CHAPTER 28 Muscle Ruptures Affecting the Shoulder Girdle
Injury to muscle structures is exceedingly common, yet many of these injuries remain poorly described and ill-defined. Most injuries are not identified as the cause of significant long-term disability unless they involve complete disruption of the muscle or its attachments. Fortunately, this complication is much less common than when a rupture involves the tendon, such as in rotator cuff tears. Interference with function, particularly diminution of strength, has previously been the major means of confirming muscle injury, together with palpable deficiency or major atrophy of the muscle substance. The exact pathologic process, however, has seldom been defined because muscle strains and minor disruptions rarely require the surgical exposure that allows documentation of pathology. Computed tomography (CT) and magnetic resonance imaging (MRI) have provided methods of visualizing muscle injuries not hitherto possible. In the past, relatively few muscle injuries of the shoulder girdle have been described, whereas such injuries increasingly are described in published works and will undoubtedly be recorded more often and more precisely in the future.
Brickner and Milch1 described muscle ruptures as being caused by active contraction of a muscle, contraction of an antagonist, increase in tearing over cohesive power, asynchronous contraction, or the additional muscular force of another muscle. Basically, however, one may consider most significant muscle ruptures as occurring when an actively contracting muscle group is overloaded by the application of a resisting load or external force that exceeds tissue tolerance. When such overload occurs, the muscle fibers are torn and the muscle sheath is disrupted, thus leading to a palpable defect in the muscle.
A great many injuries to skeletal muscle can heal without the formation of functionally limiting scar tissue.2 In more severe muscle injuries or with re-ruptures, there can be excessive proliferation of fibroblasts, resulting in a dense scar that delays or restricts the regeneration of myofibers across the defect. As an additional problem, effective surgical repair of muscle injury is very challenging as well.
GENERAL PRINCIPLES OF RUPTURE OF THE MUSCULOTENDINOUS UNIT
The classic experiments performed by McMaster3 demonstrated the relative strength of a muscle, tendon, and bone preparation. He suspended the gastrocnemius of the amputated limb of an adult rabbit. A wire was passed through the femur, and increasing weight was attached to the os calcis until rupture occurred. Between 10 and 21 kg of weight, the unit ruptured. In the seven preparations successfully tested, rupture occurred at the insertion with associated bony avulsion in three cases; two ruptured at the origin, again with bony avulsion; and the others ruptured through either the muscle belly or the musculotendinous junction. McMaster could produce a rupture of the tendon midsubstance only after 50% of its substance had been divided. The normal tendon appears to be the strongest component of the musculotendinous unit, a finding that was confirmed by Cronkite.4
The site of rupture may be influenced by the rate of loading. In 1971, Welsh and coworkers,5 while testing a tendon-bone system in the rabbit, found that lower rates of loading were associated with rupture at the tendon-bone junction. At higher rates, the tendon broke at the site of clamping, and the strength of the tendon-bone junction was found to be more secure.
Similar studies have been undertaken in stimulated muscle.6 The energy absorbed by the muscle before disruption was twice as great with prestimulation. Indeed, Safran and associates7 have demonstrated experimentally that in rabbit muscle preconditioned with isometric stimu lation, more tension developed and a greater change in length was required before failure occurred.
Muscles that cross two joints are subject to stretch at each joint and are therefore more vulnerable to injury. Likewise, muscles with a higher percentage of type II fibers are also more susceptible.8
The mechanism of injury might well influence the site of rupture. For example, in rupture of the pectoralis major, McEntire and associates9 noted that direct trauma more commonly resulted in muscle belly rupture, whereas indirect trauma was more likely to produce rupture distally. Similarly, although rupture of the long head of the biceps is common and rupture at the insertion is well recognized, rupture of the biceps muscle belly is rare. Still, as many as 48 complete belly ruptures were described by Heckman and Levine10 in parachutists, in whom the injury was caused by direct trauma from the static line.
The role of anabolic steroids in predisposing to muscle rupture also bears consideration, especially in bodybuilding, weightlifting, and throwing athletes.11,12 In 1992, Miles and coworkers13 conducted experiments on 24 male rats in which anabolic steroids and exercise were used as variables. Biomechanical tests revealed stiffer tendons in the group of rats receiving stanozolol intramuscularly than in the rats that did not receive steroid injections. In addition, “The energy at the time when the tendon failed, the toe-limit elongation, and the elongation at the time of first failure were all affected significantly.”13 Examination via electron microscopy revealed alterations in the size of collagen fibrils in rats receiving stanozolol in comparison to the control group.
In a similar study, Wood and associates12 found that the crimp pattern of collagen was shorter and the angle between collagen fibrils longer in the tendons of rats treated with anabolic steroids. On the basis of the aforementioned results, it can be speculated that steroids play a role in altering both the structure and the pattern of collagen fibrils, in turn causing a stiffer and weaker musculotendinous junction that is more likely to rupture.
RUPTURE OF THE PECTORALIS MAJOR
Historical Review
Rupture of the pectoralis major, first described by Patissier14 in 1822, is generally described as a rare injury. In 1972, a comprehensive review of the literature by McEntire and associates9 revealed only 45 cases, to which they added 11 more. However, only 22 of the 56 patients had undergone surgical exploration, and 1 case of rupture was confirmed at autopsy. Thus, actual confirmation of the lesion was lacking in 33 patients, and cases of congenital absence of the pectoralis major may have been represented in this group. Since then, approximately 225 additional cases have been published in the literature, at least 125 of which have been confirmed surgically. With more than 55 cases noted in the literature since 2004, this injury might not be as unusual at previously thought.
Anatomy
The pectoralis major arises in a broad sheet as two distinct heads–an upper clavicular head and a lower sternocostal head–that spread to a complex trilaminar insertion along the lateral lip of the bicipital groove. A portion of the sternocostal head spirals on itself to produce the round appearance of the anterior axillary fold, with the result that the lowermost fibers are inserted most proximally on the humerus and in a crescent into the capsule of the shoulder joint. McEntire and associates9 attributed the infrequency of complete rupture of the pectoralis major to the layered form of the muscle and its complex insertion.
Classification
Pectoralis major ruptures may be classified according to the extent and site of the rupture.
Type 1 ruptures consist of a contusion or sprain.
Type 2 represents partial ruptures.
Partial tears are more common than complete tears, with partial tears usually occurring at the musculotendinous junction and complete tears tending to occur at the tendon-bone interface.9 Most cases are undoubtedly partial, but 90 of the 104 cases reported since 1972 that came to surgery were complete. In these reports the predominant lesion was avulsion from the humerus in 78 cases. Avulsion from the musculotendinous junction occurred in 17 cases, tendinous ruptures accounted for 3 cases, and only 2 cases involved rupture of the muscle itself.
Incidence and Mechanisms
Rupture of the pectoralis major muscle was believed to be rare, with only infrequent reports in the literature until the 1970s. McEntire and associates9 reviewed the literature in 1972 and concluded that the injury probably occurs much more often than reports would indicate. The approximately 225 cases that have been reported since the 1970s account for nearly 80% of the 280 cases reported in the literature. The problem has been reported almost exclusively in male patients; the female patients are elderly women in nursing homes. Although the injury has occurred in patients ranging in age from newborn to 97 years, most pectoralis ruptures occur in persons aged between 20 and 40 years.
Rupture of the pectoralis major follows extreme muscle tension or direct trauma, or a combination of both. Of the 56 cases reviewed by McEntire and associates,9 excessive muscle tension caused 37 injuries and direct trauma caused 9. A combination of the two mechanisms was the cause in 4 cases, and spontaneous rupture was reported in 3 instances. In the more recent literature, excess tension injury was the cause in approximately 218 patients, and direct injury occurred in 7 cases. The most common mechanism of injury has been associated with weight-lifting (41%), with approximately 30% of the injuries resulting from bench pressing. Injuries arising from the bench press accounted for 4 of 9 cases reported by Zeman and associates,15 9 of 19 cases reported by Kretzler and Richardson,16 9 of 15 patients recorded by Connell,17 and 10 of 17 cases examined by Schepsis and coworkers.18 Other activities where injuries have resulted in pectoralis major muscle tears include rugby, snow boarding, and water skiing.19,20 Another common mechanism of injury occurs when a person attempts to break a fall and severe force is applied to a maximally contracted pectoralis major muscle.
There have been recent reports of pectoralis major ruptures in the elderly.21–23 These injuries occurred during common nursing procedures such as positioning or transfers and manifested with large pectoral ecchymosis and severe pain. The patients were well served with nonsurgical management, but the articles highlight problems associated with pain management and blood loss in this elderly population. The mean decline in hemoglobin level was 2.6 g/dL, at times resulting in hemodynamic instability and the need for blood transfusions.
Wolfe and associates,24 supported by cadaver and clinical studies, provided an explanation for the high rate of injury with bench pressing. Their patients described the rupture occurring when the bar is at its lowest point with the shoulders extended to 30 degrees, during the eccentric phase of contraction. At this point the fibers of the lowest portion of the sternal head become disproportionately stretched. Elliot and associates25 showed by electromyographic studies that the pectoralis major muscle is maximally activated at the initiation of the lift with the humerus in the extended position. Wolfe and associates24 state that the application of maximal load to inferior fibers stretched to an extreme mechanical disadvantage produces rupture of these fibers. Continued loading then increases the tension on the remaining fibers of the sternal head, which fail. This explanation might account for the increased incidence of rupture of the sternal head during weightlifting.
Clinical Findings
The physical findings depend on the site of rupture. If the muscle is injured in its proximal portion, the swelling and ecchymosis are usually noted on the anterior part of the chest wall on the involved side. The muscle belly retracts toward the axillary fold and causes a prominent bulge. Rupture in the distal portion can cause swelling and ecchymosis in both the arm and the chest; the body of the muscle bulges on the chest, and such bulging causes the axillary fold to become thin (Fig. 28-1). The shoulder is tender at the site of rupture, and a visible or palpable defect is usually present.

FIGURE 28-1 Rupture of the pectoralis major in a 30-year-old weight lifter.
(Courtesy of J. J. Brownlee, MD.)
Zeman and coworkers15 described one patient in whom the tendon felt intact through to its humeral insertion. At surgery, however, a complete tear was found at the musculotendinous junction (Fig. 28-2), with an overlying fascial layer giving the impression of an intact tendon. These authors cautioned that the lack of a palpable defect in the axilla is not a reliable sign of continuity of the pectoralis major muscle.
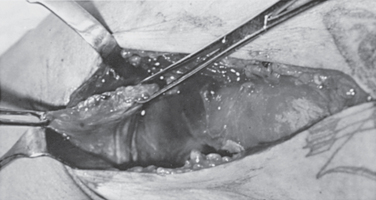
FIGURE 28-2 Findings at surgery in the patient shown in Figure 28-1. The pectoralis major tendon is avulsed from its humeral insertion (right).
Radiographic and Laboratory Evaluation
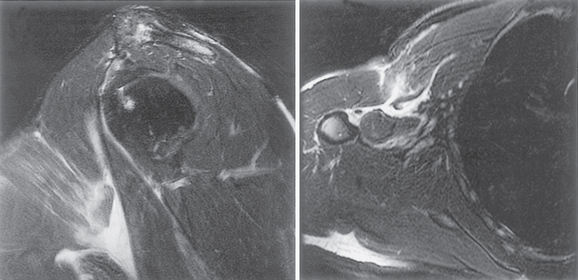
Radiographs generally fail to reveal any bone abnormality, but loss of the normal pectoralis major shadow has been described as a reliable sign of rupture. Soft tissue shadowing is visible when a significant hematoma is present, whereas ultrasound may be useful when confirming the site of rupture. Some reports suggest that MRI is superior to CT and should be the modality of choice for assessment of pectoralis major injury.17 It has been suggested that MRI can be used to distinguish partial tears from complete tears and acute tears from chronic tears.17 Acute tears demonstrate hemorrhage and edema (Fig. 28-3), whereas chronic tears demonstrate fibrosis and scarring on MRI.17 MRI may be used to monitor interval healing when patients are treated conservatively and to evaluate muscle quality before return to competitive sports.
Complications
The most sinister documented complication of pectoralis major rupture is sepsis involving the associated hematoma. Noted in three reported cases,14,27,28 sepsis directly caused the death of one patient and led to the death of a second from pneumonia. A patient described by Pai and Simison28 was remarkable in having a temperature of only 37.5 °C and a white blood cell count of 11,500/cm3 despite 1500 mL of frank purulence being drained. β-Hemolytic streptococci were cultured.
Pseudocyst formation in a hematoma has been described by Ronchetti,29 and associated neuromuscular injuries have also been reported. Kawashima and associates30 described a patient with a crush injury with total rupture of the pectoralis major at the musculotendinous junction and hypesthesia of the C6-C8 and T1 dermatomes of the affected extremity. Several associated muscle injuries have also been described, including rupture of the anteromedial portion of the adjacent deltoid, pectoralis minor rupture, and rotator cuff tears. Additional injuries in one patient included a fractured humerus and open fractures of both forearm bones. Purnell31 described myositis ossificans in a patient seen 4 months after rupture, and Smith32 reported the development of rhabdomyosarcoma 10 years after rupture of the pectoralis major at the same site.
Treatment
Methods
Partial rupture of the pectoralis major or lesions of the muscle belly respond to conservative treatment with initial icing and rest to control the hematoma. The early application of heat and ultrasound and a program of shoulder-mobilizing exercises (both passive and active assisted) help restore shoulder function. Unresisted stretching exercises should be included early in the rehabilitation program, but resisted strengthening should await a 6-week recovery with restoration of good shoulder mobility and settling of all pain.
Surgical Treatment
Complete rupture of the pectoralis major demands early surgical treatment in an active athlete. The results of late repair, although they may be satisfactory, are not as good as when primary repair is undertaken.33
Tendinous avulsion can be repaired by anatomic reattachment with heavy sutures through drill holes in the humeral cortex. For situations in which some tendon remains attached to the humerus, Orava and coworkers34 described an effective method of treatment by end-to-end repair of the tendons and reinforcement of the repair with retention sutures into bone.
Chronic tears have been reconstructed with techniques including the use of Achilles tendon allograft,35 fascia lata allograft,36 and bone–patellar tendon autograft.37 Outcome measures are not reported for these cases, but all patients appear to have returned to their prior activities without restriction and had no reported functional impairment.
Results of Treatment
In 1970, Park and Espiniella38 reviewed 31 patients reported in the literature. Surgical treatment produced an excellent result in 80% of patients, and 10% had good results. This outcome compared most favorably with the good results reported in only 58% of patients who were treated nonoperatively. These authors stated that in the nonoperative group, varying degrees of weakness of adduction and internal rotation were present. Over time, however, the teres major, subscapularis, deltoid, and latissimus dorsi slowly take over the function of the pectoralis major. Three cases were reported of wrestlers returning to successful careers after nonoperative treatment.
Gudmundsson39 reported that normal power is rarely achieved in these instances. Zeman and colleagues15 described nine athletes who had rupture of the pectoralis major. Surgical treatment was undertaken in four cases; all patients had excellent results. In the five patients treated nonoperatively, residual weakness was present in all cases; one professional boxer could not return to boxing, and two weightlifters had good results but were not entirely happy because of persistent weakness.
Kretzler and Richardson16 undertook repair in 16 of 19 patients, and 13 patients reported full return of strength. This study included 2 patients who underwent repair as late as 5.5 years after the injury. Although full strength was not achieved in these patients, significant improvement was reported. One patient demonstrated improvement in horizontal adduction strength from 50% to 80% and the other demonstrated similar adduction strength improvement from 60% to 84%. The authors indicated that with diligent freeing of adhesions and firm fixation to the humerus, late repair is worthwhile.
Scott and associates40 recommended conservative treatment on the basis that late repair is possible in patients in whom dynamometry indicates persistent weakness. Yet they indicated that all four patients tested by dynamometry, one of whom underwent repair, had complete rupture of just the sternocostal head and that these injuries would be expected to perform better than those with total rupture.
Wolfe and colleagues24 tested six patients who had chronic tears, including four with complete tears. In the four patients with complete tears, the peak torque in horizontal adduction was 74% of the normal side, and performance on repetitive testing showed 60% of the normal side at low speed and 76% of the normal side at high speed. Late repair yielded satisfactory results. The authors recommend acute repair for complete tears in patients who require their upper extremity for high-tension activities or sports.
Jones and Matthews41 classified the outcomes in the literature into one of three grades, depending on range of motion, power, and pain. If the results of those who had surgery within 1 week of injury are compared with those of a combined group of patients who had delayed or no surgery, the results of early surgery are much better (P < .001).
Hanna and associates19 examined 22 patients with complete tears of the pectoralis major by objective strength and subjective functional outcome measures. Injuries sustained in athletic activities were the mechanism in 19 of the 22 cases: 10 patients treated by surgical repair were compared with 12 patients treated nonoperatively. In the group treated surgically, the injured arm regained an average of 99% and 97% of the strength of the uninjured arm as assessed by dynamometer testing of peak torque and work, respectively, whereas patients treated nonsurgically regained 56% of the strength of the uninjured arm. Only 1 patient who did not undergo repair returned to full function.
Schepsis and associates18 reported on 17 patients with pectoralis major injuries; 4 were treated nonoperatively and 13 were treated with surgery. They found an overall satisfaction rating of 96% in the acute surgical group, 93% in the chronic surgical group, and 51% in the nonoperative group. On isokinetic testing, adduction strength was found to be 102% of the opposite side in the acute surgical group, 94% in the chronic surgical group, and 71% in the nonoperative group. They concluded that there were no significant differences in outcome between patients treated operatively for acute or chronic injuries but that surgically treated patients fared significantly better than patients treated nonoperatively.
In a meta-analysis of 112 cases of pectoralis major rupture, Bak and colleagues42 calculated 88% excellent or good results for patients treated surgically versus 27% for patients treated conservatively. They also found that significantly more patients had an excellent outcome when surgery was performed within 8 weeks of the injury than when surgery was delayed. They concluded that surgical treatment, preferably within the first 8 weeks after the injury, has a significantly better outcome than conservative treatment or delayed repair does.
RUPTURE OF THE DELTOID
Historical Review
Rupture of the deltoid was first described by Clemens26 in 1913 in a railway worker, and reports in the literature have been sparse since then. In 1919, Davis33 reported one case in which the deltoid became detached after suppuration of its bony origin as a result of osteomyelitis of the clavicle. Gilcreest and Albi43 described two further cases in 1939. In 1972, McEntire and coworkers9 reported a case associated with rupture of the pectoralis major. In 1975, Samuel and associates44 described a single case, and in 1976, Pointud and colleagues45 described a further case, both reported in the French literature. Both patients had received multiple injections of steroids: in the first case, 18 injections for a frozen shoulder, and in the second case, approximately 12 per year for several years in association with a rotator cuff tear. In the latter case, the patient also received radiotherapy, and this treatment, combined with injections of steroids in direct contact with the deltoid, resulted in disruption of the middle third of the deltoid. Management was conservative.
Panting and Hunter46 reported two deltoid ruptures in elderly patients in 1983, and Morisawa and associates47 reported two instances of deltoid muscle rupture associated with rotator cuff tears. One patient was 71 years old and the other was 80 years old; neither had an associated traumatic injury, although one did have repeated hydrocortisone injections. One patient was treated surgically with resection of the thinned portion and a side-to-side repair and achieved excellent motion at 3 months. In their review, Morisawa and associates47 noted that most of the patients had sclerotic changes and an osteophyte at the greater tuberosity and postulated that upward migration of the humeral head in the presence of a massive rotator cuff tear combined with an osteophyte on the greater tuberosity might cause repeated friction and degeneration of the deltoid.
An additional report of a posterior deltoid tear was added by Lin48 in which she described a 75-year-old woman who had neither prior trauma nor a hydrocortisone injection. Her potential risk factors for the injury were the avid pursuit of golf and Pilates. She returned to normal strength and activity after 6 weeks of conservative treatment with physical therapy and anti-inflammatory medications.
In 2002, Allen and Drakos49 described a 31-year-old professional cricket player (fast bowler) who suffered partial detachment of the deltoid muscle without concomitant rotator cuff injury. This appears to be the first report of deltoid muscle detachment without an associated rotator cuff tear. The authors suggested that the windmill action of the bowling motion places significant force on the deltoid muscle and can lead to partial detachment of the deltoid muscle. The patient did well with conservative management.
The literature does not abound with reports of deltoid rupture. Indeed, the rarity of this type of injury was exemplified in the Mayo Clinic series of 1014 cases of musculotendinous rupture described by Anzel and colleagues50 in which no cases were unveiled.
Mechanism
Complete traumatic disruption of the deltoid, as the literature reviewed indicates, is rare. Indeed, the trauma to the deltoid most commonly seen in clinical practice is associated with misguided shoulder surgery, particularly if the deltoid is detached from the acromion and becomes dehiscent. The posterior approach to the shoulder, in which the deltoid is released from the spine of the scapula, is a major culprit in this regard.
Methods of Treatment
Delay in repair with associated retraction and scarring makes the situation even more difficult. In 1919, Davis33 first reported the management of a chronic defect of the anterior deltoid with a broad graft of fascia from the thigh. He recommended retaining a thick layer of subcutaneous fat to prevent the formation of adhesions between the rotator cuff and the fascial implant. Clearly, late salvage of this injury is not satisfactory; if deltoid ruptures are to be dealt with satisfactorily, early identification and prompt surgical repair are critical.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree