Multiple Trauma
INTRODUCTION
High-velocity trauma is the number one cause of death in the 18- to 44-year-old age group worldwide.
The cost to the healthcare system for blunt trauma is greater than any other disease.
There is no consensus definition, but the polytrauma patient can be defined as follows:
Injury severity score (ISS) >18
Hemodynamic instability or coagulopathy present on admission
More than one system involvement: central nervous system (CNS), pulmonary, abdominal, musculoskeletal, etc.
FIELD TRIAGE
Management Priorities
Assessment and establishment of airway and ventilation
Assessment of circulation and perfusion
Hemorrhage control
Patient extrication
Shock management
Fracture stabilization
Patient transport
TRAUMA DEATHS
Trauma deaths tend to occur in three phases:
Immediate: This is usually the result of severe brain injury or disruption of the heart, aorta, or large vessels. It is amenable to public health measures and education, such as the use of safety helmets and passenger restraints.
Early: This occurs minutes to a few hours after injury, usually as a result of intracranial bleeding, hemopneumothorax, splenic rupture,
liver laceration, or multiple injuries with significant blood loss. These represent correctable injuries for which immediate, coordinated, definitive care at a level I trauma center is most beneficial.
Late: This occurs days to weeks after injury and is related to sepsis, embolus, or multiple organ failure.
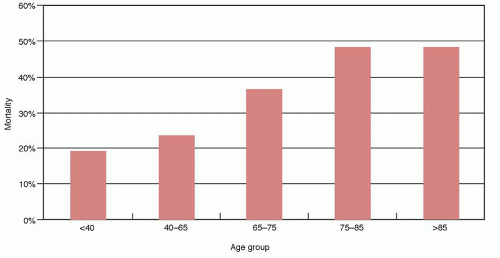
Mortality increases with increasing patient age (Fig. 2.1).
GOLDEN HOUR
Rapid transport of the severely injured patient to a trauma center is essential for appropriate assessment and treatment.
The patient’s chance of survival diminishes rapidly after 1 hour, with a threefold increase in mortality for every 30 minutes of elapsed time without care in the severely, multiply injured patient.
THE TEAM
The trauma team is headed by the trauma general surgeon, who acts as the “captain of the ship” in prioritizing and directing patient care.
The orthopaedic consult is available to assess all musculoskeletal injuries, provide initial bony stabilization, and work in concert with the trauma general surgeons to treat shock and hemorrhage.
RESUSCITATION
Follows ABCDE: airway, breathing, circulation, disability, exposure
AIRWAY CONTROL
The upper airway should be inspected to ensure patency.
Foreign objects should be removed and secretions suctioned.
A nasal, endotracheal, or nasotracheal airway should be established as needed. A tracheostomy may be necessary.
The patient should be managed as if a cervical spine injury were present. However, no patient should die from lack of an airway because of concern over a possible cervical spine injury. Gentle maneuvers, such as axial traction, are usually possible to allow for safe intubation without neurologic compromise.
BREATHING
This involves evaluation of ventilation (breathing) and oxygenation.
The most common reasons for ineffective ventilation after establishment of an airway include malposition of the endotracheal tube, pneumothorax, and hemothorax.
Tension pneumothorax
Diagnosis: tracheal deviation, unilateral absent breath sounds, tympany, and distended neck veins
Treatment: insertion of a large-bore needle into the second intercostal space at the midclavicular line to allow immediate decompression, then placement of a chest tube
Open pneumothorax
Diagnosis: sucking chest wound
Treatment: occlusive dressing not taped on one side to allow air to escape, followed by surgical wound closure and a chest tube
Flail chest with pulmonary contusion
Diagnosis: paradoxical movement of the chest wall with ventilation
Treatment: fluid resuscitation (beware of overhydration), intubation, positive end-expiratory pressure may be necessary
Endotracheal tube malposition
Diagnosis: malposition evident on chest radiograph, unilateral breath sounds, asymmetric chest excursion
Treatment: adjustment of the endotracheal tube with or without reintubation
Hemothorax
Diagnosis: opacity on chest radiograph, diminished/absent breath sounds
Treatment: chest tube placement
Indications for intubation
Loss (or anticipated loss) of airway control
Prevention of aspiration in an unconscious patient
Hyperventilation for increased intracranial pressure
Obstruction from facial trauma and edema
CIRCULATION
Hemodynamic stability is defined as normal vital signs (blood pressure, heart rate) that are maintained with only maintenance fluid volumes.
In trauma patients, shock is hemorrhagic until proven otherwise.
At a minimum, two large-bore intravenous lines should be placed in the antecubital fossae or groin with avoidance of injured extremities. Alternatively, saphenous vein cutdowns may be used in adults or intraosseous (tibia) infusion for children <6 years of age.
Serial monitoring of blood pressure and urine output is necessary, with possible central access for central venous monitoring or Swan-Ganz catheter placement for hemodynamic instability. Serial hematocrit monitoring should be undertaken until hemodynamic stability is documented.
Peripheral blood pressure should be assessed.
Blood pressure is necessary to palpate a peripheral pulse.
|
INITIAL MANAGEMENT OF THE PATIENT IN SHOCK
Direct control of obvious bleeding: direct pressure control preferable to tourniquets or blind clamping of vessels
Large-bore venous access, fluid resuscitation (normal saline or Ringer’s lactate), monitoring of urine output, central venous pressure, and pH
Blood replacement as indicated by serial hematocrit monitoring
Traction with Thomas splints or extremity splints to limit hemorrhage from unstable fractures
Consideration of angiography (with or without embolization) or immediate operative intervention for hemorrhage control
DIFFERENTIAL DIAGNOSIS OF HYPOTENSION IN TRAUMA
Cardiogenic Shock
Cardiac arrhythmias, myocardial damage
Pericardial tamponade
Diagnosis: distended neck veins, hypotension, muffled heart sounds (Beck triad)
Treatment: pericardiocentesis through subxiphoid approach
Neurogenic Shock
This occurs in patients with a thoracic level spinal cord injury in which sympathetic disruption results in an inability to maintain vascular tone.
Diagnosis: Hypotension without tachycardia or vasoconstriction. Consider in a head-injured or spinal cord-injured patient who does not respond to fluid resuscitation.
Treatment: Volume restoration followed by vasoactive drugs (beware of fluid overload).
Septic Shock
Consider in patients with gas gangrene, missed open injuries, and contaminated wounds closed primarily.
Diagnosis: Hypotension accompanied by fever, tachycardia, cool skin, and multiorgan failure. This occurs in the early-to-late phases, but not in the acute presentation.
Treatment: fluid balance, vasoactive drugs, antibiotics.
Hemorrhagic Shock
More than 90% of patients are in acute shock after trauma.
Consider in patients with large open wounds, active bleeding, pelvic and/or femoral fractures, and abdominal or thoracic trauma.
Diagnosis: Hypotension, tachycardia. In the absence of open hemorrhage, bleeding into voluminous spaces (chest, abdomen, pelvis, thigh) must be ruled out. This may require diagnostic peritoneal lavage (DPL), Focused Assessment with Sonography for Trauma (FAST) angiography, computed tomography (CT), magnetic resonance imaging (MRI), or other techniques as dictated by the patient presentation.
Treatment: Aggressive fluid resuscitation, blood replacement, angiographic embolization, operative intervention, fracture stabilization, and other techniques as dictated by the source of hemorrhage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree