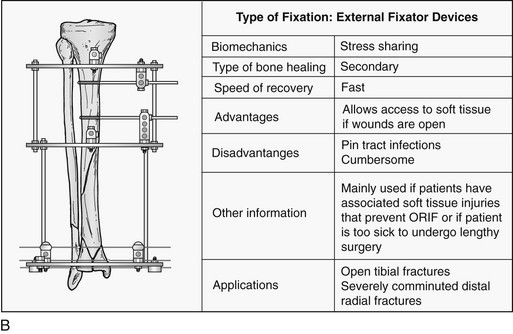
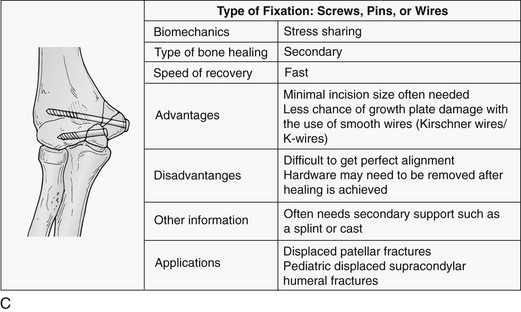
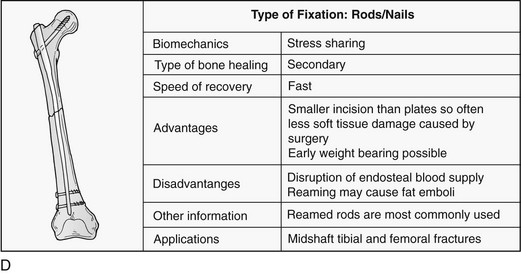
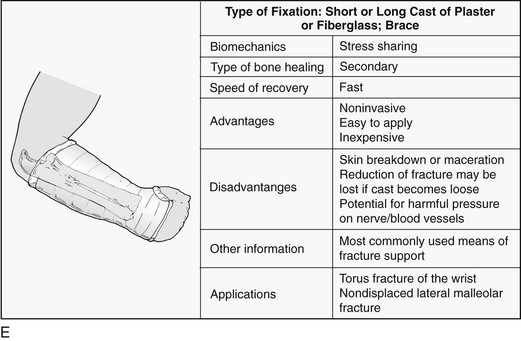
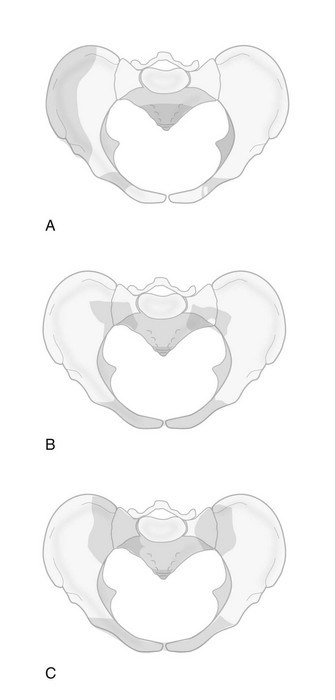
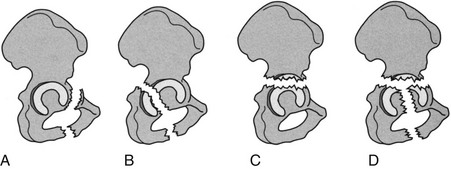
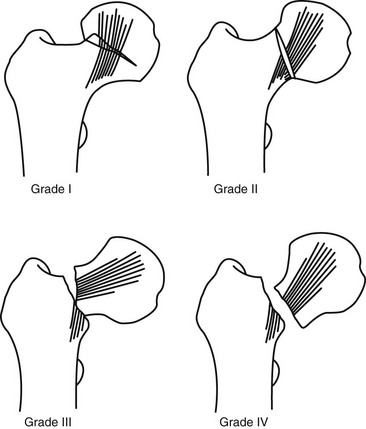
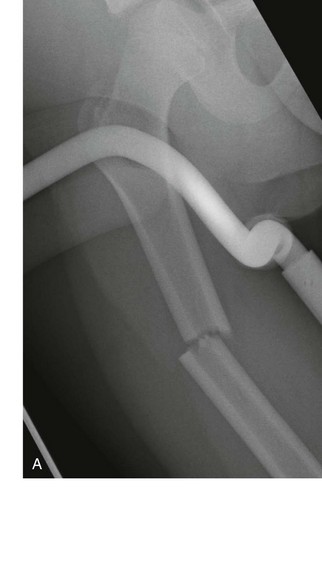
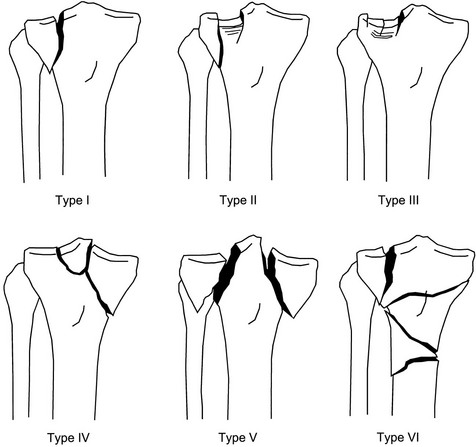
Chapter 5 Structure and Function of the Musculoskeletal System Decrease Pain and/or Muscle Guarding Prevent Circulatory and Pulmonary Complications Prevent Range of Motion and Strength Deficits Improve Functional Mobility While Protecting the Involved Structures Equipment Used in the Management of Musculoskeletal Pathologies The objectives of this chapter are the following: 1 Provide a brief overview of the structure and function of the musculoskeletal system 2 Describe the physical therapist’s examination and management of the patient with musculoskeletal impairments in the acute care setting 3 Give an overview of fracture management and common orthopedic surgeries seen in the acute care setting 4 Describe the equipment commonly used by patients with musculoskeletal impairments in the acute care setting Please refer to Appendix A for a complete list of the preferred practice patterns, as individual patient conditions are highly variable and other practice patterns may be applicable. Patients with orthopedic impairments often experience pain, frustration, and anxiety while maneuvering in an environment that frequently includes peripheral lines, catheters, casts, and drains. A challenge for physical therapists in the acute care setting is to accurately interpret the reasons for the patient’s presentation and then effectively achieve optimal outcomes in a very short time frame. To do this, the therapist must incorporate the judicious use of examination findings into the decision-making process. Various factors influence clinical reasoning. These factors include the therapist’s knowledge, expertise, goals, values, beliefs, and use of evidence; the patient’s age, diagnosis, and medical history, as well as his or her own goals, values, and beliefs; available resources; clinical practice environment; level of financial and social support; and the intended use of the collected information.1,2 Information about the patient’s history can be obtained from the medical record, the patient, and/or the patient’s caregivers. According to the Guide to Physical Therapist Practice, the different types of data that can be generated from the patient history include general demographics, social history, employment/work, growth and development, general health status, social/health habits, family history, medical/surgical history, current condition(s)/chief complaint(s), functional status and activity level, medications, and other clinical tests.3 In addition to a standard medical review (see Chapter 2), information pertaining to the patient’s musculoskeletal history should include the following: • Cause and mechanism of injury • Medical treatment and/or surgical procedures • Weight-bearing status, limitations on ROM, positioning of extremities • Equipment such as braces, orthotics, assistive device use • Comorbidities and medical history • Diagnostic test and laboratory results Computed tomography (CT) incorporates the use of radiography with a computer in order to provide images that have greater sensitivity than plain films alone. CT is the diagnostic test of choice for the evaluation of subtle and complex fractures; degenerative changes; trauma in which both soft-tissue and bone injuries are suspected; and loose bodies in a joint.4 Magnetic resonance imaging (MRI) is superior to x-ray or CT for the evaluation of soft tissue. MRI is the imaging modality of choice for the detection of partial or complete tendon, ligament, or meniscal tears; bony and soft-tissue tumors; and disc hernations.4 A bone scan is the radiographic picture of the uptake in bone of a radionuclide tracer. Bone scans reflect the metabolic status of the skeleton at the time of the scan. They can provide an early indication of increased bone activity and are therefore used to detect skeletal tumors, subtle fractures, infections, and avascular necrosis.4 A myelogram is a radiograph or CT of the spinal cord, nerve root, and dura mater with dye contrast. A myelogram can demonstrate spinal stenosis, spinal cord compression, intervertebral disc rupture, and nerve root injury.4 As with any test that includes contrast media, contrast-related reactions postarthrogram or myelogram may occur. • X-rays may be ordered after any new event, such as an in-hospital fall, abnormal angulation of an extremity, or possible loss of fixation or reduction, or for a dramatic increase in pain. Regardless of the situation, defer physical therapy intervention until results are reported or the situation is managed. • Physical therapy intervention is typically deferred for the patient post myelography secondary to specific postprocedure positioning and bed-rest restrictions. If physical therapy is scheduled immediately following the completion of this test, the physical therapist should verify with the nurse that the patient is able to participate in rehabilitation. Physical therapists should also be aware of the patient’s medications. If the patient is being seen shortly after surgery, the residual effects of general anesthesia may be present. Specifically, the patient could be woozy, confused, delirious, and/or weak.5 If a local anesthetic such as an epidural or spinal neural blockade is being used, the patient may have insufficient analgesia or diminished sensation or motor function.5 Refer to Chapter 20 for more detailed information on anesthesia. Pain medications, specifically opioid analgesics, are commonly used by this patient population. The physical therapist needs to be aware of the type of pain medication, its side effects, and dosing schedule in order to enhance the patient’s participation in rehabilitation. Refer to Chapter 21 for more information on pain management. The physical therapist should also collect information from the patient about his or her: • Functional level before admission • Previous use of assistive device(s) • Recreation or exercise level and frequency • Need for adaptive equipment or footwear on a regular basis (e.g., a shoe lift) • Any additional medical problems that limit use of assistive devices, participation in physical therapy • Anticipated discharge location to determine the presence of stairs, railings, and so forth The cardiovascular and pulmonary systems should be assessed for any signs or symptoms that indicate that the patient might not tolerate aerobic activities. As the energy expenditure (i.e., cardiopulmonary demand) required for use of an assistive device is greater than the demand imposed during ambulation without a device, it is important for the physical therapist to examine the aerobic capacity of the individual.6,7 Heart rate and rhythm, blood pressure, respiratory rate, and oxygen saturation (if applicable) must be assessed at rest, before the initiation of further tests and measures, as well as during and at the completion of aerobic activities (e.g., walking). The physical therapist should also examine the circulatory status of the patient. With decreased mobility, the risk for the development of deep venous thrombosis (DVT) increases. The lower extremities should be observed for signs of a DVT. Deficits in skin temperature, capillary refill, and peripheral pulses at the level of or distal to the injury or surgical site should also be noted. Refer to Chapter 7 for a further discussion on vascular examination. The patient’s skin should be screened for the presence and location of edema, bruising, lacerations, or surgical incisions. Skin integrity and color should be examined, especially around and distal to injuries and incisions. Pressure sores from prolonged or increased bed rest after trauma or orthopedic surgery can develop in anyone, regardless of age or previous functional abilities. The therapist should be aware of signs and symptoms of infection, circulatory compromise, or pressure ulcer development that would warrant further testing. Refer to Chapter 12 for a further discussion of skin integrity. The neuromuscular system should be assessed for impairments in sensation, especially in the involved extremity. Physical therapists should be aware of signs and symptoms of sensory deficits in patients with diabetes, compartment syndrome, and peripheral nerve injury (e.g., after THA, acute foot drop may be present because of injury to the sciatic nerve). Patients should be asked if they are experiencing any changes in sensation. Light touch awareness should be performed by lightly brushing different areas (distal and proximal, medial and lateral) on the extremity. The patient with eyes closed must recognize that a stimulus has been applied for the system to be intact. If deficits are noted, more formal testing is required. Refer to Chapter 6 for more detailed information on the nervous system. The physical therapist should observe the patient throughout the examination process (as well as during interventions) to determine if the patient is expressing or experiencing pain. The patient might present nonverbal indicators of pain such as behavior changes, facial expressions, and body language. The physical therapist should determine if pain is constant or variable and if movement or positioning increases or decreases the pain. Refer to Chapter 21 for more detailed information on pain assessment and management. If the patient is unable to move through the full available ROM, the therapist will then need to move the limb passively through the remaining range to determine if it is a strength deficit or loss of ROM. Further assessment of the magnitude of the ROM impairment can be examined both passively and actively via the use of a goniometer (e.g., after total knee arthroplasty). Table 5-1 outlines normal ROM values. TABLE 5-1 Normal Range-of-Motion Values* *Values are from the American Academy of Orthopedic Surgeons (AAOS) as reported in Appendix B of Reese NB, Bandy WD: Joint range of motion and muscle length testing, ed 2, St Louis, 2010, Saunders. †As the AAOS does not report a value for external rotation of the shoulder, the value is from the American Medical Association (AMA) as reported in Appendix B of Reese NB, Bandy WD: Joint range of motion and muscle length testing, ed 2, St Louis, 2010, Saunders. • Decrease pain and/or muscle guarding • Prevent circulatory and pulmonary complications • Prevent ROM and strength deficits • Improve functional mobility while protecting the involved structures The analysis and classification of fractures reveal the amount of energy imparted to bone, the extent of soft-tissue injury, and optimal fracture management. Traumatic fractures can be classified according to well-recognized classification systems such as the one established by the Orthopedic Trauma Association (OTA).8 They can also be described according to the following9,10: 1. The maintenance of skin integrity: a. A closed fracture is a fracture without disruption of the skin. b. An open fracture is a fracture with an open laceration of the skin or protrusion of the bone through the skin. 3. The classification of the fracture: a. A linear fracture lies parallel to the long axis of the bone. b. An oblique fracture lies on a diagonal to the long axis of the bone. c. A spiral fracture encircles the bone. d. A transverse fracture lies horizontal to the long axis of the bone. e. A comminuted fracture has two or more fragments; a butterfly (wedge-shaped) fragment may or may not be present. f. A segmental fracture has two or more fracture lines at different levels of the bone. g. A compression fracture occurs when the bone is crushed; it is common in the vertebrae. 4. The extent of the fracture: a. An incomplete fracture has only one portion of the cortex interrupted, and the bone is still in one piece. b. A complete fracture has all cortices of bone interrupted, and the bone is no longer in one piece. 5. The relative position of the fragments: The goal of fracture management is bony union of the fracture without further bone or soft-tissue damage that enables early restoration of maximal function.11 Early restoration of function minimizes cardiopulmonary compromise, muscle atrophy, and the loss of functional ROM. It also minimizes impairments associated with limited skeletal weight bearing (e.g., osteoporosis). Fractures are managed either nonoperatively or operatively on an elective, urgent, or emergent basis depending on the location and type of fracture, presence of secondary injuries, and hemodynamic stability. Elective or nonurgent management (days to weeks) applies to stable fractures with an intact neurovascular system or fracture previously managed with conservative measures that have failed. Urgent management (24 to 72 hours) applies to closed, unstable fractures, dislocations, or long bone stabilization with an intact neurovascular system. Emergent management applies to open fractures, fractures/dislocations with an impaired neurovascular system or compartment syndrome, and spinal injuries with increasing neurologic deficits.11 Fracture reduction is the process of aligning and approximating fracture fragments. Reduction may be achieved by either closed or open methods. Closed reduction is noninvasive and is achieved by manual manipulation or traction. Open reduction with internal fixation (ORIF) techniques require surgery and fixation devices commonly referred to as hardware. ORIF is the treatment of choice when closed methods cannot maintain adequate fixation throughout the healing phase. In order to decrease the extent of soft-tissue disruption that occurs when direct reduction is required, minimally invasive surgical techniques for fracture fixation have been developed. In minimal access surgery or minimally invasive surgery (MIS), the surgeon uses the least invasive access portal and mainly indirect reduction techniques to fixate the fracture.12 Immobilization of the fracture is required to maintain reduction and viability of the fracture site. Immobilization is accomplished through noninvasive (casts or splints) or invasive (screws, plates, rods, pins, and external fixators) techniques (Figure 5-1). Regardless of the method of immobilization, the goal is to promote bone healing. FIGURE 5-1 Fracture fixation methods. A, Compression plate and screws; B, external fixator devices; C, screws, pins, or wires. D, Rods/nails; E, short or long cast of plaster or fiberglass; brace. ORIF, Open reduction with internal fixation. (From Cameron MH, Monroe LG: Physical rehabilitation, St Louis, 2007, Saunders.) Fracture healing is complex and proceeds through two different processes. Primary cortical or direct healing occurs when bone fragments are anatomically aligned via rigid internal fixation, encounter minimal strain, and are stable.13 More commonly, fracture healing occurs through endochondral or secondary bone healing (Figure 5-2).14 The first stage (inflammatory stage) of this process involves the formation of a hematoma with a subsequent inflammatory response. The reparative phase follows and includes the influx of fibroblasts, chondroblasts, and osteoblasts that results in formation of a soft calcified cartilage callus. The remodeling phase begins with the transition of the soft callus to a permanent hard callus consisting of lamellar bone. In children, the healing of bone can take less than 2 months, whereas in adults it typically takes 2 or more months.15 Box 5-1 lists the multitude of factors that contribute to fracture healing. Complications of fracture may be immediate (within days), delayed (weeks to months), or late (months to years). The immediate or early medical-surgical complications of special interest in the acute care setting include16: • Loss of fixation or reduction • Deep vein thrombosis, pulmonary or fat emboli • Nerve damage, such as paresthesia or paralysis • Arterial damage, such as blood vessel laceration Delayed and late complications are as follows16: • Loss of fixation or reduction • Delayed union (fracture fails to unite in a normal time frame in the presence of unfavorable healing factors) • Nonunion (failure of fracture to unite) • Malunion (fracture healed with an angular or rotary deformity) • Pseudarthrosis (formation of a false joint at the fracture site) The pelvis is formed by the paired innominate bones, sacrum, sacroiliac joints, and the symphysis pubis. Stability of the pelvis is provided by the posterior sacroiliac ligamentous complex.17 Pelvic fractures are classified, according to the Orthopedic Trauma Association (OTA) classification system, based on the mechanism of injury and the resultant stability of the pelvic ring (Figure 5-3). FIGURE 5-3 Classification of pelvic fractures. Type A, Lesions sparing (or with no displacement of) the posterior pelvic arch. Type B, Incomplete disruption of the posterior arch (partially stable). Type C, Complete disruption of the posterior arch (unstable). (Courtesy of the Orthopedic Trauma Association.) Stable pelvic fractures (Type A injuries), due to low-impact direct blows or falls, do not disrupt the integrity of the pelvic ring.8 Stable pelvic fractures include avulsion and localized nondisplaced iliac wing, pubic rami, or sacral fractures. When a pelvic fracture is described as stable, it is typically treated nonsurgically. Mobilization of the patient can occur in 1 to 2 days after a brief period of bed rest.18,19 Ambulation with an assistive device that allows for limited weight bearing on the affected side is often prescribed. Disruption of the pelvic ring is commonly the result of high-energy injuries that result in concurrent damage to the urinary, reproductive, and bowel systems as well as soft tissues, blood vessels, and nerves.19 When two or more components of the pelvic ring are injured, leading to rotational instability, but the pelvis remains stable vertically because the posterior osteoligamentous complex has been only partially disrupted, the pelvic fracture is considered to be partially stable (Type B).8,17 If the posterior osteoligamentous complex is completely disrupted, the pelvis becomes unstable both vertically and rotationally (Type C).8,17 Type B and C injuries are treated with external fixation or internal fixation using plates and screws.18 Based on the stability of the fracture and type of fixation, the physician will determine the patient’s weight-bearing status, which could range from non–weight bearing (NWB) to weight bearing as tolerated (WBAT) on either one or both extremities. Functional mobility training, with the use of an assistive device, and active and active assisted ROM exercises for both lower extremities are encouraged as soon as the patient is physiologically stable.18 Acetabulum fractures occur when a high-impact blunt force is transmitted through the femoral head into the acetabulum. Depending on the direction of the force, different components of the acetabulum may be injured (Figure 5-4). If the hip is flexed and a force is transmitted through the femur posteriorly, as commonly occurs in a motor vehicle accident, the posterior wall will fracture.20 An acetabulum fracture is a complex injury and is associated with retroperitoneal hematomas, injury to the lungs, shock, dislocation or fracture of the femoral head, and sciatic nerve palsy.20,21 Acetabulum fractures are by nature intra-articular; hence, medical management focuses on the restoration of a functional and pain-free weight-bearing joint.22 Closed reduction via skeletal traction with bed rest for the initial 6 to 8 weeks may be used if the patient is unable to undergo surgery.22 Surgical management includes percutaneous pinning, open reduction with internal fixation, and hip arthroplasty. FIGURE 5-4 The innominate bone and the acetabulum are divided into anterior and posterior columns to reference the location of the trauma. Classification of acetabular fractures: A, anterior column; B, posterior column; C, transverse, involving both columns; D, complex or T-shaped, involving both columns. (From McKinnis LM: Fundamentals of musculoskeletal imaging, Philadelphia, 2010, FA Davis, p 348.) Fractures of the proximal femur include proximal trochanteric, neck, and head fractures.8 Collectively they are often referred to as hip fractures. They can be classified as intracapsular or extracapsular. In the older adult, a femoral neck fracture can occur with surprisingly little force owing to osteoporosis of the proximal femur. Femoral neck fractures in younger adults are almost always the result of high-impact forces, such as motor vehicle accidents. Femoral head fractures are associated with a posterior hip dislocation and acetabular fracture, although the fracture can occur in the absence of either of these conditions.23 Hip dislocations require urgent reduction because the vascular supply to the femoral head may be compromised.23 Management of hip dislocation without fracture includes closed reduction under conscious sedation and muscle relaxation followed by traction or open reduction if closed reduction fails. Rehabilitation includes functional mobility activities with weight-bearing limitations, exercise, and positioning per physician order based on hip joint stability and associated neurovascular injury. Hip dislocation with fracture warrants surgical repair. Intracapsular fractures are located within the hip joint capsule and include the femoral head, subcapital, and femoral neck regions. The four-stage Garden scale (Figure 5-5) is used to classify femoral neck fractures and is based on the amount of displacement and the degree of angulation. FIGURE 5-5 The Garden classification of femoral neck fractures. Grade I is an incomplete, impacted fracture in valgus malalignment (generally stable). Grade II is a nondisplaced fracture. Grade III is an incompletely displaced fracture in varus malalignment. Grade IV is a completely displaced fracture with no engagement of the two fragments. The compression trabeculae in the femoral head line up with the trabeculae on the acetabular side. Displacement is generally more evident on the lateral view in grade IV. For prognostic purposes, these groupings can be lumped into nondisplaced/impacted (grades I and II) and displaced (grades III and IV) because the risk of nonunion and aseptic necrosis is similar within these grouped stages. (From Browner BD, Jupiter JB, Levine AM et al: Skeletal trauma: basic science, management, and reconstruction, ed 4, Philadelphia, 2009, Saunders.) • Garden stage I fractures are impacted and incomplete. • Garden stage II fractures are complete and nondisplaced. • Garden stage III fractures are complete and partially displaced. Femoral neck fractures require reduction and internal fixation, often through the use of cannulated screws.23,24 In the older adult who has a displaced femoral neck fracture, some surgeons may elect to use a prosthetic replacement of the femoral head (hemiarthroplasty) in order to minimize the development of osteonecrosis or nonunion.23,24 Extracapsular fractures occur outside of the hip joint capsule. They can be further classified as intertrochanteric or subtrochanteric. Intertrochanteric fractures occur between the greater and lesser trochanters. Subtrochanteric fractures occur below the lesser trochanter and end at a point 5 cm distally.25 Intertrochanteric and subtrochanteric fractures are shown in Figure 5-6. Extracapsular fractures are typically stabilized via open reduction and internal fixation through the use of a sliding hip screw or intramedullary nail.26 Mobility and gait training focuses on ensuring protected weight bearing. Active or assisted hip ROM and strengthening exercises should be initiated to foster an early restoration of function. Fractures of the femoral shaft typically result from high-energy trauma and are associated with concurrent injuries to the pelvis and ipsilateral lower extremity.27 Femoral shaft fractures can be accompanied by life-threatening systemic complications, such as hypovolemia, shock, or fat emboli. There also can be significant bleeding into the thigh with hematoma formation. Femoral shaft fractures can be classified based on their location (e.g., proximal, middle, and distal third) and through descriptive terms (Figure 5-7). In the presence of contamination or hemodynamic instability, external fixation or skeletal traction may be applied temporarily.28 For most surgeons, the treatment of choice is the use of an intramedullary nail.27 After intramedullary nailing, the patient should avoid rotation of and pivoting on the lower extremity, because microrotation of the intramedullary rod can occur and place stress on the fixation device. Initially, weight bearing is limited to touchdown weight bearing. Active and assisted ROM of the hip, quadriceps setting, straight-leg raises, and hip abduction exercises should be initiated. FIGURE 5-7 Femur fracture patterns. A, Transverse. B, Oblique. C, Spiral. D, Butterfly fragment (arrow). E, Comminuted. F, Segmental. (From Townsend CM, Beauchamp D, Evers M, Mattox KL: Sabiston textbook of surgery, ed 19, Philadelphia, 2012, Saunders.) Fractures of the distal femur are classified by the OTA classification system as extra-articular (type A), partial articular (type B), or complete articular (type C).8 Involvement of the articular surface of the knee joint complicates the fracture. Typically, this type of fracture is caused by high-energy impact to the femur, especially in younger patients, or a direct force that drives the tibia cranially into the intercondylar fossa. Distal femur fractures may be accompanied by injury to localized skin, muscle, and joint ligaments and cartilage with the potential for decreased knee joint mechanics.29 A patella fracture results from direct trauma to the patella from a fall, blow, or motor vehicle accident (e.g., dashboard injury) or indirect mechanisms from a forceful contraction of the quadriceps with the knee flexed.30 Injury to the patella may lead to alterations in the articular surface of the patellofemoral joint and abnormal extensor mechanism mechanics. Late complications include patellofemoral or hardware pain, osteoarthritis, decreased terminal extension, quadriceps weakness, or adhesions.30 Nonsurgical management through immobilizing the knee in extension via a cast or brace may be chosen for nondisplaced fractures or patients with significant medical cormorbidities.31 Surgical treatment includes reduction and internal fixation, with a partial or total patellectomy reserved for highly comminuted fractures. Postoperatively, the knee is immobilized, and quadriceps setting exercises are initiated. Strong, forceful quadriceps contractions and straight-leg raises should be avoided. Protected weight bearing should ensue, abiding by the weight-bearing limitations prescribed by the physician. Tibial plateau fractures typically result from direct force on the proximal tibia (e.g., when a pedestrian is hit by an automobile) and are considered extra-articular, partial articular, or complete articular.8 The Schatzker classification system is commonly used with displaced fractures (Figure 5-8). This high-force injury often presents with open wounds and soft-tissue injuries, including capsular, ligamentous, and meniscal disruption. Immediate or early complications of tibial plateau fractures include popliteal or peroneal nerve compression, compartment syndrome, infection, and DVT.27 Late complications include abnormal patellofemoral mechanics, lack of ROM or stability, and posttraumatic arthritis of the articular surface. Surgical management via internal or external fixation is used for fractures that are unstable or associated with ligamentous and articular disruption.27 The complexity of the tibial plateau fracture will dictate the precautions for movement and mobility after surgery. In most situations, no weight bearing will be allowed during the initial healing phases, and gentle active or active assisted knee ROM exercises may be delayed for several days postoperatively. FIGURE 5-8 Tibial plateau fractures: Schatzker classification system. In this system, the treatment is more difficult and the prognosis poorer with higher fracture types. Types I, II, and III fractures are low-energy injuries that often occur in older persons and involve the lateral tibial plateau. Types IV, V, and VI fractures are higher-energy injuries and are associated with fracture comminution and involvement of the medial aspect of the tibia or medial tibial plateau. Type I injuries may also occur in young persons and are characterized by a split or wedge fracture line, although the size of the wedge is variable. These fractures are commonly associated with lateral meniscal tears or entrapment. Type II fractures are characterized by a lateral split fragment with or without articular depression just medial to the split. Type III fractures are characterized by pure articular depression. Type IV fractures involve the medial tibial plateau and may be further subdivided into those that are split fractures (type IVA) and those that are depression injuries (type IVB). These fractures may extend to the lateral aspect of the midline. Type V fractures involve both tibial plateaus and are often designated bicondylar fractures. Type VI fractures extend inferiorly to involve the metaphysis and diaphysis of the tibia. (From Langford JR, Jacofsky DJ, Haidukewych: Tibial plateau fractures. In Insall JN, Scott WN, editors: Surgery of the knee, ed 5, New York, 2012, Churchill Livingstone, p 775.)
Musculoskeletal System
Preferred Practice Patterns
Examination
Patient History
Medical Record Review
Diagnostic Tests Review
Computed Tomography.
Magnetic Resonance Imaging.
Bone Scan.
Myelography.
Physical Therapy Implications
Medication Review
Patient Interview
Tests and Measures
Observation
Cardiovascular and Pulmonary.
Integumentary.
Sensation.
Pain.
Range of Motion and Strength.
Interventions
Health Conditions
Traumatic Fracture
Traumatic Fracture Classification
Clinical Goal of Fracture Management
Complications of Fracture
Fracture Management According to Body Region
Pelvis and Lower Extremity
Pelvic Fractures.
Acetabulum Fractures.
Proximal Femur Fractures.
Femoral Shaft Fractures.





Distal Femur Fractures.
Patella Fractures.
Tibial Plateau Fractures.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree